Demodex blepharitis is a common yet underappreciated ocular disease that can significantly impact patients as well as the health care system. The prevalence of Demodex blepharitis is estimated to be as high as 25 million in the United States alone,1 but since proper screening is not routine and symptoms are similar to those of other inflammatory ocular surface diseases, it is often overlooked or misdiagnosed.
Disease Impact
Demodex blepharitis is caused by an infestation of Demodex mites on the eyelid. In the Atlas study presented at ARVO in 2021, 80% of patients with Demodex blepharitis reported that the disease negatively affected their daily life.2 More than half (52%) of patients reported experiencing itchy or dry eyes frequently or most of the time, and for many, these symptoms affected daily activities like the ability to drive at night (47%) and time spent conducting daily hygiene routines (30%).2,3 In addition, not only were more than half of patients (51%) experiencing symptoms for more than 4 years, but they were making multiple doctor visits (33% making two or more visits; 15% making six or more visits) for their blepharitis. Fifty-eight percent (58%) of patients in this study were never even diagnosed with blepharitis.3 We can do better to help identify and treat these patients.
Early Diagnosis
Detecting and treating Demodex blepharitis sooner can result in improved patient outcomes. As part of the ASCRS Cornea Clinical Committee, we developed the “LLPP” or “look, lift, pull, and push” algorithm to help surgeons navigate the preoperative diagnosis of ocular surface diseases. If you do this, you are almost certain to find the presence of collarettes in more patients than you may think. Collarettes are an accumulation of keratinized skin cells, mite waste, and eggs and are most easily seen on the upper eyelid when patients are looking down during the slit-lamp examination (Figure).
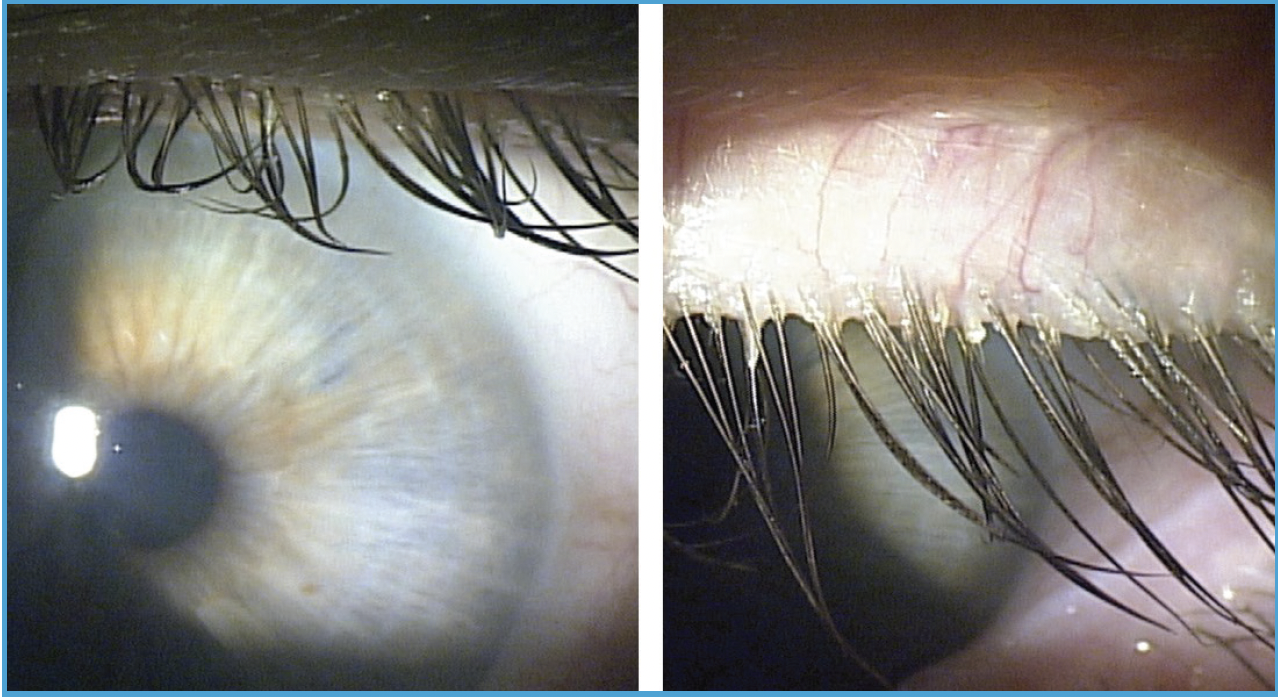
Figure. Look for collarettes during every slit-lamp exam to determine if your patient has Demodex blepharitis. Collarettes are often missed when a patient is looking straight ahead even with lid lift (left); they are easily seen when the same patient is looking down (right).
