CASE PRESENTATION
A 58-year-old man is referred for a refractive surgery evaluation. The patient has no significant ocular history and has never undergone eye surgery. He began wearing glasses at a young age and desires spectacle independence.
On examination, the patient’s uncorrected distance visual acuity is 20/100 OD and 20/80-1 OS. His BCVA is 20/20 OU with a manifest refraction of -3.00 +4.00 x 010º OD and -2.00 +3.50 x 010º OS. His current spectacle prescription is -2.50 +4.00 x 010º OD and -1.75 +3.50 x 010º OS. His Brightness Acuity Test is 20/30 OU.
The patient is happy with the quality of his BSCVA. He has never worn contact lenses. He reports no problems with driving at night or recent changes in his manifest refraction.
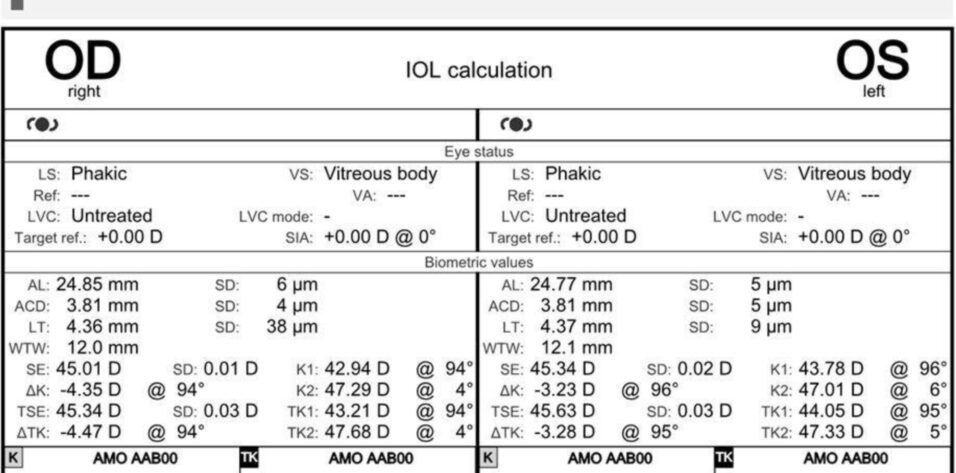
A slit-lamp examination finds mild corneal steepening and thinning just inferior to the corneal apex and a 1+ nuclear sclerotic cataract in each eye. The anterior segment of each eye is otherwise unremarkable. A fundus examination of both eyes is within normal limits, and the findings are confirmed with macular OCT imaging. Both eyes have a posterior vitreous detachment. Figures 1 and 2 present the biometry and corneal topography measurements, respectively.
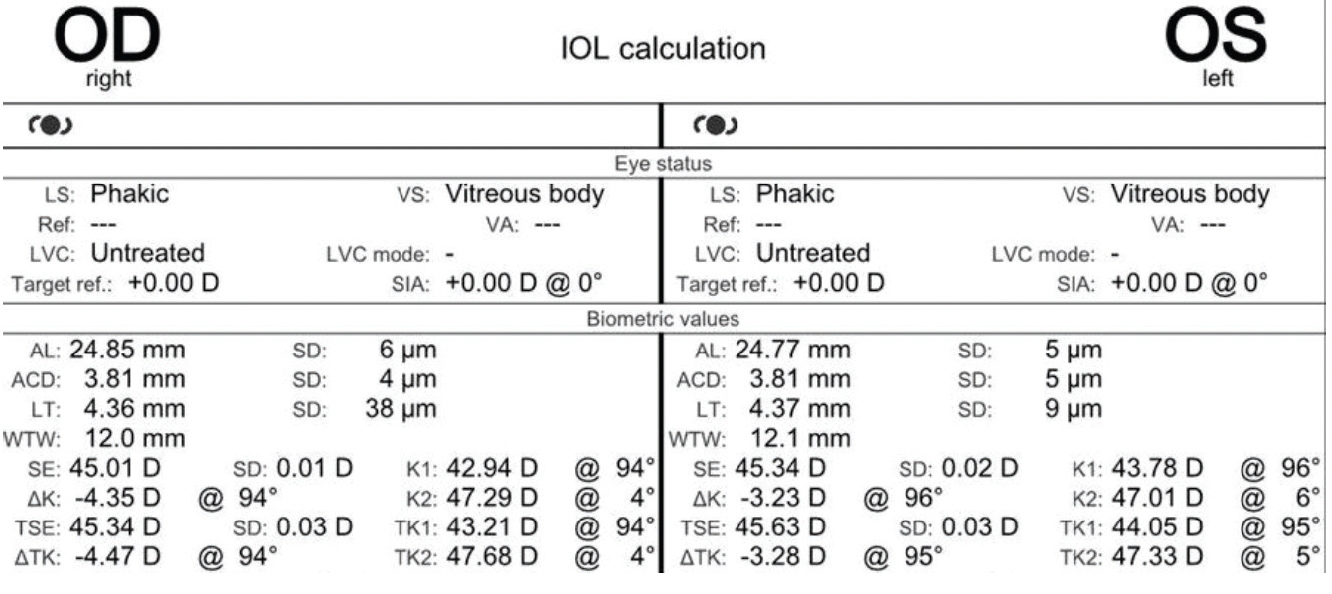
Figure 1. Biometry measurements of both eyes with the IOLMaster 700 (Carl Zeiss Meditec).
