There are more than 140 species of mites, but only Demodex folliculorum and Demodex brevis exist in humans.1-5 Demodex mites tend to accumulate on the face, cheeks, forehead, nose, and external ear canal, where sebum excretion may provide a favorable habitat for breeding.1,4 The anatomical features of the eyelids can also create a favorable environment for Demodex mites to spread and flourish, which can lead to lid margin infection, ocular surface irritation, and symptoms of ocular discomfort such as itching, foreign body sensation, and stinging.2,3,6 Chronic infestation of the eyelids by Demodex mites may cause inflammation of the eyelid or ocular surface and secondary bacterial infection.1,2,5
Several studies have shown a significant increase in the incidence of Demodex mite infestation in the eyelashes of individuals with chronic blepharitis compared with healthy individuals. The exact pathogenesis of chronic blepharitis, however, remains unclear. With few cross-sectional observational studies investigating the prevalence of Demodex mites in healthy individuals and no FDA-approved medications currently available, identifying and treating Demodex blepharitis has been exceedingly challenging. As of this writing, the most common treatments for demodicosis include tea tree oil products and ivermectin.2 Tea tree oil products are widely used. It is worth noting, however, that a recent Cochrane review found that their efficacy for the treatment of demodicosis is uncertain,7 and Chen et al reported that tea tree oil might be harmful to the human meibomian gland epithelial cells in vitro.8 Our study sought to provide information on the identification and treatment of Demodex blepharitis.
RESEARCH
Study design. We conducted a cross-sectional, nonrandomized prospective study at two large tertiary care medical centers in New York (one urban and one suburban; N = 199). We investigated the prevalence of Demodex mites among all patients presenting to general and subspeciality outpatient ophthalmology clinics at these two centers and identified comorbid conditions and risk factors associated with chronic blepharitis in affected individuals. We also set out to design and build a model to predict the incidence of Demodex in individuals presenting with the risk factors we identified.
We collected relevant data such as the duration of dry eye/blepharitis syndrome, demographics, use of medications, surgical history, previous ocular treatments aimed at improving dry eye/blepharitis syndrome, and use of over-the-counter cosmetic products. Examination findings recorded included dry eye disease (DED), blepharitis, pterygium, use of eye makeup, and the presence of Demodex mites on epilated eyelashes (one from each lid).
Results. We identified 123 patients with blepharitis, and Demodex mites were identified in 68% of them. Patients with blepharitis practiced lid hygiene twice as often as those without blepharitis, suggesting that the former’s symptoms prompted them to seek help or to change their daily routines. Among the 84 patients with blepharitis thought to be associated with Demodex, only one (1%) was receiving adequate management targeted to the pathology. In agreement with prior studies, we found a positive and linear correlation with age. Strong correlations were also observed between the presence of Demodex and a history of pterygium surgery, blepharitis, DED, and dermatochalasis.
Discussion. Validating our results, the Titan study, a retrospective chart review of 1,032 patients seen for any reason at six eye care clinics across the country, was also presented at this year’s ASCRS meeting.9 Sadri et al reported that collarettes, the pathognomonic sign of Demodex blepharitis, were present in 58% of patients, similar to the prevalence of DED, and that 69% of blepharitis patients had Demodex, similar to our finding of 68%. Among patients using prescription medications for the treatment of DED, 60% still had collarettes. Both our study and the Titan study identified a largely underdiagnosed cohort of patients who were experiencing Demodex blepharitis with an inadequate management of disease.
ALGORITHM FOR PREDICTING RISK
Visualizing Demodex mites requires epilation of the eyelashes and direct observation under light microscopy, both of which are impractical and time-consuming at most clinics. In an effort to streamline diagnosis, we leveraged the data collected in our study to develop a predictive calculator to determine the likelihood of any one patient’s having Demodex (Figure). The calculator is available online at www.DoIHaveDemodex.com. Demodex activity can then be confirmed in these patients at the slit lamp by looking for collarettes.
