I have encountered several patients over the age of 40 years who received phakic IOLs (Visian ICL, STAAR Surgical) many years ago and now present for a cataract evaluation. Surgeons have mixed opinions on how to approach this situation. Many oppose the use of a femtosecond laser in these cases because they are unsure if the presence of an additional media opacity (ie, the phakic IOL) can impede the normal function of the laser. I shared this attitude earlier in my career when I had less experience using a femtosecond laser. After gaining more proficiency with laser cataract surgery, I began using the femtosecond laser even for patients with phakic IOLs. My transition, however, was not without a hitch, and my approach has evolved.
EARLY EXPERIENCE
Initially, I took a conservative approach to performing laser cataract surgery on eyes with a Visian ICL. The patient was first taken into the OR, the phakic IOL was explanted, the OVD was carefully removed with irrigation and aspiration, and a temporary suture was placed in the main corneal incision. Next, the patient was moved into the laser suite, the laser was docked, and the capsulotomy and lens fragmentation were performed. The patient was then returned to the OR, the surgical field was resterilized, the drape was replaced, the suture was removed, and cataract surgery was performed.
The trips back and forth between the OR and the laser suite wasted a lot of time and supplies. The risk of infection also increased because the patient and I were moving between sterile and unsterile settings. Moreover, incomplete removal of the OVD could prevent the laser from operating properly. Leakage from a freshly created incision secured by a single suture raised the chance of an unstable anterior chamber.
Over time, I became fed up with this cumbersome approach to surgery, and I resumed performing routine manual cataract surgery without use of the femtosecond laser on patients who had a Visian ICL.
A CHANGING ATTITUDE
Soon after switching back to routine cataract surgery, I started to reconsider the advantages of laser cataract surgery for this patient population. In younger individuals, for example, the strength, thickness, and elasticity of the anterior and posterior capsules can make performing the capsulorhexis and centering it on the visual axis more difficult, and there can be an increased risk of an errant tear. In contrast, I can consistently achieve nearly perfect centration of a laser capsulotomy, which is important because many of these patients have a high angle kappa due to high myopia or keratoconus. Centration is also essential when a patient is receiving a multifocal IOL.
Many of these patients, moreover, receive arcuate incisions or a toric IOL to correct significant corneal astigmatism at the time of cataract surgery, and I prefer to use a femtosecond laser for these procedures. The IntelliAxis Refractive Capsulorhexis (Lensar) marks the steep axis on the capsule to help achieve accurate toric IOL alignment. I find that laser arcuate incisions help me to correct small amounts of astigmatism (as low as 0.50 D) and thus optimize refractive outcomes. A manual approach does not allow me similar fine-tuning capabilities.
Eventually, I decided to perform laser cataract surgery through the ICL. To date, I have performed several of these cases successfully (see Case Examples).
CASE EXAMPLES
Case No. 1
A 56-year-old woman presented with a cataract in her left eye. The patient had undergone bilateral implantation of a Visian ICL (STAAR Surgical) 20 years earlier to treat high myopia. A slit-lamp examination found grade 0.5 vault of the ICL in the left eye. The cataract was characterized by 2+ to 3+ anterior subcapsular haze. Her UCVA was 20/150 OS, and her BCVA was 20/40 with a manifest refraction of plano -3.00 x 022º OS. The axial length was 27.41 mm OS, and the eye had 2.00 D of corneal cylinder.
I planned to perform the femtosecond laser portion through the ICL, explant the ICL, and then complete cataract surgery with implantation of a toric IOL in the left eye.
A femtosecond laser was used to perform the capsulotomy and create the clear corneal incision (see video below). The IntelliAxis Refractive Capsulorhexis (Lensar) was used to mark the steep axis at 105º. The borders of the phakic IOL and cataract not captured by the femtosecond laser system were manually identified and demarcated.
Femtosecond Laser Capsulotomy and Clear Corneal Incision
A femtosecond laser was used to perform a capsulotomy and create a clear corneal incision.
In the OR, the eye was filled with a generous amount of a dispersive OVD. A nucleus manipulator with an olive-shaped tip was used to disengage the four haptic footplates from underneath the iris. An additional amount of an OVD was injected underneath the ICL to separate it from the underlying capsulotomy. Grasping forceps were used to pull the edge of the ICL and footplate junction and to gently draw the ICL out of a 2.75-mm temporal corneal incision. The lens was removed, and trypan blue dye was used to stain the anterior capsule, revealing a 360º capsulotomy.
Cataract surgery was completed in a normal fashion. A +7.50 D monofocal toric lens (enVista, Bausch + Lomb) was inserted into the bag and rotated to the correct axis. The patient’s UCVA and BCVA were 20/30 with a nearly plano refraction at 1 month postoperative.
Case No. 2
A 56-year-old woman presented with a cataract in the left eye (Figure). The patient had a history of high myopic astigmatism and keratoconus in each eye. She had received intrastromal corneal ring segments (ICRSs; Intacs, CorneaGen) in each eye in 2006 and a Visian ICL in the left eye in 2009.
