CASE PRESENTATION
A 56-year-old woman is referred for evaluation of a rapid and profound decrease in vision in her right eye. The patient states that everything she sees with her right eye “is in a constant fog” and “seems to be worsening fast.” She has difficulty with depth perception and currently wears a bandage over her right eye when driving to decrease glare. The patient reports no history of trauma, ocular surgery, or intraocular injections. She describes an episode of vertical and horizontal diplopia that occurred approximately 1 year ago, resolved without treatment, and was attributed to high blood pressure. Her ocular history includes borderline glaucoma and hypertensive retinopathy in both eyes. Her medications include amlodipine and simvastatin.
On examination, BCVA is counting fingers in the right eye and 20/25 in the left eye with a manifest refraction of +1.25 -0.75 x 105º. Manual keratometry reveals 2.00 D of anterior corneal astigmatism in the right eye. The IOP is 18 mm Hg OD and 19 mm Hg OS. A slit-lamp examination is remarkable for 2+ to 3+ milky nuclear sclerosis and 4+ cortical changes in the right eye and 1+ to 2+ milky nuclear sclerosis and 1+ to 2+ cortical changes in the left eye. There is no view of the posterior segment in the right eye, and B-scan ultrasound is unremarkable. The left eye has a 0.55 cup-to-disc ratio but is otherwise unremarkable.
After discussing the risks and benefits of surgery, the patient elects to proceed with cataract surgery on her right eye. What additional testing, if any, would be helpful when planning surgery? What concerns do you have regarding the risks of surgery? What special procedures or steps during surgery would you consider in order to minimize these risks?
The patient decides to have conventional cataract surgery without addressing her astigmatism. A femtosecond laser is used. After viewing a video of the laser treatment (see below), do you have any additional concerns? If so, how might these concerns affect your surgical plan?
—Case prepared by Cathleen M. McCabe, MD

NICOLE R. FRAM, MD
This patient appears to have a rapidly advancing cataract in her right eye and a history of uncontrolled hypertension. Prior to any surgical intervention, a thorough assessment of her general health is required to ensure that there are no active issues with uncontrolled hypertension or diabetes. This precaution is particularly important given her history of diplopia and the rapid onset of cataract development. Once the patient’s hypertension is confirmed to be stable, if an afferent pupillary defect is ruled out and a B-scan confirms that she has no active retinal pathology, I would feel confident about proceeding with surgery. Preoperatively, it will be important to discuss with the patient both refractive targets and the difficulty of predicting visual outcome, given the advanced white cataract. Similarly, she should understand that she will need spectacle correction for all distances after surgery if her astigmatism is not addressed perioperatively.
When standard cataract surgery is performed on an eye with a white cataract that is intumescent or under pressure, the goal should be to keep the pressure in the anterior chamber higher than that within the lens during creation of the capsulorhexis. Staining with trypan blue dye will be critical for visualization of the anterior capsule because there typically is no red reflex in an eye such as this one.1 A common approach is to puncture the anterior capsule centrally with a 27-gauge needle or cystotome and decompress the milky cortical material while initiating the capsulorhexis. It can be helpful to use a cohesive OVD to flatten the anterior lens capsule and spiral out the capsulorhexis (Figure 1).2 Most dreaded in a white cataract case is the Argentinian flag sign, which occurs when the capsule tears out, potentially past the equator.
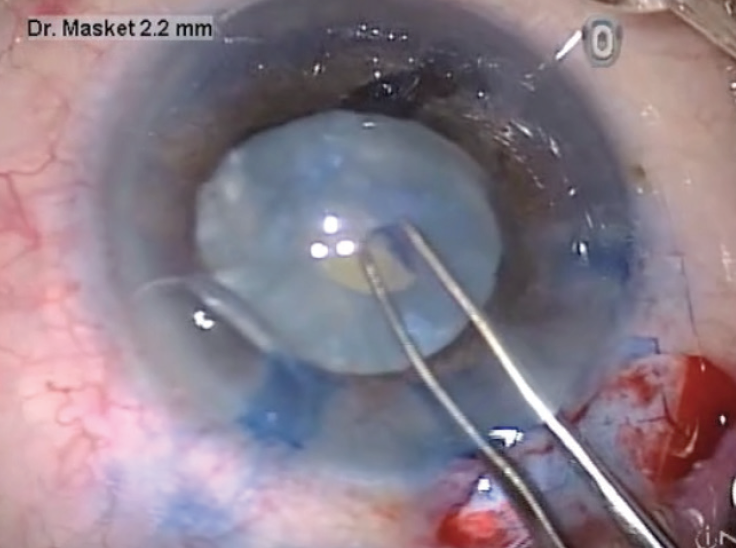
Figure 1. Spiral-out capsulorhexis.
