
Technological innovation continues to refine cataract surgery and refractive lens exchange to provide increasingly successful and customized outcomes. Anesthesia techniques to ensure patient comfort and cooperation during these procedures, however, have not kept up with other surgical advances.
As phacoemulsification gradually supplanted extracapsular cataract extraction, retrobulbar anesthesia was replaced by topical anesthesia with IV sedation. Since the latter became the accepted technique for lensectomy surgery, innovations have consisted of different recipes for IV medications to keep patients calm and comfortable. Most of the formulations include an opioid medication, typically fentanyl. A recent single-center retrospective study at Duke University of 3,764 procedures (2,659 patients) found that at least one dose of fentanyl was used in most cases (3,649 or 96.9%).1 Cataract surgeons probably do not consider themselves significant contributors to the opioid epidemic, but they can help fight it by exploring alternatives to an IV medication that includes fentanyl.2-6
ADMINISTRATION OF SUBLINGUAL SEDATION
The establishment of IV access is one of the greatest pain points in lensectomy surgery. Administering medications sublingually can safely and effectively provide sedation without this pain point. The MKO Melt (ImprimisRx/Harrow Health) was developed for lensectomy surgery but has been used widely outside of ophthalmology. This opioid-free sublingual troche is a compound of 3 mg midazolam, 25 mg ketamine, and 2 mg ondansetron. Once dissolved, it provides sedation, mild amnesia, some analgesia, and an antinausea effect. More than 35,000 of my patients have received MKO Melt, and it has become a part of my daily practice.
Effect and recovery. The product’s effects become evident in 4 to 5 minutes. The peak effect occurs in 15 to 20 minutes. The duration of effect is 1 to 1.5 hours after administration. Recovery time from the sublingual troche is similar to that for IV sedation. Patients leave the surgery center with the assistance of a nurse soon after the procedure concludes.
Dosage. There is a learning curve to using MKO Melt. Administering the proper dose and correctly timing its delivery are critical. Patients must receive a sufficient dose before entering the OR. It is hard, if not impossible, to supplement sedation with another MKO Melt. Dosing is based primarily on patient age, but their size and comorbidities are also considered. Ideally, the patient receives the medication approximately 20 minutes before surgery, allowing the peak effect to occur and the individual’s sedation level to be assessed before they enter the OR.
If a patient is still anxious or if they are overly sedated and somnolent, I take hold of their hand and talk to them. I encourage anxious patients by calmly saying something like the following, “What you’re experiencing is normal. Your surgery is going great. You’re doing a great job. You’re going to feel an increase in pressure. The lights may dim now. Not too much longer. You did it!” I ask somnolent patients to squeeze my hand. This allows me to assess if they are drifting into a deeper plane of consciousness, in which case I speak forcefully to them to keep them awake and present. If these measures do not work, the IV delivery of additional medication for anxiety and a partial dose of reversal for somnolence is started.
