For most ophthalmic surgeons, the annual ASCRS meeting in May was a good time to rekindle the flame for innovation in ophthalmology. Specifically for me, the meeting gave me an opportunity to take a closer look at innovations in several eye care sectors that pertain to my practice, including microinvasive glaucoma surgery (MIGS), and it helped me to identify what’s hot now and what’s sure to be hot in the years ahead.
The most obvious hot topics in the MIGS sector are the introductions of the iStent inject (Glaukos) and the Hydrus Microstent (Ivantis). Other trends that have started to surface include combining MIGS procedures, which I like to call MIGS2 or MIGS on MIGS, and MIGS plus, a term I like to use for minimally invasive filtering procedures for glaucoma management.
A BREAKDOWN OF TOP TRENDS
Stenting. As evidenced by the interest in the iStent inject and the Hydrus Microstent, the focus in MIGS is turning toward stenting the trabecular meshwork as minimally invasively as possible. The advantage of this strategy is that one can leave as much of the ocular anatomy as possible in its normal physiologic state.
With devices like the iStent inject in particular, stenting has also become a more intuitive procedure compared to the first-generation device. The learning curves are now shorter, meaning more cataract surgeons may feel comfortable implanting these devices at the time of cataract surgery in patients with concomitant glaucoma.
Glaucoma treatment in pseudophakes. Another trend in MIGS is treating pseudophakic glaucoma patients. The number of glaucoma patients who have already had cataract surgery is on the rise, which is drawing the attention of a lot of companies. In the future, I anticipate an increase in the number of new MIGS products that are designed for routine maneuvers, for instance dilating Schlemm canal, in this patient population. The Kahook Dual Blade (New World Medical) and the Omni Glaucoma Treatment System (Sight Sciences) continue to gain widespread acceptance among many of my colleagues looking to perform pseudophakic MIGS.
MIGS2. As surgeons become more comfortable with MIGS, a third area that is gaining traction is the combination of multiple microinvasive procedures in one eye to maximize IOP lowering. One MIGS2 option is to combine viscodilation of Schlemm canal over 360º (iTrack, Ellex) with the implantation of two iStent Trabecular Micro-Bypass Stents (Glaukos, see Watch It Now). Another is to combine use of the Omni with placement of two iStent injects (see Watch It Now; Figure).
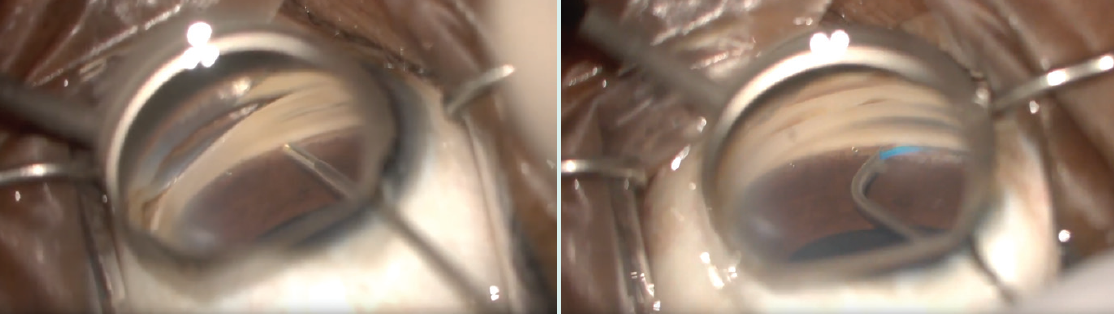
Figure. Placement of a second iStent inject during a MIGS2 procedure (left). The Omni device is threaded through Schlemm canal during the same MIGS2 procedure (right).
Combining multiple MIGS procedures in the same eye to target the outflow pathway, while already in the eye for cataract surgery, can be an especially useful strategy in patients who have more moderate to advanced primary open-angle glaucoma and are in need of a greater reduction of IOP than can be provided by a single MIGS procedure.
MIGS plus. A lot of people are getting excited about the MiniJect supraciliary device (iStar Medical). The soft, flexible, microporous stent is implanted in the supraciliary space, but a very small part of the device remains in the anterior chamber. In the company-sponsored first-in-human STAR-I study, patients achieved an average IOP reduction of 32.6%, to a mean of 15.6 mm Hg, at 1 year postoperative. Also at 1 year, 75% of patients were able to discontinue using topical medication, and corneal endothelial cell loss was minimal (mean change from baseline, -2%).1
What I like about this device is that it gives practitioners a chance to re-explore the supraciliary space after Alcon’s withdrawal of the CyPass Micro-Stent from the market. The iStent Supra (Glaukos) is also on the horizon, so at least two relevant devices may become available for this space.
The subconjunctival space. Let’s not forget about the subconjunctival space. In addition to the new ab externo approach to implanting the Xen Gel Stent (Allergan) that is becoming all the rage, the MicroShunt (Santen, distributed by Glaukos in the United States; not approved by the FDA) is designed for use in the subconjunctival space. Three-year data on the safety and efficacy of the MicroShunt have been published.2 In a single-site, prospective, nonrandomized study of 23 eyes in which maximum-tolerated glaucoma medication failed to control IOP, implantation of the MicroShunt achieved IOP control in the low teens (≤ 14 mm Hg) for up to 3 years. Device implantation was combined with cataract surgery in nine eyes.
Juan Batlle, MD, also recently presented promising data from a 2-year pooled analysis of the MicroShunt.3
WATCH IT NOW
Georges M. Durr, MD, FRCSC, presents a case of viscodilation of Schlemm canal using the iTrack device over 360º followed by the implantation of two trabecular microbypass stents.

Dr. Williamson presents a case of iStent inject combined with viscocanalostomy and ab interno trabeculotomy (Omni procedure).
Drug delivery. Last but not least, drug-eluting devices from Glaukos and Allergan are not too far from reality. Like many practitioners, I like to imagine a day when I will be able to place a drug-eluting device in combination with a MIGS procedure, thereby targeting the inflow and outflow pathways simultaneously.
CONCLUSION
Strategies combining MIGS procedures and combining procedures that target the inflow and outflow pathways are in their infancy, but I expect these practices to become common in the years to come.
In terms of what’s next, the MicroShunt and the MiniJect hold much promise for the MIGS space. Both may prove to be robust options for glaucoma management, and I especially look forward to getting back into the supraciliary space.
1. iSTAR Medical’s MINIject maintains exceptional results in first-in-human trial one year post-surgery (STAR-I). https://eyewire.news/articles/istar-medicals-miniject-maintains-exceptional-results-in-first-in-human-trial-one-year-post-surgery-star-i/. Accessed May 16, 2019.
2. Batlle JF, Fantes F, Riss I, et al. Three-year follow-up of a novel aqueous humor microshunt. J Glaucoma. 2016;25(2):58-65.
3. Batlle J. Two-year pooled analysis of the MicroShunt in patients with primary open-angle glaucoma. Paper presented at: ASCRS-ASOA Annual Meeting; May 3-7, 2019; San Diego.