
A 66-year-old woman is referred for a glaucoma evaluation by her family optometrist. She was diagnosed as a glaucoma suspect a few years earlier, and now there is concern regarding possible progression. She has no chief complaint except for intermittently blurred vision, which is most noticeable when reading. She uses over-the-counter Systane Ultra lubricant eye drops (Alcon) twice a day in each eye, which helps.
Comparing your current examination findings with previous findings, you determine that she is indeed showing progression, and you subsequently modify her diagnosis to open-angle glaucoma. Before you enter the room to explain your findings and discuss treatment options, your technician conveys to you that the patient remarked that, if treatment is absolutely necessary, she would prefer a generic medication.
Does this scenario sound familiar?
BACKGROUND
Glaucoma is a chronic progressive optic neuropathy most commonly associated with elevated IOP. If left unchecked, progression of the disease is likely to occur, resulting in visual field loss and, eventually, blindness. According to the World Health Organization, of the 37 million people who are blind worldwide, glaucoma is the main cause in roughly 5 million.
The estimated prevalence of glaucoma in those greater than 40 years of age is 2.4%, and this increases to roughly 7% in those over age 70.1 Meanwhile, the prevalence of ocular surface disease (OSD) is estimated to be more than twice those percentages in similar age groups.2
According to the Women’s Health Study, several factors influence the prevalence of OSD, including age, sex, and, to a certain extent, race.3 Studies have also shown that glaucoma patients are at higher risk for developing or exacerbating OSD, largely due to the long-term use of preservative-containing eye drops designed to lower IOP.4 Leung and colleagues found that 60% of patients being treated for glaucoma reported dry eye symptoms.4
It has long been recognized that eye drops containing a preservative may initiate or exacerbate OSD if used long and often enough. In recent years, there has been a growing appreciation of the ocular side effects of ophthalmic preservatives, especially in the subspecialty of glaucoma. While a positive side effect of a preservative might be enhanced tissue penetration of the active ingredient, the adverse short- and long-term side effects of these substances related to OSD may be of more concern.
The most common preservative found in prescription and over-the-counter eye drops is benzalkonium chloride (BAK). A number of studies have demonstrated that repeated BAK exposure can weaken cellular junctions, decrease goblet cell density, and increase inflammatory mediators on the ocular surface.5 In fact, BAK concentrations as low as 0.005% can induce pathologic change.6 Because the effects of BAK are not only dose dependent but also cumulative, long-term exposure can adversely affect wound healing and, secondarily, filtration surgery outcomes.7,8
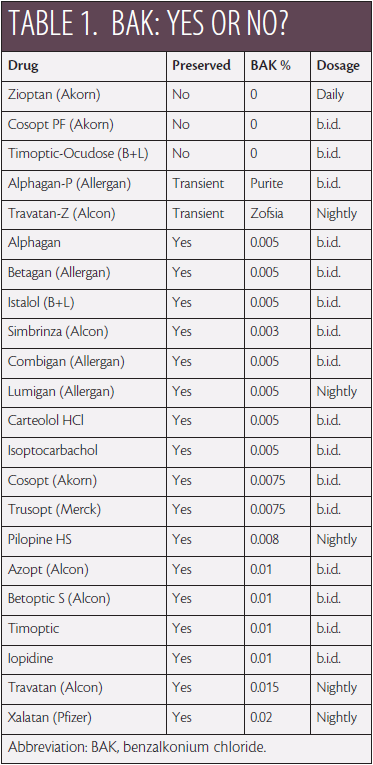
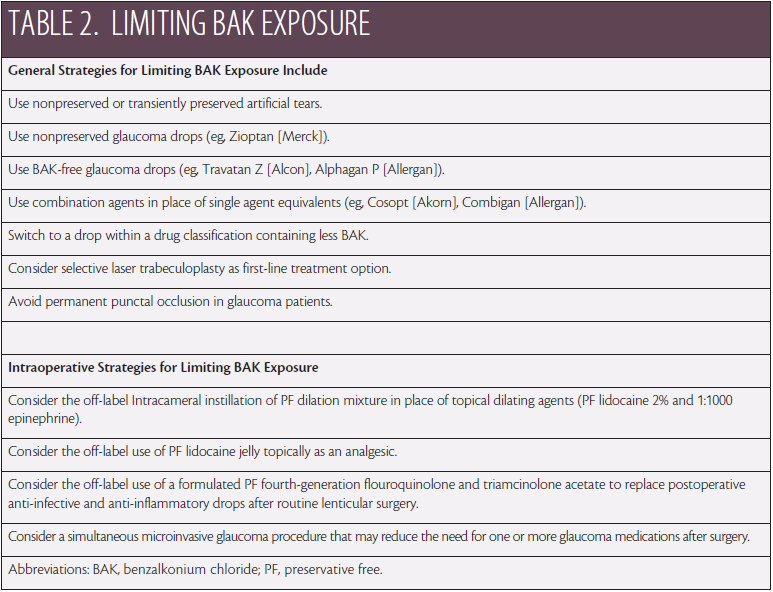
Pharmaceutical companies have responded to the pleading of cornea and dry eye specialists around the country by developing glaucoma products that reduce the BAK load to the eye (Table 1). There are also clinical and perioperative strategies that can help prevent patients from developing symptomatic dry eye disease (DED) (Table 2).
