

This article details the case of a patient with unrealistic expectations of cataract surgery whom we managed over a period of 10 years. This 41-year-old man presented to our clinic for an opinion on his eyes. He had undergone LASIK for high myopia 1 year earlier, performed by a surgeon at another center. He was angry and was considering litigation against that refractive surgeon.
The patient reported significant double, blurred, and shadowed vision even with the use of glasses since his refractive procedure. He reported that his manifest refraction before LASIK was -13.00 D in each eye. This patient was a business owner and was not concerned about cost if there was anything he could do to help his eyes.
On examination, the patient’s UCVA was 20/40 OD and 20/50 OS. His BCVA was 20/25 OD with a manifest refraction of +0.50 +1.00 x 165° and 20/30 OS with a manifest refraction of plano +1.00 x 162°. The patient’s corneas were clear with a well-centered LASIK flap in each eye. His lenses were clear, and the retinal health was unremarkable. Topography showed a well-centered high myopic LASIK ablation (Figure 1). Central pachymetry was 452 µm in the patient’s right eye and 447 µm in his left (Figure 2).
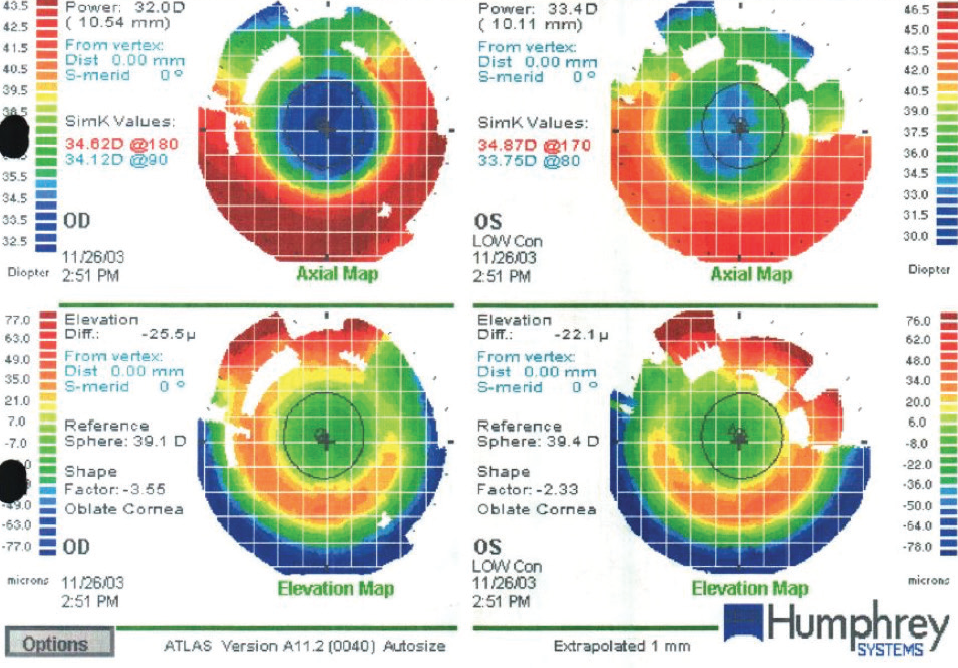
Figure 1. The patient’s topography showed a well-centered high myopic LASIK ablation.
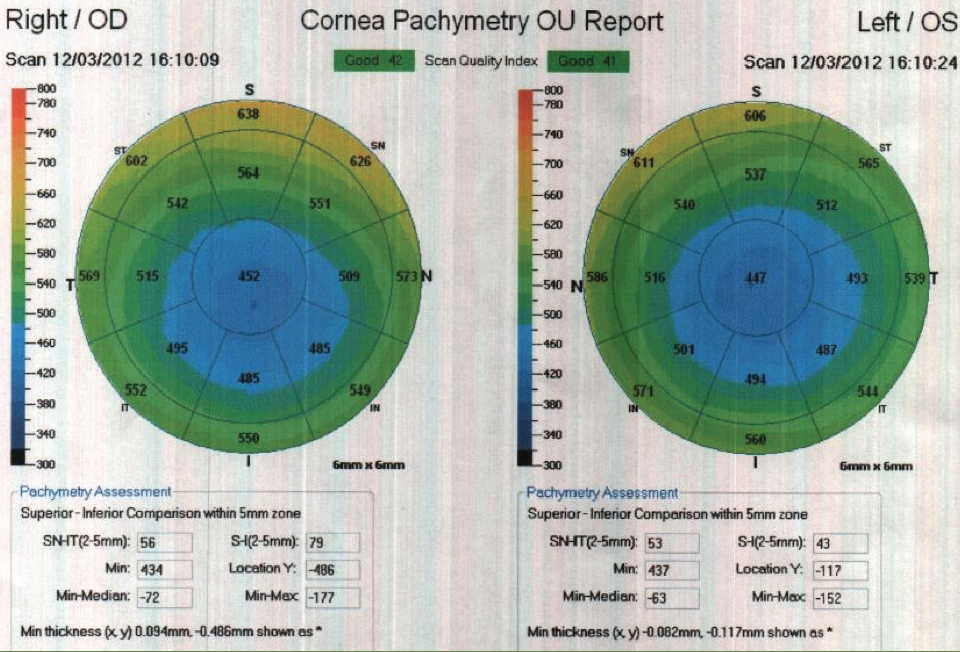
Figure 2. Central pachymetry in the patient’s right and left eyes.