Courtesy of Samuel Masket, MD
If the chamber is shallow, one option is to inject mannitol to decompress the vitreous preoperatively and create more room in the anterior chamber to work. The dosage of intravenous mannitol is 0.5 to 1 g/kg or 12.5 g in 50 mL. Caution is advisable if patients have contraindications such as congestive heart failure.
There also may be circumstances in which the anterior chamber will be too shallow to provide space in which to work despite all efforts. In that event, a dry vitrectomy may be performed to allow room for the OVD to flatten the lens capsule and form the anterior chamber. Doing so involves making a 23-gauge–equivalent sclerotomy located 3.5 mm posterior to the limbus and pointing toward the optic nerve.3 This is obviously out of the comfort zone of many ophthalmologists and should be attempted only by a surgeon who has experience with this technique. If there is absolutely no room to work safely, then a pars plana lensectomy is required.
In my experience, surgery on an eye with a white intumescent cataract can be facilitated by using a femtosecond laser, but achieving a flat dock is critical to avoiding an incomplete capsulotomy, as demonstrated beautifully in Dr. McCabe’s video. Ideally, laser technology that can quickly complete the capsulotomy will decrease the chance of capsular tags and missed laser firings. The duration of laser capsulotomy can range from 0.7 to 10 seconds, depending on the technology. The faster the capsulotomy creation, the less likely that liquefied cortex or milk will be released that may block the laser from completing the capsulotomy (Figure 2). After completing the laser capsulotomy and irrigating the milk from the anterior chamber, therefore, I recommend staining the anterior capsule with trypan blue dye to confirm that the capsulotomy is complete. Chee et al reported that the main complication (17.2%) of laser cataract surgery on an eye with a white cataract was an incomplete capsulotomy, the incidence of which was significantly higher with morgagnian cataracts and increased lens thickness.4 It is therefore important to be aware of this potential complication of laser assistance in cases involving a white intumescent cataract.
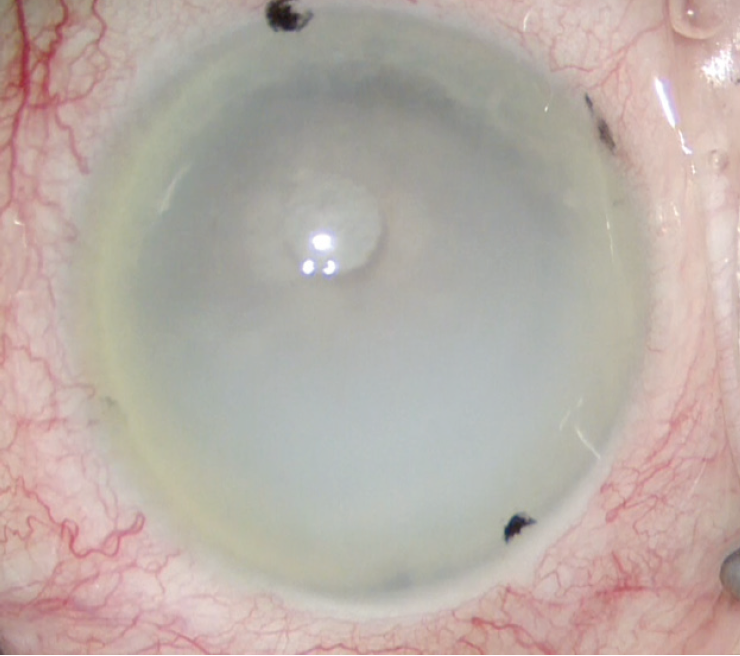
Figure 2. Cortical milk released by laser capsulotomy blocked the laser beam in this eye, so only 2 clock hours were completed. Staining with trypan blue dye improved visualization, and the surgeon manually completed the capsulotomy.
Courtesy of Nicole R. Fram, MD
Laser lens fragmentation is not possible or necessary with a truly white cataract because a laser system cannot cut what it cannot see. Fortunately, the most challenging aspect of this case is creating the capsulotomy, and the rest of the surgery should be routine.

