In recent years, patient expectations regarding cataract surgery have evolved. Spectacle dependence after surgery is no longer satisfactory for many patients. Correcting astigmatism—even small amounts—is one strategy to give patients what they want. One way to achieve this is with the use of femtosecond laser arcuate incisions as part of laser cataract surgery.
DETERMINING CORNEAL ASTIGMATISM
Evaluating the nature of astigmatism is a crucial step in ensuring the desired refractive outcome. Any remnants of astigmatism, even as low as 0.50 D, can leave the patient with glare, halos, or blurry vision. We must determine whether the patient has regular astigmatism and rule out other pathologies such as dry eye disease or blepharitis, epithelial basement membrane disease, corneal scars, Fuchs corneal dystrophy, or keratoconus.
To quantify astigmatism, I obtain three reference metrics for comparison, making sure to maintain consistency within the devices used on each patient (within 0.50 D and 10° of axis): Placido-ring topography with the Atlas 9000 Corneal Topography System (Carl Zeiss Meditec), anterior and posterior corneal astigmatism with the Galilei topographer (Ziemer Ophthalmic Systems), and optical biometry measurements of the magnitude and axis of astigmatism with the Lenstar LS 900 (Haag-Streit) or IOLMaster 700 (Carl Zeiss Meditec).
CASE EXAMPLE
One benefit of femtosecond laser penetrating incisions is the ability to titrate their magnitude postoperatively. One of our patients started with 1.88 D astigmatism at 97°. Based on our current nomogram, we performed two penetrating incisions, 40° in length, at 97°. At 3 weeks postoperative, the patient still had approximately 1.00 D astigmatism and complained of blurred vision. After applying numbing drops, we opened the incisions at the slit lamp. When the patient returned 3 weeks later, UCVA was 20/20, and residual cylinder was approximately 0.50 D (Figure).
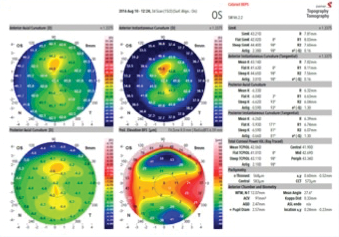
Figure. Postoperative topography maps demonstrating the effect of penetrating incisions on correcting astigmatism in this case.
If the patient has a low magnitude of astigmatism, up to about 1.25 D with-the-rule or 0.80 D against-the-rule, astigmatic keratotomy (AK) or peripheral corneal relaxing incisions are my preferred method of correction.1 For any higher magnitude, many studies have shown us that correcting astigmatism with toric IOLs is the way to go.2-4
MANUAL VERSUS LASER
Before introducing laser cataract surgery into my practice, I performed a high volume of manual AKs. The difficulty with manual incisions arises from their unpredictable outcomes: A diamond blade does not produce a perfect arcuate shape, and manual incisions can be subject to wound gape, infection, scarring, epithelial inclusions, and corneal perforations.
The use of laser AKs allows us to consistently achieve precise cuts (both penetrating and intrastromal) with respect to depth, length, and centration, and it also significantly reduces the risk of corneal perforation, wound gape, and patient discomfort.5
PENETRATING VERSUS INTRASTROMAL
Penetrating incisions pierce the corneal epithelium, whereas intrastromal cuts leave about 20% of the anterior cornea (epithelium and stroma) and 20% of the posterior corneal (stroma and endothelium) untouched. We have observed that intrastromal incisions are more comfortable for patients and produce less inflammation, wound gape, and corneal perforation; however, there is a lack of studies demonstrating how effective they are at correcting astigmatism and how stable the correction is in the long term.