A gas permeable contact lens fitting was recommended for the patient to assist with his vision. No further surgery was recommended.
STILL FRUSTRATED
The patient returned for the first time 4 years later, still frustrated with the same complaints of double, shadowed, blurry vision even with glasses and contact lenses. At this exam, the patient said he was continuing to seek further surgery to, in his words, “fix” his vision. His BCVA had improved to 20/20 OU with manifest refraction of +0.25 +1.75 x 180° OD and +0.25 +1.25 x 175° OS. His ocular health and topographies remained stable with no signs of cataract or retinal pathology. Again, we recommended no further surgery because we expected to see minimal improvement in symptoms.
The next time the patient returned, now 8 years after LASIK, there was a significant change to his vision, and he was still looking for a way to see “perfectly” again. His refraction had shifted to -4.00 +1.50 x 175° OD and -2.50 +1.75 x 175° OS, resulting in 20/25 BCVA OU. The patient’s topography remained stable, with no signs of ectasia. Dilated examination showed a 2+ nuclear sclerotic and cortical cataract in each eye.
We educated the patient on cataracts and cataract surgery and the challenges that his eyes posed. Because of his flat keratometry and thin pachymetry values, there would be limited to no potential for laser vision correction enhancement after a cataract procedure.
Even after extensive education regarding the limitations of cataract surgery with his ocular status, the patient held unrealistic expectations of the level of vision improvement that could be gained after a cataract procedure. Despite our efforts to explain, he anticipated that any further procedure on his eyes would bring him back to the same level of vision he had before LASIK. At this time, we recommended that the patient wait to undergo cataract surgery and continue to use contact lenses to achieve his best visual acuity.
The patient was seen several times over the next few years. At every examination, he was again educated on the status of his eyes and the realistic expectations for his vision after cataract surgery. As long as we didn’t feel confident with the patient’s level of understanding of the limitations of his vision postoperatively, it was our opinion that his visual needs were best managed with nonsurgical options.
The patient pursued second opinions. Because of the level of trust he had gained with our clinic over the years, even when he was offered surgery at another clinic, he elected to follow our guidance and refrained from undergoing surgery elsewhere.
FINALLY SELF-AWARE
Finally, after 10 years of continued worsening of objective and subjective findings, the patient came to a level of self-awareness regarding his ocular status. He understood that cataract surgery would not fix everything with his vision.
At this point, the patient’s BCVA was 20/60 OD with a manifest refraction of 10.00 +1.75 x 140° and 20/50 OS with manifest refraction of -8.25 +2.50 x 010°. Cataract surgery was recommended, and the patient elected to proceed. After uncomplicated cataract surgery, the patient had a good objective outcome, with uncorrected vision as expected secondary to irregular astigmatism. At 2 months postoperative, the patient’s UCVA had improved to 20/25 OD and 20/60 OS. His BCVA was 20/20 OD with manifest refraction of -0.25 +0.75 x 170° and 20/25 OS with manifest refraction of -0.75 +2.00 x 035°.
The patient was happy with his outcome and has since referred many family members and friends to our clinic.
DEVELOPING TRUST
What we learned from this patient was the importance of managing expectations and developing trust over time. This unhappy refractive surgery patient had significantly unrealistic expectations for cataract surgery, which we managed over a time span of 10 years.
In our experience, if a patient has unrealistic expectations for a procedure preoperatively, he or she will be difficult to please postoperatively. This patient was already distrusting of ophthalmology because of the visual symptoms he experienced after his LASIK surgery. Secondary to his flat topography, irregular astigmatism, and thin pachymetry, there was limited ability to enhance the patient’s vision after cataract surgery. He would need to continue to wear glasses and likely continue to have some of the visual symptoms that had been present ever since his laser vision correction. Rushing into another surgery with this patient could have resulted in an angry patient, as all of his visual symptoms would likely not be resolved to his unrealistic level of expectation.
When eye care practitioners are deciding whether to proceed with an elective ocular surgery, it is important to determine if it is likely that the patient’s visual symptoms will improve from the procedure. More important, we must determine whether it is likely that the patient’s visual symptoms will improve to the level of his or her expectations.
This particular patient developed a visually significant cataract, but he remained focused on symptoms that had started after his LASIK procedure many years before and that were likely to continue even after cataract surgery. Not until the patient finally understood the visual implications of his previous laser vision correction did we finally offer cataract surgery.
When we are considering a surgical procedure, a trusting relationship with the patient is a necessity—especially for a patient with a difficult personality or a complex ocular history. This particular patient had been working with our clinic for 10 years prior to undergoing a procedure, even though at every examination he was seeking a surgical solution to his visual concerns. Because of this trust developed over the years, the patient became less angry and demanding and was compliant with our recommendations.
A patient with a complicated eye history or personality often requires more time and finesse postoperatively. When we enter into a postoperative journey with a trusting relationship, it helps make the process smoother, especially if there is a high likelihood of a variable result or a long healing course. In some cases, trust is gained over one or two examinations. But other patients may require a relationship over years to develop the trust necessary for a positive surgical relationship.