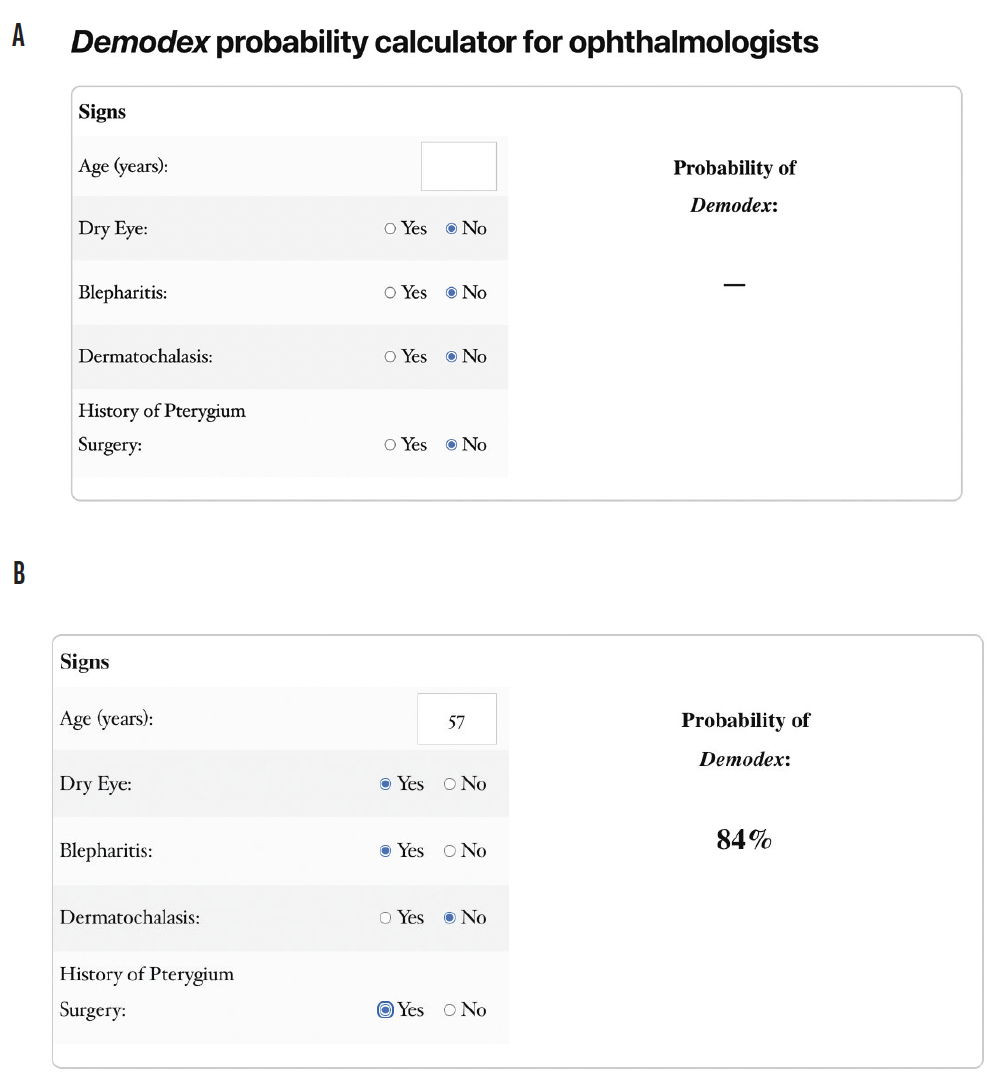
Figure. The Demodex probability calculator (A) and a sample risk probability calculation (B). The calculator is available at www.DoIHaveDemodex.com.
Source: www.DoIHaveDemodex.com
CONCLUSION
Identifying and treating Demodex mites in patients with associated blepharitis and DED can provide them with symptomatic relief. Studies such as ours clearly demonstrate the need for innovative, effective, and safe treatments that address the root cause of blepharitis.
1. Kheirkhah A, Casas V, Li W, Raju VK, Tseng SCG. Corneal manifestations of ocular Demodex infestation. Am J Ophthalmol. 2007;143(5):743-749.
2. Navel V, Mulliez A, d’Azy CB, et al. Efficacy of treatments for Demodex blepharitis: a systematic review and meta-analysis. Ocul Surf. 2019;17(4):655-669.
3. Randon M, Liang H, Hamdaoui ME, et al. In vivo confocal microscopy as a novel and reliable tool for the diagnosis of Demodex eyelid infestation. Br J Ophthalmol. 2015;99(3):336-341.
4. Zhong J, Tan Y, Li S, et al. The Prevalence of Demodex folliculorum and Demodex brevis in cylindrical dandruff patients. J Ophthalmol. 2019;8949683. doi: 10.1155/2019/8949683
5. Zhu M, Cheng C, Yi H, Lin L, Wu K. Quantitative analysis of the bacteria in blepharitis with demodex infestation. Front Microbiol. 2018;9:1719.
6. Bhandari V, Reddy JK. Blepharitis: always remember Demodex. Middle East Afr J Ophthalmol. 2014;21(4):317-320.
7. Savla, K., Le, J.T., and Pucker, A.D. Tea tree oil for Demodex blepharitis. Cochrane Database Syst Rev. 2020;6(6):CD013333.
8. Chen D, Wang J, Sullivan DA, Kam WR, Liu Y. Effects of Terpinen-4-ol on Meibomian Gland Epithelial Cells In Vitro. Cornea. 2020;39(12):1541-1546.
9. Sadri E, Yeu E, Trattler W, Holdbrook M, Baba S. The prevalence of collarettes and Demodex blepharitis in ophthalmology and optometry practices. Paper presented at: American Society of Cataract and Refractive Surgeons Annual Meeting; July 23–27, 2021; Las Vegas, Nevada.