
Cataract surgeons today have access to unprecedented technologies that help to make our cases go smoothly and quickly and that produce outstanding results. With the use of femtosecond lasers, intraoperative aberrometry, and refined phacoemulsification technologies, we can help our patients achieve excellent UCVA on the first postoperative day after uncomplicated cataract surgery.
But sometimes we face a cataract that is not amenable to today’s technologies, and we have to look to the techniques of yesterday—techniques that all surgeons should have in their cataract tool kits for just such eventualities. In this article and accompanying video (see Watch It Now), I present such a case, a rock-hard cataract with diffuse zonular instability that required use of an extracapsular cataract extraction (ECCE) technique.
SURGERY WITH A GUARDED PROGNOSIS
A 57-year-old man presented with a long-standing cataract, associated with a traumatic event that occurred 40+ years prior (Figure 1). Visual acuity in this eye was hand motion and in the fellow eye was 20/20. The patient was interested in cataract surgery to improve cosmesis. Because of the rock-hard nucleus, phacodonesis, and the decades-long persistence of the cataract, the visual prognosis for this eye was guarded. In the course of a thorough informed consent process, we discussed all the possible risks and outcomes of performing ECCE to remove the cataract, and the patient agreed.
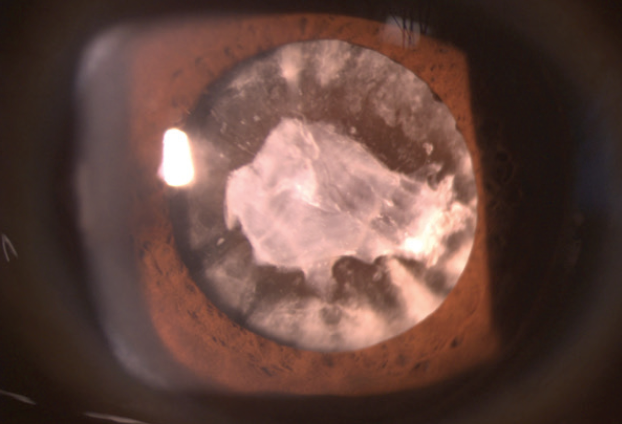
Figure 1. The patient presented with a traumatic cataract of long standing.
The ECCE surgery began with creation of a conjunctival peritomy with Westcott scissors, exposing about 11 mm of the sclera. After hemostasis was established, a limbal groove was created using a crescent blade (Figure 2). The anterior chamber was first entered with a 1-mm paracentesis blade to maintain firm control of the anterior chamber, followed by injection of an OVD.
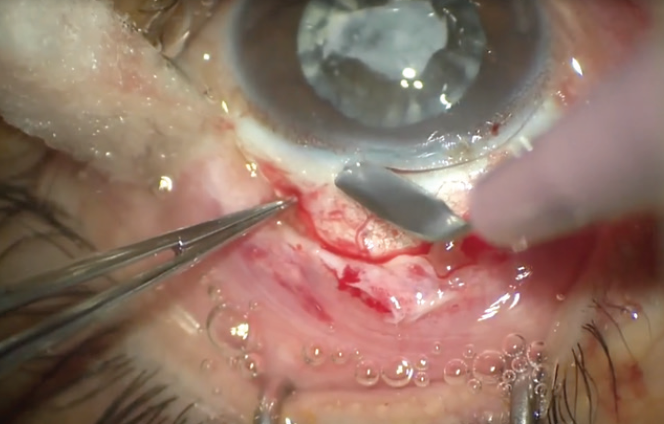
Figure 2. A limbal groove is created using a crescent blade.
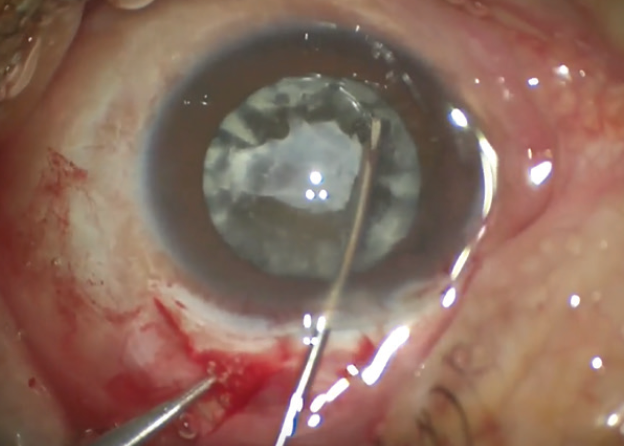
Figure 3. A can-opener capsulotomy is performed.
A can-opener capsulotomy was then created through the paracentesis opening (Figure 3), and the nucleus was mobilized. During these steps, I expectantly noted significant movement of the nucleus secondary to severe diffuse zonular instability and zonulolysis. It was important to take these steps slowly and methodically, so as not to create any further zonulolysis.