Given this increased effort in the fight against iatrogenic DED in glaucoma, are we clinicians doing our part? Is this an important enough issue to add a few minutes of valuable chair time to explain, for example, the potential benefits of a branded product over a generic one in an effort to reduce the BAK load to the eye in our glaucoma patients? Is this an important enough issue to broach the idea of selective laser trabeculoplasty (SLT) as a first-line treatment with the same goal in mind?
Not sure of your answer? Consider the following.
THE ECONOMIC BURDEN OF GLAUCOMA AND OSD
The difference in direct out-of-pocket expense for certain branded products that are more preservative “friendly” compared to some that are not can be significant. Eye care practitioners are naturally sensitive to the economic burdens their patients face and will often acquiesce to use of a less expensive generic product without debate.
It has been estimated that a diagnosis of glaucoma carries with it an average annual cost of $2,200 in direct medical expenses alone. Meanwhile, according to Yu and colleagues, excluding products such as Restasis (cyclosporine ophthalmic emulsion 0.05%; Allergan) and punctal plugs, the annual direct medical costs for DED can range from $678 for patients with mild symptoms to $1,267 for those with severe symptoms.9
Dismissing preservative-free or preservative-friendly products in favor of generics may seem like the logical approach to mitigating this expense. The economic burden for any condition, however, is more complex than only the direct medical costs.
The economic burden of any disease state is actually defined in terms of direct medical costs (cost of medication, treatments, office visit copayments, etc.) plus complication costs (eg, cost associated with managing a secondary infection) plus overutilization costs (eg, cost of punctal cautery or autologous serum) plus indirect costs (eg, lost time at work, decreased productivity).
How many times have you been forced to have patients return for extra visits because the generic product has been less consistent or less predictable than a branded version would have been? Was there lost productivity at work involved for the patient? Did a family member have to take time off work to bring the patient to the appointment? All of these ancillary costs figure into the total cost.
UTILITY ASSESSMENT IN DED
Although the imposed economic burden of iatrogenic OSD cannot be overlooked, its impact on quality of life may be more telling.
The symptoms associated with DED (redness, irritation, burning, scratchiness, blurriness, and pain) can be severe and even debilitating. Recent quality-of-life studies found that patients with moderate to severe DED had comparable quality-of-life utility scores to patients on dialysis or with severe angina or a disabling hip fracture.10.11
It is time to stop treating glaucoma and OSD each in isolation and begin to realize that glaucoma patients represent a significant demographic in dry eye clinics around the country. Following are a few strategies that can help you make a difference in your patients’ long-term quality of life.
Strategy No. 1. Discuss the Indirect Costs of Treatment
With respect to the patient described at the outset, it would have been easy for me to take the path of least resistance and acquiesce to her request regarding generic eye drops. However, her decision would not have been an informed one. Instead, I took the time to educate the patient on the potential side effects of preservatives such as BAK, took the time to explain the variability of generic products and how this can lead to extra office visits and copayments, and took the time to explain the possible benefits of considering SLT with the potential of no need for drops.
When I explained to this patient that the long-term use of BAK has been associated with worsening of OSD symptoms and sometimes a decline in reading endurance, this was all she needed to hear. As a self-proclaimed avid reader, she immediately wanted to hear other options. Cost was no longer her number one concern.
The lesson here is, do not prejudge or make assumptions about patients’ wants and needs. Present the facts, and let them speak for themselves.
Strategy No. 2. Use Framing to Highlight Your Recommendation
There has been a significant amount of research on the psychology of choice. Framing is a marketing concept that has been shown to be effective in influencing consumers’ behavior and to ease consumers’ decision making.