Studies comparing effectiveness and long-term stability in penetrating and intrastromal incisions are limited. I am involved in an ongoing study designed to show the effects of penetrating versus intrastromal incisions performed in conjunction with cataract surgery in patients with low magnitudes of corneal astigmatism. In the study, patients undergo cataract extraction and IOL placement along with astigmatism correction using the Catalys Femtosecond Laser System (Johnson & Johnson Vision). Patients are randomly assigned by research coordinators to penetrating incisions in one eye and intrastromal incisions in the other; the investigator is not masked. Outcomes are measured at 3 weeks and 1 year postoperatively in patients who have achieved a BCVA of 20/30 or better after the procedure.
Currently, 38 eyes have received intrastromal incisions and 29 have received penetrating incisions. The results described here are based on 3-week data; patients have not yet reached the 1-year mark for long-term outcome comparison. To measure effectiveness, we compared preoperative corneal astigmatism to postoperative manifest refraction astigmatism. Our results are described in the accompanying sidebar above.
Penetrating Versus Intrastromal Incisions
Intrastromal Incisions
Preoperative
- 25% of eyes had 0.50 D astigmatism or less
- 42% of eyes had less than 0.75 D astigmatism
3 Weeks Postoperative
- 72% of eyes had less than 0.50 D astigmatism
- 90% of eyes had less than 0.75 D astigmatism
The Bottom Line
Double-angle plots were created to compare vector changes in mean astigmatism as measured with the IOLMaster 700 (Carl Zeiss Meditec):
- Intrastromal incisions created an average 0.57 D decrease in astigmatism; and
- Penetrating incisions created an average 0.61 D decrease in astigmatism.
Penetrating Incisions
Preoperative
- 19% of eyes had 0.50 D astigmatism or less
- 30% of eyes had less than 0.75 D astigmatism
3 Weeks Postoperative
- 89% of eyes had less than 0.50 D astigmatism
- 96% of eyes had less than 0.75 D astigmatism
With only 38 eyes, these numbers are still low, and we cannot state that there is a statistically significant difference between the two procedures. Our goal is ultimately to include 100 patients (200 eyes). However, in the interim, both seem to be comfortable, low-risk methods to produce an effective decrease in cylinder in patients with low degrees of astigmatism.
An excellent nomogram for intrastromal incisions, developed by Julian D. Stevens, MRCP, FRCS, FRCOphth, DO, is available at www.femtoemulsification.com. We do not, however, have a nomogram for penetrating incisions on the Catalys; one purpose of our study is to collect data to develop a nomogram. When completed, our goal is that users will input the magnitude of astigmatism to be corrected, and the nomogram output will be the arc length and vector analysis showing the axis on which to place the cut.
IMPROVING PATIENT OUTCOMES
We have long heard the debate about whether laser cataract surgery produces a meaningful benefit over standard phacoemulsification. My response is that there is a time and place for everything. Software is continually changing and improving the positioning of incisions. Investigators are assessing long-term outcomes, and those outcomes are getting better.
Toric IOLs are the best option for correcting more than 2.00 D astigmatism, but what about lower magnitudes of astigmatism? Femtosecond laser technology offers us a way to deliver the results patients want. It is time to change the discussion around femtosecond lasers from simply yes or no to: “What are the situations in which the patient can benefit?”
1. Al-Mohtaseb Zaina, Culbertson W. Intrastromal astigmatic keratotomy with the femtosecond laser: A nonpenetrating approach for the correction of keratometric and refractive astigmatism. CRST. March 2014.
2. Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: A systematic review and meta-analysis. Ophthalmol. 2016;123(2):275-286.
3. Mingo-Botín D, Muñoz-Negrete FJ, Won Kim HR, Morcillo-Laiz R, Rebolleda G, Oblanca N. Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg. 2010;36(10):1700-1708.
4. Ouchi M. High-cylinder toric intraocular lens implantation versus combined surgery of low-cylinder intraocular lens implantation and limbal relaxing incision for high-astigmatism eyes. Clin Ophthalmol. 2014;8:661-667.
5. Wu E. Femtosecond-assisted astigmatic keratotomy. Int Ophthalmol Clin. 2011;51(2):77-85.