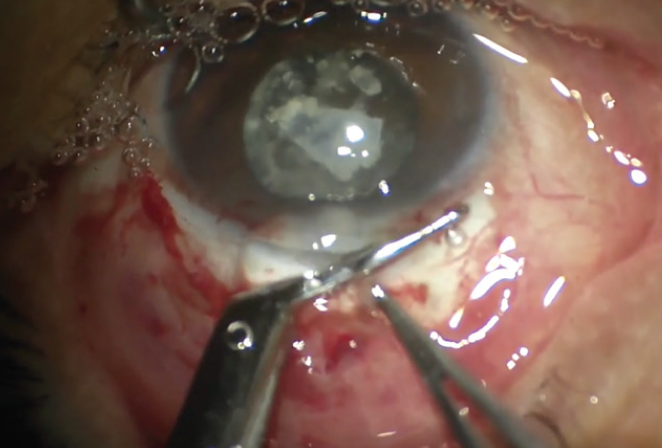
Figure 4. Corneal scissors are used to extend the wound to the left and right of the paracentesis.
Next, corneal scissors were used to extend the incision to the left and right of the paracentesis (Figure 4) to allow delivery of the nucleus. As with everything we do in surgery, it’s safety first, so two 7-0 polyglactin sutures were placed—one on each side of the main wound—to allow me to maintain control of the eye later in the case. They were placed about 6 to 7 mm apart to accommodate implantation of the IOL (Figure 5).
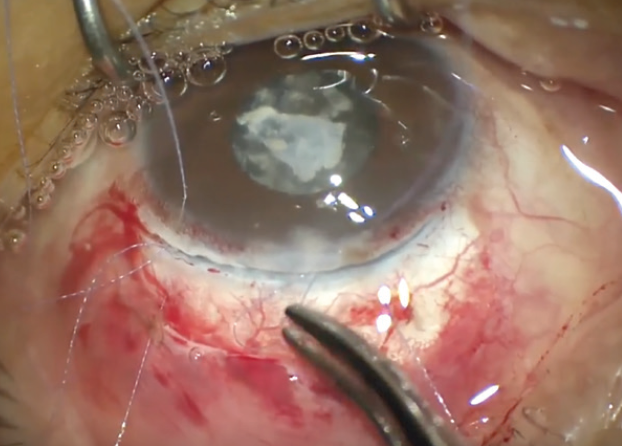
Figure 5. Two 7-0 polyglactin safety sutures are placed, 6 to 7 mm apart.
Pressure was then applied about 2 mm posterior to the limbal groove to mobilize the nucleus and express it from the anterior chamber. In this difficult case, it took two attempts before the nucleus was mobilized and delivered from the eye (Figure 6).
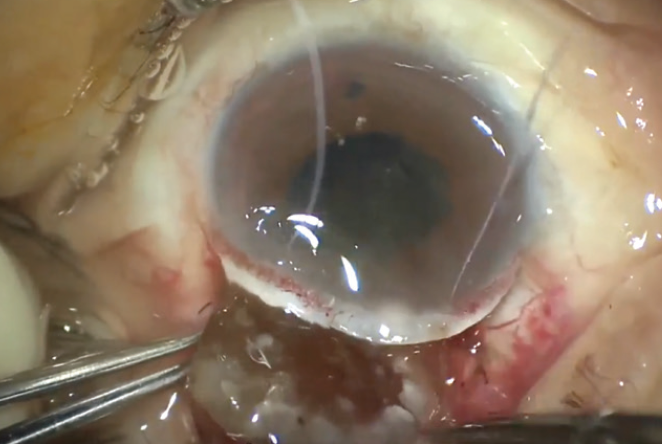
Figure 6. The nucleus is expressed.
Once the nucleus was expressed, the 7-0 safety sutures were quickly tied down. Irrigation and aspiration were performed to remove residual cortex, and a three-piece IOL was inserted, passed between the safety sutures.
After the trailing haptic was tucked behind the iris and into the sulcal space, the wound was checked for vitreous strands and then closed with multiple interrupted sutures. Finally, the conjunctiva was closed. At the end of the case, the pupil was round and there was no presence of vitreous in the anterior chamber or to the wound.
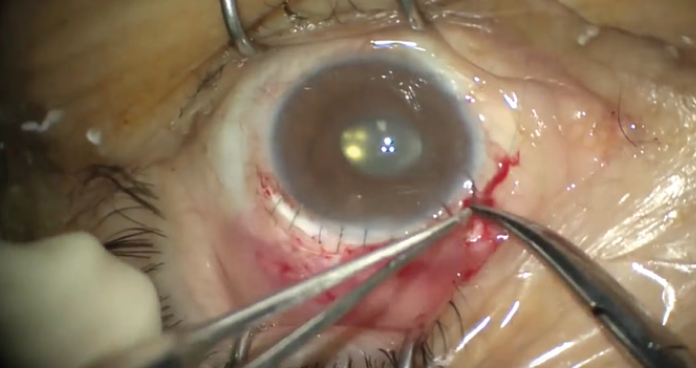
Figure 7. The wound is closed with interrupted sutures.