MARIA S. ROMERO, MD
White cataracts are a surgical challenge, and patients should receive thorough counseling before they undergo surgery. Anterior bulging of the crystalline lens and the presence of fluid pockets on OCT images of the anterior segment are suggestive of an intumescent cataract. If these findings are present, intravenous mannitol or a vitreous tap can help to decrease pressure in the posterior chamber.
The benefit of a laser versus a manual capsulotomy is that the former is performed in a closed space, which reduces the pressure differential between the anterior chamber and inside the capsule, thereby decreasing the risk of a runaway radial tear that could lead to the Argentinian flag sign and the risk of a posterior capsular tear. The drawback of a laser capsulotomy is that milky proteins may interfere with the laser, thus leaving the capsulotomy incomplete.5 If this occurs, however, the capsulotomy can easily be completed manually. When I have lacked access to a femtosecond laser in a case such as this one, I have performed a two-staged capsulorhexis, as described by Kara et al.6
However the capsulotomy is executed, I would stain the anterior capsule with trypan blue dye and instill an OVD that has a high molecular weight. After performing gentle hydrodissection, I would tap down the nucleus to prevent it from blocking the anterior capsulotomy and blowing out the posterior capsule.
Whatever technique is used to fragment the lens, it should be one that minimizes cumulative dissipated energy. Protecting the posterior capsule will be important because the cortex is nonexistent, and only a thin layer of epinucleus remains as the scaffold of the posterior capsule. Postoperative steroid therapy can decrease corneal edema.

MICHAEL E. SNYDER, MD
With a mature white cataract, the inherent cause of capsulotomy extension (dubbed Argentinian flag sign when the capsule is stained with trypan blue dye because of the blue and white colors of that nation’s flag) is the uncontrolled release of fluid from the endolenticular space. This results from denaturation and breakdown of the crystalline lens proteins; their breakdown into smaller, more numerous proteins induces an osmotic gradient that causes fluid to flow into the bag, resulting in an endolenticular pressure that is higher than anterior chamber pressure.
OCT imaging shown in the video for this case demonstrates fluid clefts between the lamellae of lens fibers and shows the hyperconvexity of the anterior capsule. When a capsulotomy is created using a femtosecond laser, the opening necessarily has to begin in one area first; it is not a simultaneous event. At the 1:03 time stamp in Dr. McCabe’s surgical video, as she creates the first opening in the capsule, a rapid outward rush of fluid causes a microexplosion.
The sophistication of femtosecond laser systems is seductive for both surgeons and patients. Although a laser capsulotomy may be successful in some eyes with white cataracts, this technology is poorly suited to the inherent physics of an intumescent lens. With a manual approach, the cataract surgeon can overpressurize the anterior chamber with an OVD until the pressure in the anterior chamber exceeds the endolenticular pressure, signaled by and titrated to a flattening of the anterior capsule’s convexity. At that point, the surgeon can safely pierce the central capsule with a 25-gauge needle and aspirate liquid cortex without abruptly releasing the pressure gradient. A continuous curvilinear capsulorhexis can then be safely propagated by means of a traditional approach.
At ophthalmic meetings, I have heard speakers advocate using laser cataract surgery for white cataracts, presumably because visualization is harder in these cases and the surgeon does not need to see the capsule with this technology. Seeing no evil does not mean that it is not present, however, and even evil obeys the laws of physics. Using trypan blue dye solves the visualization challenge in manual cataract procedures. Although docking a femtosecond laser to the eye modestly increases the pressure inside the anterior chamber, success becomes a matter of luck. If the endolenticular pressure is lower than that induced by the laser’s docking interface, then an even capsulotomy will be achieved. If endolenticular pressure is higher, as in this case, a disruption will occur. An intumescent white cataract is an example of a situation in which laser cataract surgery is not better than a manual approach. In an eye with a higher endolenticular pressure, laser cataract surgery is worse.

WHAT I DID: CATHLEEN M. MCCABE, MD
Intumescent white cataracts present a surgical challenge, especially during creation of the capsulotomy. When a patient has a unilateral, advanced cataract and reports a rapid onset of worsening visual acuity, clinicians must suspect the possibility of additional complicating factors such as posterior capsular pathology. The risk of rupturing the posterior capsule is elevated in patients with a history of trauma, pars plana vitrectomy, or posterior segment injection. B-scan ultrasonography can sometimes reveal additional pathology such as a discontinuity in the posterior capsule or a mass in the posterior segment.