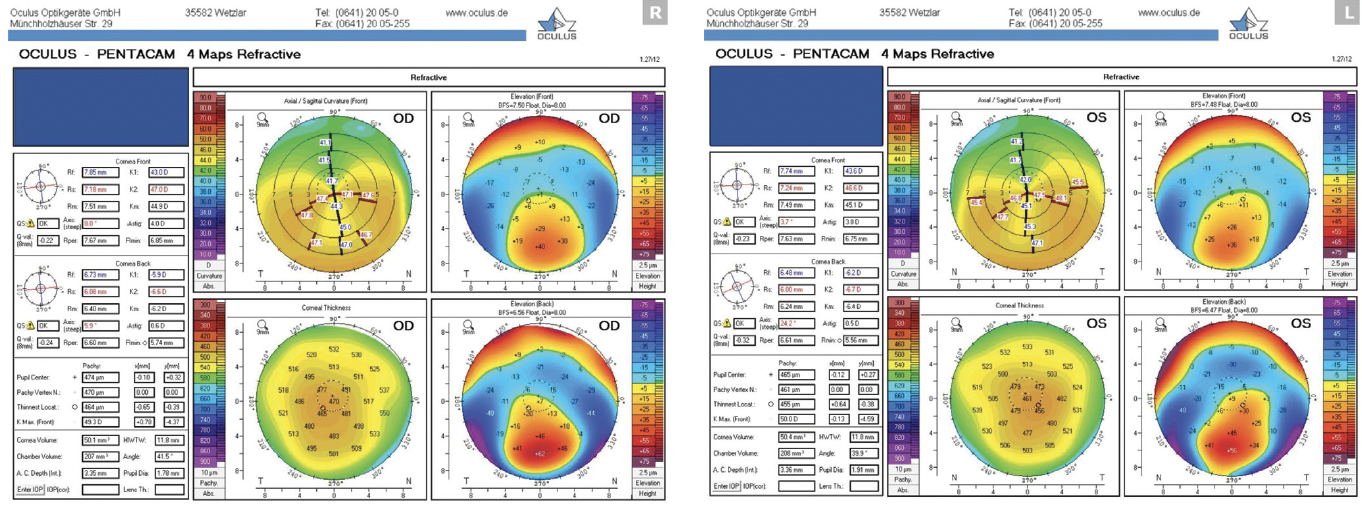
Figure 2. Corneal topography of both eyes with the Pentacam (Oculus Optikgeräte).
How would you proceed?
—Case prepared by Priya M. Mathews, MD, MPH

KANIKA AGARWAL, MD
The patient appears to have keratoconus, which precludes conventional laser vision correction and refractive lens exchange (RLE) with multifocal IOLs.
I would recommend a monovision trial with contact lenses and advise him that specialty lenses may be required. If the patient can tolerate contact lenses, I would counsel him against surgical intervention and explain that regular observation for corneal ectasia progression is necessary.
If the patient is contact lens intolerant or corneal ectasia progression is detected, he would be evaluated for an off-label, staged surgical procedure, specifically CXL using the Athens protocol followed by topography-guided PRK after his refraction stabilizes. This strategy could regularize the cornea, facilitate a successful contact lens fitting, and improve his quality of vision. Hyperopic topography-guided PRK is not available in the United States, where I practice.
Preoperative imaging with the WaveLight Vario Topolyzer (Alcon) would be assessed to determine how much tissue would be removed during treatment. The amount must be conservative (residual stromal bed > 400 µm) given the preexisting ectasia.
I would hesitate to offer RLE as an alternative because the procedure is unlikely to provide the patient with spectacle independence. The corneal irregularity is a contraindication for multifocal IOLs and increases the risk of a refractive surprise. If lens-based surgery is elected, a monofocal toric IOL would be selected for the right eye, and either the same lens type or a Light Adjustable Lens (LAL; RxSight) would be implanted in the left. Undercorrection of the nondominant eye is an option to reduce his dependence on spectacles if the patient tolerates monovision in a contact lens trial.
Before any form of surgical intervention is pursued, serial refraction and topography would be performed to confirm disease stability. Preoperative counseling would be extensive to ensure that the patient understands the goals of surgery and manage his expectations.