The postoperative outcome was satisfactory (Figures 8 and 9), with a 3-line improvement in UCVA, likely secondary to deprivation amblyopia and concurrent astigmatism. Given the young age at which the traumatic event occurred, we anticipated some element of uncorrectable amblyopia, as the cataract may have interfered with development in the normal visual pathways. Final visual acuity was 20/150. However, the patient was happy with the result of the case, as were we.
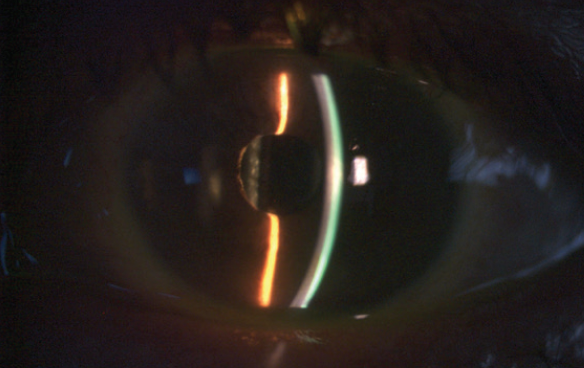
Figure 8. Postoperative image of the eye at the slit lamp.
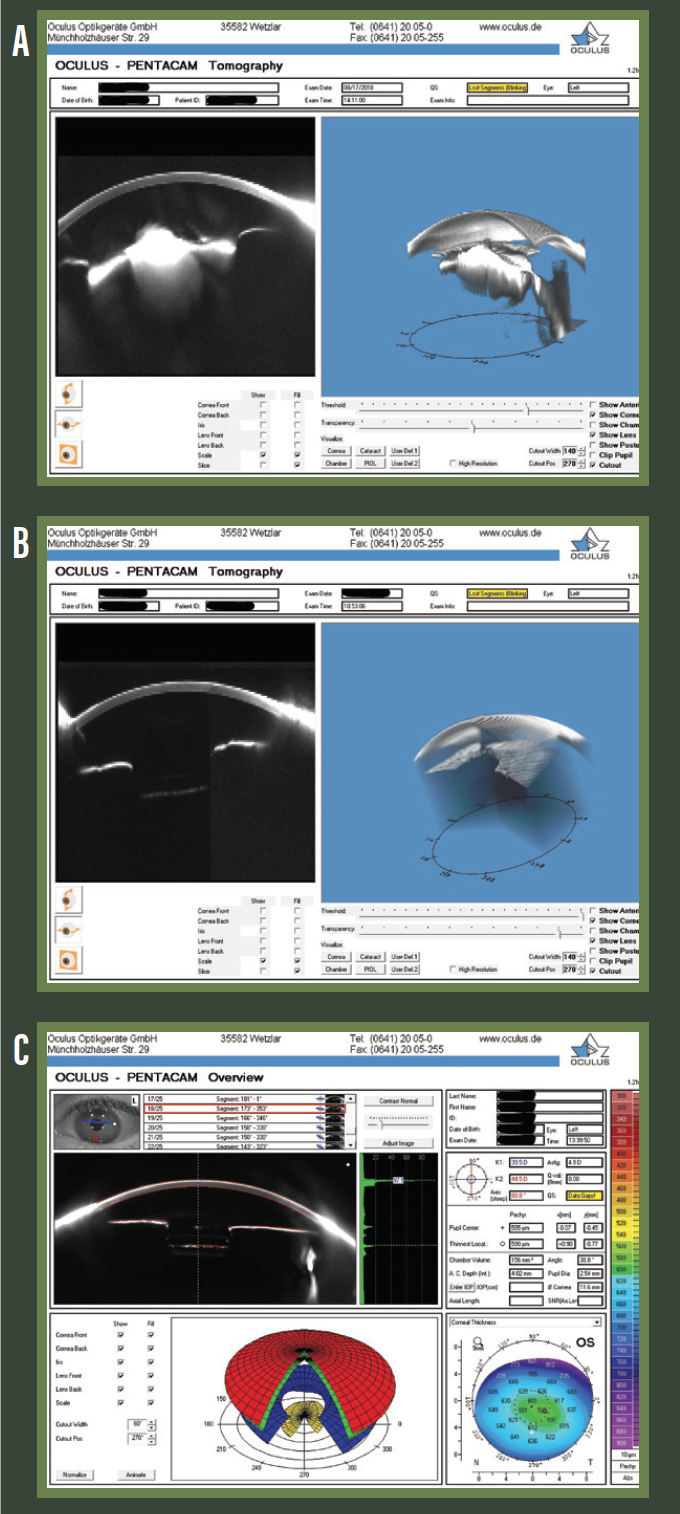
Figure 9. Preoperative (A) and postoperative day 1 (B and C) Pentacam (Oculus Optikgeräte) images.
CONCLUSION
The moral of this story is that older techniques that some believe are better relegated to the history books can prove practical for challenging cases such as this one. Do not neglect ECCE (or intracapsular cataract extraction) and other manual techniques because you never know when you might need to use them.