Efficacy. A large phase 2 FDA-monitored study compared the efficacy of a combination of midazolam and ketamine (Melt Pharmaceuticals), midazolam alone, ketamine alone, and placebo.7 Procedural sedation was not achieved in 19% of patients who received both midazolam and ketamine versus 36% of patients who received midazolam or ketamine alone and 65% who received placebo (Figure).
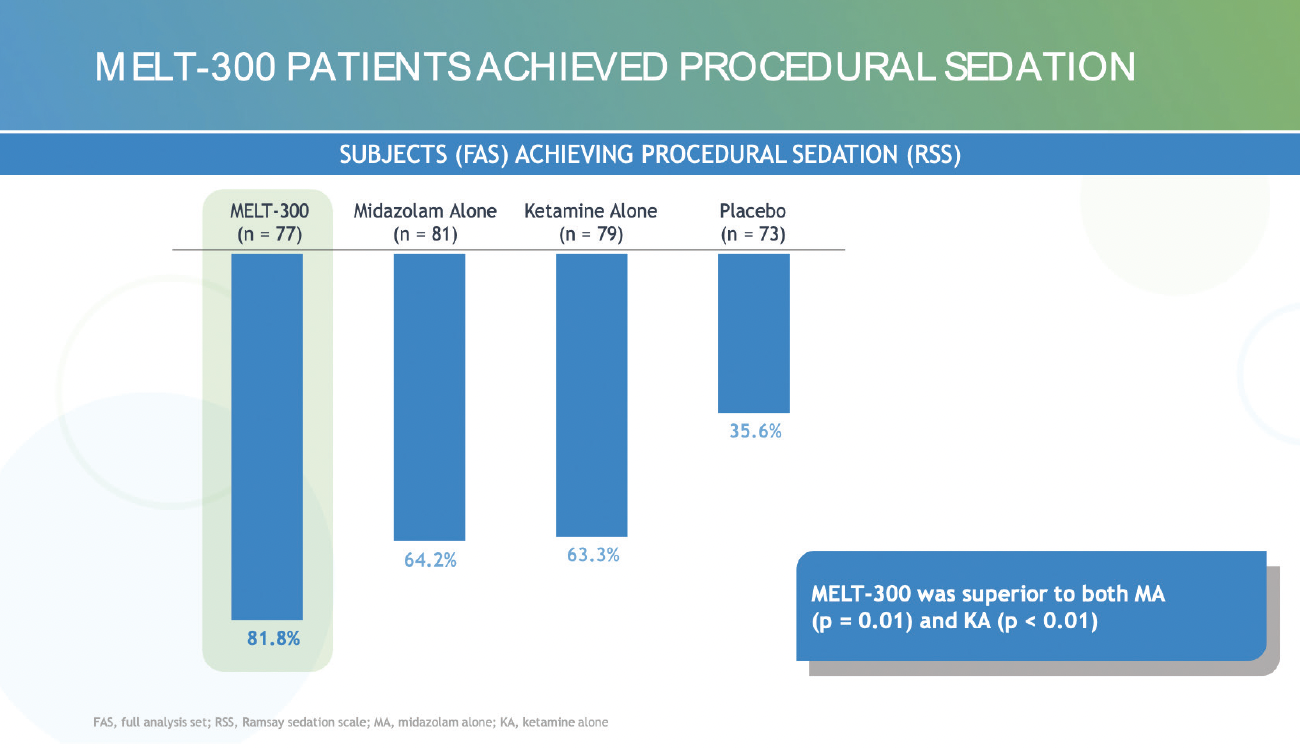
Figure. More patients achieved procedural sedation with Melt-300 versus midazolam alone, ketamine alone, and placebo.
IV intervention. IV access is established in patients who have comorbidities that necessitate it and in those whose anxiety is so great that they are unlikely to get through surgery without additional intervention. A veto rule for MKO Melt is used where I practice: An IV is started if the surgeon, preoperative nurse, or anesthesia staff notices something that may necessitate IV intervention. I start IVs preoperatively on roughly 5% of patients undergoing refractive, cataract, corneal, glaucoma, and combined surgeries, but IV medication is delivered to only approximately 1%.
PATIENT EXPECTATIONS AND EXPERIENCE
Setting realistic expectations before the day of surgery is highly beneficial. Patients should understand that they will not be asleep during surgery. They are instructed that they will see strange lights and feel mild pressure but not pain.
One benefit of sublingual sedation I have noticed is a smoother overall patient experience because the medication can be delivered earlier in the preoperative process. Staying ahead of anxiety is akin to staying ahead of pain. Administering anxiolytic medications when a patient is calm helps them remain calm. A greater amount of anxiolytic medication is required to achieve the same effect if the drug is not administered until after a patient becomes anxious.
1. Davidson RS, Donaldson K, Jefferies M, et al. Persistent opioid use in cataract surgery pain management and the role of nonopioid alternatives. J Cataract Refract Surg. 2022;48(6):730-740.
2. Donnenfeld ED, Mychajlyszn D, Mychajlyszyn A, Stein R. Pain control and reduction of opioid use associated with intracameral phenylephrine/ketorolac 1.0%/0.3% administered during cataract surgery. J Cataract Refract Surg. 2022;48(7):759-764.
3. Visco DM, Bedi R. Effect of intracameral phenylephrine 1.0%–ketorolac 0.3% on postoperative cystoid macular edema, iritis, pain, and photophobia after cataract surgery. J Cataract Refract Surg. 2020;46(6):867-872.
4. Donnenfeld ED, Shojaei RD. Effect of intracameral phenylephrine and ketorolac 1.0%/0.3% on intraoperative pain and opioid use during cataract surgery. Clin Ophthalmol. 2019;13:2143-2150.
5. Hovanesian JA, et al. Intracameral phenylephrine and ketorolac during cataract surgery to maintain intraoperative mydriasis and reduce postoperative ocular pain: integrated results from 2 pivotal phase 3 studies. J Cataract Refract Surg. 2015;41:2060-2068.
6. Davidson RS, Donaldson K, Jeffries M, et al. Persistent opioid use in cataract surgery pain management and the role of non-opioid alternatives. J Cataract Refract Surg. 2022;48(6):730-740.
7. Berdahl JP, Levenson JH, Nordlund M, et al. Sublingual midazolam and ketamine for surgical sedation: a multicenter, double-masked, randomized controlled trial. Paper presented at: ASCRS Annual Meeting; May 5, 2023; San Diego.