Identifying Demodex blepharitis early is critical for patient relief and improving surgical outcomes. While the presence of Demodex blepharitis does not cause infection of the eye directly, the bacteria that may accompany the mites and associated collarettes do.4
Treatment Today
Once a patient is diagnosed, there are a limited number of options to manage the disease and no FDA-approved treatments. This is not only troubling for providers, but it can be discouraging for patients, who are likely still trying to process the shock and psychological impact of having a mite infestation on their eyelids that may also be causing redness or an inability to wear make-up.
In my practice, I typically prescribe a combination of lid scrubs, overnight lid ointments, anti-infectives, and microblepharoexfoliation procedures, in addition to other treatments for co-morbid ocular surface disease subtypes like dry eye disease or Meibomian gland disease. I’ve found that patient tolerability, compliance, and satisfaction with these treatments are relatively low, and none of them satisfactorily address the root cause of the disease—the Demodex mite infestation. Fortunately, there is a new treatment in development that looks encouraging.
Future Treatment
Tarsus Pharmaceuticals, Inc., is developing an investigational therapeutic, TP-03 (lotilaner ophthalmic solution, 0.25%), that is designed to eradicate Demodex mites by inhibiting parasite specific GABA-CI channels. TP-03 met all primary and secondary endpoints with clinically meaningful results and high statistical significance (P < .0001) in a Phase 2b/3 pivotal trial (Saturn-1)5, and Tarsus is currently enrolling patients in a second pivotal trial (Saturn-2).
Demodex blepharitis presents a significant burden to patients and the health care system, but the good news is that it is relatively easy to identify by having patients look down and checking for collarettes during every slit-lamp exam. More education and awareness about the prevalence, impact, and diagnosis of this disease are needed, but, with proper screening protocols in place, we can see the problem that has been hiding in plain sight—and thus improve care for our patients.
1. Sadri E, Yeu E, Trattler W, Holdbrook M, Baba S. The prevalence of collarettes and Demodex blepharitis in ophthalmology and optometry practices. Presented at: ASCRS 2021. Abstract 75009.
2. Elizabeth Yeu, Mark J. Holdbrook, Stephanie N. Baba, Paul J Gomes; Psychosocial Impact of Demodex Blepharitis. Invest Ophthalmol Vis Sci. 2021;62(8):1261. Presented at ARVO 2021.
3. Scott Schachter, Elizabeth Yeu, Mark J. Holdbrook, Stephanie N. Baba, Paul J Gomes. Clinical Manifestations of Demodex Blepharitis. Invest Ophthalmol Vis Sci. 2021;62(8):1268.
4. Yan Y, Yao Q, Lu Y, et al. Association Between Demodex Infestation and Ocular Surface Microbiota in Patients With Demodex Blepharitis. Front Med (Lausanne). 2020;7:592759. Published 2020 Nov 4. doi:10.3389/fmed.2020.592759
5. Yeu E, Baba S, Holdbrook M, Wirta, D. Safety and Efficacy of Topical Lotilaner 0.25% for the Treatment of Demodex blepharitis: Results of the Saturn-1 Ph 2b/3 FDA-Pivotal Trial. Presented at: ASCRS 2021. Abstract 75012.

