Charles Kelman, MD, developed his phaco technique in the secluded OR No. 4 at the Manhattan Eye, Ear, and Throat Hospital in New York. By the time I arrived in 1978 to begin my training, Dr. Kelman had already moved to Lydia E. Hall Hospital, but he left behind his scrub and machine technicians, Louise and Lloyd. At that time, Manhattan Eye and Ear was mostly an intracapsular hospital, and I begged to operate with the few attendings who could perform phacoemulsification. When those surgeons were not available, I leaned on Louise and Lloyd. Tucked in that same OR No. 4, I performed my first phaco cases, assisted by Dr. Kelman’s team.
MACHINE AND TECHNIQUE
I never used the original silver phaco machine; that device was before my time. Instead, I performed my first phaco cases on the Cavitron 7007, the blue box. Louise assembled the handpiece by sliding each O-ring into position, and then, we tuned the handpiece manually. I activated the power by depressing the pedal into foot position 3, and Lloyd turned a dial. We watched a needle jump back and forth on a meter, and the handpiece was tuned when the needle was at its peak. The machine had one level for power and two settings for aspiration. I/A Min was used with the large-bore phaco handpiece, and I/A Max was used with the small-bore I/A handpiece.
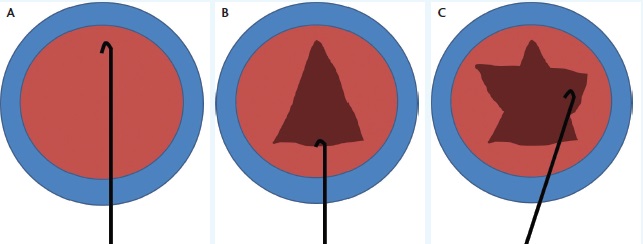
Figure 1. The can opener capsulotomy. The surgeon places a blunt cystotome on the distal anterior capsule and engages the anterior capsule, while being careful not to tear into it (A). By pulling on the anterior capsule with the blunt cystotome, the surgeon makes an ever-widening capsulotomy known as the Christmas tree (B). Additional relaxing incisions are made on either side to open the anterior capsule enough to eliminate any impediment to prolapsing the nucleus (C).
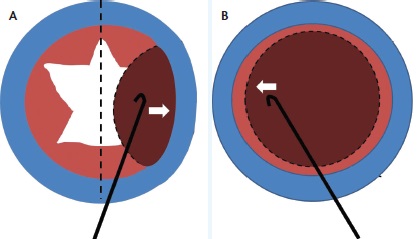
Figure 2. To prolapse the nucleus, the surgeon rocks it more than halfway across the eye, while watching as the equator of the lens crosses the midline of the pupil (A). As the nucleus rocks back, the cystotome releases pressure and coaxes the nucleus into the anterior chamber for emulsification. This was before viscoelastics were used (B).
I created a Christmas-tree capsulotomy by putting a blunt cystotome on the lens and tearing off the capsule. I watched the capsulotomy widen as it approached the incision. I made two additional side cuts to prolapse the nucleus (Figure 1). Using the same cystotome, I rocked the nucleus more than halfway across the eye—a terrifying step at first (Figure 2). When the equator of the nucleus crossed the midline, the capsule’s flaps unfolded, and if the pupil was large, the nucleus popped out. For eyes with small pupils, I spun the nucleus into the anterior chamber using the aptly named “tire-iron maneuver.”
There were no viscoelastics at the time, so I learned to aim a little down to hold the nucleus close to the iris and prevent it from bumping into the cornea. Eventually, great teachers like Robert Sinskey, MD, and Richard Kratz, MD, helped me get out of the anterior chamber and away from the cornea. Dr. Sinskey taught me how to perform phacoemulsification in the posterior chamber, and Dr. Kratz taught me to use two hands.1,2 Unfortunately, I learned more than I wanted about busted capsules, dropped nuclear chunks, vitreous to the incisions, and cystoid macular edema. Critics claimed surgeons in training would blind 50 eyes before attaining proficiency. This did not happen, but we surgeons learning this new procedure did struggle.
Patients could be fit with aphakic spectacles or contact lenses 1 to 2 days postoperatively, or the incision could be opened to 6 mm for the implantation of an anterior chamber IOL, a Binkhorst two-loop capsular fixation IOL, or a Shearing J-loop posterior chamber IOL.
REFINEMENTS AND BREAKTHROUGHS
Phaco machines became more refined to keep up with surgeons’ technical improvements. Handpieces came packaged, assembled, and sealed for sterilization and no longer had to be dismantled in between cases. As they became automatically tuned, dials and the meters disappeared.
I/A Min and I/A Max were abandoned in favor of linear control. After the development of linear vacuum came linear power, and finally, dual-linear controls allowed ophthalmologists to finesse vacuum and power in real time during surgery. Manufacturers experimented with various pumps. Some machines still used the peristaltic pump. Others used a diaphragm, Venturi, or rotary vane pump. Engineers programmed software to allow surgeons to use pulses, micropulses, ascending and descending waves of power, and more options than most people could master in a lifetime.
Surgical technique had to keep pace with the versatility of the phaco machines. It evolved from anterior chamber phacoemulsification to one-handed posterior and then to two-handed posterior chamber phacoemulsification. Howard Gimbel, MD, taught me that bowling out the nucleus facilitated making segments of the rim, and John Shepherd, MD, showed me that grooving two long trenches might make it even easier.3,4 Kunihiro Nagahara, MD, taught me that chopping was more efficient than separating.5 Every possible combination of dissecting, grooving, bowling, chopping, flipping, and rotating has been tried, and they all contributed to the same end result—manual fragmentation of the cataract so that the machine did not have to work as hard. Small pieces are more gently removed than large ones.
CONCLUSION
Today, phacoemulsification is a magnificent and popular operation that is now challenged by laser cataract surgery. The extraordinary adventure continues.n
1. Kratz RP, Colvard DM. Kelman phacoemulsification in the posterior chamber. Ophthalmology. 1979;86(11):1983-1984.
2. Sinskey RM, Cain W Jr. The posterior capsule and phacoemulsification. J Am Intraocul Implant Soc. 1978;4(4):206-207.
3. Gimbel HV. Divide and conquer nucleofractis phacoemulsification: development and variations. J Cataract Refract Surg. 1991;17(3):281-291.
4. Shepherd JR. In situ fracture. J Cataract Refract Surg. 1990;16(4):436-440.
5. Nagahara, K. Phaco chop. Video presented at: The American Society of Cataract and Refractive Surgery; May 8-12, 1993; Seattle, WA.
Paul S. Koch, MD
• founder and medical director of Koch Eye Associates in Warwick, Rhode Island
• (401) 738-4800; paulkoch@kocheye.com