The premise is that, when dealing with a cost-conscious consumer, if you offer two options, the consumer tends to select the cheaper product most of the time. When at least three options are presented, however, the patient is more likely to feel better about selecting a product priced higher than baseline, because he or she knows that the expense is still favorable to another higher-priced alternative.
In the case example, I believed the patient would be best served using preservative-free Zioptan (tafluprost ophthalmic solution 0.0015%; Akorn). Therefore, I decided to frame this product between another branded prostaglandin analogue with low or no BAK and SLT. Once she was informed of the benefits of preservative-free, once-daily Zioptan, she concluded (and I concurred) that this was the best approach to start with. She felt good about her decision, because she knew there was more to it than just price, and she felt that this was a good middle-of-the-road way to start therapy.
Strategy No. 3. Provide Hope Through Microinvasive Glaucoma Surgery
Although this patient did not have clinically significant cataracts, I believed it was a good idea to touch on microinvasive glaucoma surgery (MIGS) for two main reasons. First, MIGS provides hope to patients that they may not have to take drops for the rest of their lives, and this future potential, in turn, justifies the current acceptance of a higher-priced treatment regimen.
Second, ppatients are more apt to consider or feel better about choosing a more expensive treatment regimen if they believe their treatment may be short-term or finite. When you consider a 45-year-old’s lifetime commitment to glaucoma therapy compared with that of someone who is 65 years old, a few dollars at a time can make a big difference over that additional 20-year span. That said, the use of a preservative-free product is potentially even more important in younger patients, considering that BAK’s adverse effects on the ocular surface are cumulative.
Although no guarantee was given to the patient, hope was provided that she might one day be able to get rid of the eye drops via MIGS when we simultaneously address her cataracts in the future.
Strategy No. 4. Set Realistic Expectations
I explained the goals of therapy to this patient, as I do all patients:
“It is always my goal to have you visit the office the least number of times you need to be here and to be taking the least amount of medicine you need to be on in order to achieve our goal, which is protecting your eyesight. Sometimes, extra visits and extra tests will be needed in order to do this. If you do your part and take your drops to the best of your ability, however, together we will be successful.”
This explanation tells her a number of things. First, I care about her, and I will do my best to keep her direct and indirect costs to a minimum. Second, I am not expecting perfection from her. I do not set patients up for failure by asking them to be 100% compliant with their medical therapy or their office visits. I take time at each visit to address any barriers to treatment adherence or issues related to chronic reappointments.
CONCLUSION
When we consider the comorbidity of OSD and glaucoma, the combined economic impact can be overwhelming for patients. Already, too many patients are forced to prioritize their health problems and decide how best to utilize their limited prescription drug plans and financial resources.
That said, we must not prejudge what is most important to patients with respect to their care. Although a fair number of my patients may still choose generic medications based on direct costs alone, I will sleep well at night knowing these are well-informed choices.
1. Heijl A, Leske MC, Bengtsson B, et al; Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268-1279.
2. Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264-1268.
3. Schaumberg DA, Sullivan DA, Buring JE, et al. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318-326.
4. Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17(5):350-355.
5. Noecker R. Effects of common ophthalmic preservatives on ocular health. Adv Ther. 2001;18(5):205-215.
6. Ichijima H, Petroll WM, Jester JV, et al. Confocal microscopic studies of living rabbit cornea treated with benzalkonium chloride. Cornea. 1992;11(3):221-225.
7. Broadway DC. Reversal of topical anti-glaucoma medication effects on the conjunctiva. Arch Ophthalmol. 1996;114:262-267.
8. Broadway DC, Grierson I, O’Brien C, Hitchings RA. The outcome of filtration surgery. Arch Ophthalmol. 1994;112:1446-1454.
9. Yu J, Asche CV, Fairchild CJ. The economic burden of dry eye disease in the United States: a decision tree analysis. Cornea. 2011;30(4):379-387.
10. Schiffman RM, Walt JG, Jacobsen G, et al. Utility assessment among patients with dry eye disease. Ophthalmology. 2003;110:1412-1419.
11. Buchholz P, Steeds CS, Stern LS, et al. Utility assessment to measure the impact of dry eye disease. Ocul Surf. 2006;4:155-161.
Richard B. Mangan, OD, FAAO
• private practice in Lexington, Kentucky
• eyeam4uk@gmail.com
• financial interest: none acknowledged


