
Despite impressive technological and technical advances, an IOL exchange is still sometimes necessary. When an IOL implanted in the capsular bag is dangling after a YAG capsulotomy, management can be complex, owing to fibrosis of surrounding structures. This article shares tips based on my experience for success with these challenging cases (Figure 1).
EVALUATION
Intraoperative assessment is key to determining how to proceed. because it allows the surgeon to determine the exact position and extent of the fibrosis. Although every case is unique, I have found that two factors in particular influence my plan: (1) the amount of membrane formation over and around the IOL and (2) the stability of the bag preoperatively and during all surgical steps.
My first tip is to make the right number of incisions to permit a bimanual approach at all times.
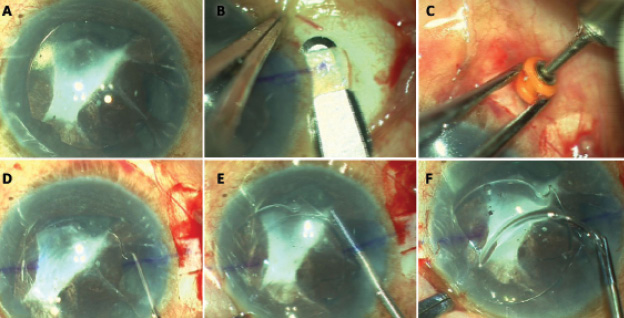
Figure 1. A posterior chamber IOL (PCIOL) in the anterior chamber (A). A temporal scleral flap is created (B). A 23-gauge trocar cannula infusion is placed (C). The PCIOL is dislodged from the iris (D and E). The broken haptic is explanted (F).
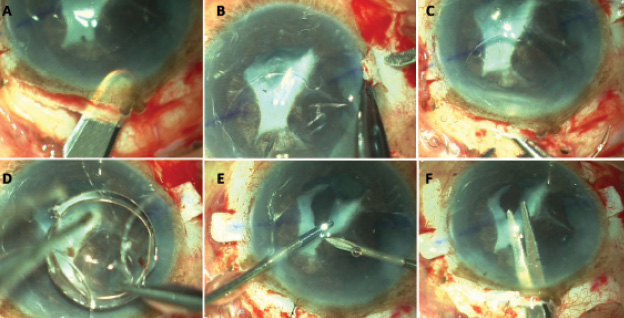
Figure 2. A scleral tunnel is created during small-incision cataract surgery (A). Sclerotomies are made 1.5 mm under the flap and behind the limbus (B). The PCIOL is explanted with the other haptic still attached (C and D). The fibrous membrane is excised (E and F).
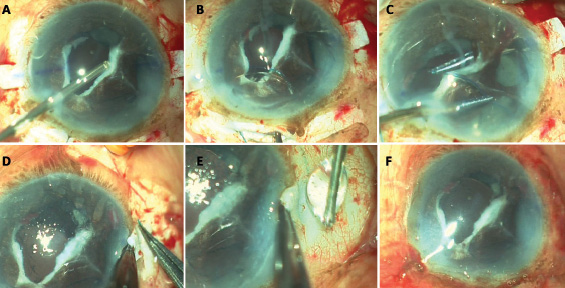
Figure 3. The surgeon uses a vitrectomy cutter to excise the membrane (A). The leading haptic is externalized (B), followed by the trailing haptic (C and D). Fibrin glue is applied under the scleral flaps (E). The end of the case (F).
I cannot overstate the importance of having the proper instruments on hand. For me, this includes a Y rod, dialer, Vannas scissors, and a dispersive ophthalmic viscosurgical device. These tools help me to carefully dissect all adhesions and to retract iris tissue so that I may assess the posterior chamber and the stability of the bag.
It is necessary to inject enough viscoelastic to displace any membrane and then evaluate its looseness. I use a Y rod to retract the iris on all sides so as to evaluate the adhesions. Most of them can be released simply with the rod, but some may be difficult to break or may raise concern about bleeding. In that situation, I recommend against the application of force. Rather, I suggest simply cutting the adhesions with Vannas scissors (Figure 2). At times, a snip at the optic-haptic junction may be necessary.
Should bleeding occur, I find that diathermy can be helpful, but sometimes, an air bubble tamponade is necessary. The key is not to panic.
EXPLANTING THE LENS
After releasing adhesions, I bring the IOL into the anterior chamber—either from the bag or the sulcus—haptic by haptic. During this process, I carefully observe every movement of the IOL. If additional adhesions become evident and they are not very strong, a simple trick is to place the Y rod below the optic-haptic junction on one side and to pull toward the endothelium (Figure 1). In other cases, it may be possible just to pull through the haptic.
If there is or was any communication between the anterior and posterior segments during this or the previous surgery, I believe a vitrectomy is warranted. Because the vitrectomy port will attract and cut vitreous, a vitrectomy performed in the anterior chamber will draw more vitreous to the anterior chamber from the posterior segment. I therefore prefer a pars plana/pars plicata approach in these cases. Immediately before initiating the vitrectomy, I place an anterior chamber maintainer or a trocar cannula with infusion in the eye.
After the IOL is in the anterior chamber, it can be cut with scissors and explanted through a small clear corneal incision or extracted in its entirety through a scleral tunnel incision created in accordance with the size of the lens optic (Figure 2A).
If it is trapped in the iris tissue, I will amputate a haptic with scissors so that I can explant the optic and other haptic. I can then remove the stuck haptic from the other side by dialing it in the right direction (Figure 2C and D).
IMPLANTING THE IOL
I will place the new IOL in the capsular bag if it is intact and stable.
I will place the IOL in the sulcus if the posterior capsule is defective but the anterior capsular rim is stable and no zonular dehiscence is evident or if the bag is intact and stable but adhesions are present between the anterior and posterior capsules.
When the bag is unstable and the anterior capsular rim is defective, zonular dehiscence is evident, or the posterior capsule has ruptured and there are fibrotic adhesions in the sulcus, I recommend implanting an anterior chamber IOL, fixating the IOL to the sclera with sutures, or using the glued IOL technique. Because I myself prefer the third option (Figure 3), I make the initial scleral flaps while the eye is taut, after verifying capsular support.
CONCLUSION
Successful IOL exchanges require careful planning. The steps described herein have helped me to achieve a systematic and reproducible approach to IOL exchange in eyes with a capsular bag defect.
Ashvin Agarwal, MS
• director, consultant, and surgeon at Dr. Agarwal’s Eye Hospital,
Chennai, India
• +91 9840430100; agarwal.ashvin@gmail.com; Twitter @AgarwalJR