I have found anterior segment OCT images obtained during laser cataract surgery to be invaluable. Irregularity of the posterior capsule can sometimes be visualized, although the cataract may be too dense in some cases to permit adequate imaging of the posterior margin of the lens. A tilted or decentered lens may suggest zonulopathy. In these instances, the thickness of the lens can be highly variable, ranging from very thick to extremely thin. Prior knowledge of the thickness—especially of a thin, opaque lens—can help the surgeon avoid iatrogenic rupture of the posterior capsule during phacoemulsification.
In the case presented here, I chose to use a femtosecond laser in effort to increase procedural safety by imaging the thickness and orientation of the lens and by creating the capsulotomy in an efficient and precise manner. It is important that the dock be as flat as possible so that the capsulotomy is completed quickly and the laser treats all quadrants at once. In this way, the release of internal lenticular pressure happens at several points simultaneously, distributing the stress on the capsule. A flat dock can be difficult to attain, however, given that the patient is not able to see well enough to fixate easily. I sometimes use forceps to help stabilize the eye during the docking procedure. Watching the capsulotomy creation is always a bit worrisome because a sudden release of fluid and pressure within the lens can theoretically rupture or tear the anterior capsule. In this case, a sudden release of fluid is seen when the capsulotomy proceeds to the nasal quadrant. I was therefore highly suspicious that an anterior capsular tear might have occurred in that area.
In the OR, I opened the paracentesis with a spatulated cannula designed for that purpose. Next, I instilled preservative-free 1% lidocaine in the anterior chamber, followed by trypan blue dye (VisionBlue, Dutch Ophthalmic USA). I filled the anterior chamber with a dispersive OVD (Viscoat, Alcon) while flushing out the trypan blue dye. Next, I gently grabbed the capsule with Utrata forceps and carefully removed it from the eye. When I suspect there may be tags or an incomplete capsulotomy, I find it helpful to move the capsule in a circular fashion prior to its removal in order to break any attachments that may remain. I spread the capsular fragment on the cornea and examined it. Despite the suspicious release of fluid during laser treatment, a circular and complete capsulotomy had been achieved.
During nuclear disassembly, I removed a small wedge of cortical cataract, revealing a lucency in that area that seemed suggestive of a rent in the posterior capsule. I withdrew the chopper while the phaco probe remained in the eye. I replenished the dispersive OVD in the anterior chamber before removing the phaco tip from the eye in order to avoid collapse of the anterior chamber and vitreous prolapse through the suspected defect. I inspected the area under high magnification and placed an OVD at the site of the suspected defect. The OVD did not pass into the vitreous, confirming the integrity of the posterior capsule.
The remainder of the surgery was unremarkable, and UCVA was 20/30 in the operated eye on postoperative day 1. This case illustrates the typical manner in which I treat patients with intumescent white cataracts. Although it is important to maintain a high index of suspicion for complications, I have found that, in most instances, these surgeries proceed routinely after a complete and uneventful capsulotomy. I believe that use of a femtosecond laser improves my ability to perform routine, uncomplicated surgery in these patients.
1. Melles GR, de Waard PW, Pameyer JH, Houdijn Beekhuis W. Trypan blue capsule staining to visualize the capsulorhexis in cataract surgery. J Cataract Refract Surg. 1999;25(1):7-9.
2. Gimbel HV, Willerscheidt AB. What to do with limited view: the intumescent cataract. J Cataract Refract Surg. 1993;19(5):657-661.
3. Machemer R. Subtotal vitrectomy through the pars plana. Trans Am Acad Ophthalmol Otolaryngol. 1973;77(2):OP198-201.
4. Chee SP, Chan NS, Yang Y, Ti SE. Femtosecond laser-assisted cataract surgery for the white cataract. Br J Ophthalmol. 2019;103(4):544-550.
5. Taravella MJ, Meghpara B, Frank G, Gensheimer W, Davidson R. Femtosecond laser-assisted cataract surgery in complex cases. J Cataract Refract Surg. 2016;42(6):813-816.
6. Kara-Junior N, Santhiago MR, Kawakami A, Carricondo P, Hilda WT. Mini-rhexis for white intumescent cataracts. Clinics (Sao Paulo). 2009;64(4):309-312.