FRANCIS W. PRICE JR, MD
The patient desires spectacle independence, presumably at distance and near. It is important to set realistic expectations because his BSCVA is currently 20/20 OU. Based on the tomography and biometry measurements provided, he has 4.00 D of astigmatism in the right eye and 3.00 D in the left. The spherical equivalent refraction is not in the range of an EVO ICL (STAAR Surgical), eliminating the options of a monovision or blended vision strategy with phakic IOLs. Laser refractive surgery is not an option because of his keratoconus.
Any attempt to provide good uncorrected vision at near, far, and possibly intermediate distance would require an RLE. A challenge is that the correction of sphere and cylinder with lens-based surgery in keratoconic eyes is unpredictable, especially when the cone is displaced from the center of the cornea. The amount of cylinder is too high to expect complete resolution with an LAL, especially if the sphere ultimately must be corrected as well.
My colleagues and I recently reported the results of staged surgery on keratoconic eyes with cataracts.1 A spherical IOL was implanted with a target refraction of -2.00 D. After the refraction stabilized, patients who achieved acceptable visual acuity with manifest refraction were given the option of undergoing RLE.
We found that a staged approach offered two advantages. First, if manifest refraction could not achieve acceptable visual acuity, then patients could be fit for a contact lens without the challenge of a toric IOL in situ. Second, both the sphere and cylinder could be fine-tuned based on the postoperative refraction. Patients’ UCVA was 1 line better after the staged procedure compared to primary toric IOL placement.
Given that keratoconus increases higher-order aberrations, I would advise the patient against a multifocal or extended depth of focus IOL. One alternative would be a monovision or blended vision strategy with a standard monofocal IOL or monofocal plus lens such as the Tecnis Eyhance (Johnson & Johnson Vision) in one or both eyes. A second option would be to implant an IC-8 Apthera (Bausch + Lomb) in one eye.
The patient may be difficult to satisfy because his current BSCVA is 20/20 OU. In the right eye, the incision would be placed on the axis of astigmatism to decrease the cylinder. The same approach would be used in the left eye if implantation of an IC-8 lens is planned. A trial with lenses simulating a targeted monovision or blended vision result, while not perfect, would give him an idea of that form of visual correction and his level of comfort with it. A retina consultation would help with informed consent.

WHAT I DID: PRIYA M. MATHEWS, MD, MPH
The patient had underlying corneal ectasia, specifically keratoconus, in both eyes. He was aware of his high astigmatism but not his corneal disease. Based on my experience, subtle corneal irregularities and disease are underdiagnosed in patients whose visual acuity objectively corrects to 20/20. As this case illustrates, it is important to include corneal topography in the evaluation of any individual for refractive surgery, whether corneal or lens based.
The patient had experienced a mild myopic shift, but his glasses prescription remained stable. His BCVA was 20/20 OU, and he was happy with the quality of his BSCVA—something I inquire about when evaluating anyone who has irregular astigmatism for refractive surgery. Someone who must wear hard contact lenses to achieve an acceptable quality of vision is not a suitable candidate for an advanced technology IOL.
The patient desired the greatest degree of spectacle independence possible. Corneal irregularity ruled out laser vision correction. Early cataracts and posterior vitreous detachments, however, made him a candidate for bilateral RLE. We discussed the procedure and his IOL options at length. I explained that the irregularity of his corneas made a diffractive multifocal IOL a poor choice and discussed his other options:
- Option No. 1: A toric monofocal IOL. The amount and axis of astigmatism in each eye were similar on biometry and corneal topography. The probability of a residual refractive error after RLE was high, however, so the patient’s ineligibility for a postoperative refractive enhancement was a concern.
- Option No. 2: An LAL. I explained to the patient that, although the implantation of an LAL allows for postoperative refractive adjustments, the Light Delivery Device might be unable to correct his residual refractive error fully, particularly in the right eye, which had greater than 4.00 D of corneal astigmatism.
The patient elected to receive an LAL in each eye with the understanding that he might need to wear glasses to see at all distances. As expected, his residual refractive errors after RLE were significant before the light adjustments; his manifest refraction was +1.75 -4.50 x 100º OD and +0.25 -3.25 x 102º OS.
Four light adjustments and two lock-in treatments were performed (a total of six treatments with the fourth adjustment off-label) to address the patient’s refractive error. At the final visit, his UCVA was 20/20-2 and J2 OD and 20/20-1 and J2 OS. His BCVA was 20/15 OD with a manifest refraction of -0.25 -1.00 x 090º and 20/15 OS with a manifest refraction of -0.25 -1.00 x 065º. Thankfully in this case, the patient’s subjective vision was the best it had ever been, and he achieved spectacle independence at all distances. In situations like this one, however, it is vital to set realistic expectations from the beginning.
1. Goebel GJ, Price MO, Price FW Jr. Staged toric IOL exchange in keratoconus patients after cataract surgery. Paper presented at: World Cornea Congress; September 28, 2022; Chicago, IL.