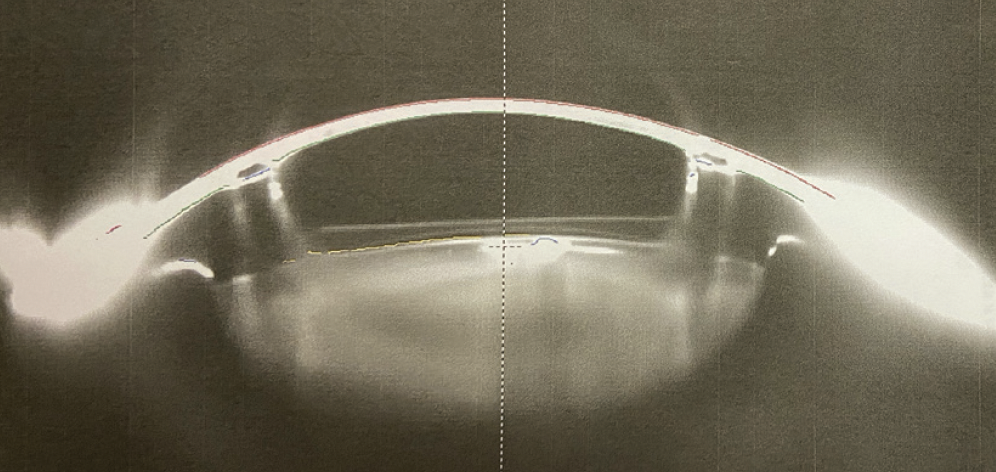
Figure. Scheimpflug image of the eye from Case No. 2 showing the shallow ICL vault and well-centered ICRSs.
At the slit lamp, the ICRSs were well centered at 7 mm, and the ICL was noted to have a grade 0.5 vault. The cataract was characterized by 2+ to 3+ anterior subcapsular haze and 2+ to 3+ nuclear sclerosis. Her UCVA was 20/200 OS, and her BCVA in that eye was 20/25 with a manifest refraction of -3.25 -1.25 x 100º. Axial length in the left eye was 30.23 mm. The keratometry readings were 50.50/51.70 D.
Removal of the ICL was planned in combination with laser cataract surgery and the implantation of a monofocal IOL in the left eye. Slight myopia (-0.50 D) was targeted based on the patient’s history of keratoconus, and the Barrett II formula was used for the IOL power calculation.
A femtosecond laser was used for the capsulotomy and grade 1 lens fragmentation (see video below). The clear corneal incision function was turned off because of the presence of ICRSs, the location of which was peripheral enough not to obstruct the pathway of the laser. The borders of the ICL and cataract not captured by the laser system were manually identified and demarcated.
Femtosecond Laser Capsulotomy and Lens Fragmentation
A femtosecond laser is used for capsulotomy and grade 1 lens fragmentation.
In the OR, the eye was filled with a generous amount of a dispersive OVD. Like in Case No. 1, a nucleus manipulator with an olive-shaped tip was used to disengage the four haptic footplates from underneath the iris. An additional amount of an OVD was injected underneath the ICL to separate it from the underlying capsulotomy. Grasping forceps were used to pull the edge of the ICL and footplate junction and to gently extract the ICL through a 2.75-mm temporal corneal incision. The phakic IOL and free-floating anterior capsulotomy were removed. The anterior capsule was not stained because the capsulotomy appeared to be complete.
Cataract surgery was completed in the normal fashion. A -7.00 D Sensar IOL (model AR40M, Johnson & Johnson Vision) three-piece monofocal lens was inserted into the bag. The patient’s UCVA and BCVA were 20/30 at 1 month postoperative.
SURGICAL PEARLS
In my experience, there are two main challenges to performing laser cataract surgery on an eye with a Visian ICL. First, the phakic IOL is often located close to the cataract, especially in cases of a shallow ICL vault due to ICL undersizing, making it difficult for the laser system to differentiate the IOL from the cataract and to identify the posterior border of the ICL and the anterior border of the cataract. Sometimes, the system sees these as one structure and cannot identify any of them. I often must manually delineate the borders with the outlining tools provided by the laser platform. I can do this on all the frames. The platform can then successfully reconstruct a 3D image to perform the appropriate treatment.
Second, the phakic IOL disperses some laser energy. As a result, the laser capsulotomy and lens fragmentation may be incomplete. After encountering this situation a few times, I worked with my Lensar representative to adjust some of the energy and pulse-spacing settings on my system to achieve a more efficient and complete capsulotomy. I also recommend decreasing the fragmentation energy because many of these patients have anterior subcapsular cataracts, which are absent of any real hardening or nuclear sclerosis. Excess energy can increase adherence between the phakic IOL and the anterior capsule. I also inject a generous amount of an OVD within the plane between the ICL and the anterior capsule to loosen the lens as much as possible before pulling out the phakic IOL.
If, despite the aforementioned adjustments, the capsulotomy is incomplete, Utrata forceps are used to complete the capsulotomy manually. I can usually see the laser imprint of the anterior capsulotomy on the ICL itself once removed, which illustrates just how close the phakic IOL sits anterior to the lens—a known risk factor for cataract development—in some of these cases. (See video below.)
The danger with an incomplete capsulotomy and a capsule that has adhered to the ICL is that the capsule will be withdrawn with the IOL, which could cause the capsule to tear or the capsulotomy to radialize.
CONCLUSION
Patients who received a Visian ICL can benefit from laser cataract surgery, with the femtosecond laser portion performed through the ICL, provided that some modifications are made and extra care is taken.