Patients often undergo corneal refractive surgery with the mindset that it will be a sort of magic solution for everything related to their vision throughout the rest of their lifetimes. This thought process often extends beyond vision disorders and into eye health. The lay public has somehow come to believe that LASIK is the solution for everything related to eyes—from myopia to presbyopia, and even including totally unrelated conditions such as strabismus and glaucoma.
Have you encountered the phenomenon in a social setting when you tell someone you’re an ophthalmologist and the first question asked is: “Do you do LASIK?” LASIK is to ophthalmology what Xerox is to copy machines and Kleenex is to facial tissues. Everyone knows about it … or they think they do.
So it should come as no surprise when patients come in and say something like: “My LASIK is wearing off.” When LASIK is the one thing that patients know about ophthalmology, it’s no wonder they come to the incorrect conclusion that LASIK must be the answer to their problems again. They often then have a reasonable followup question: “How many times am I going to need this?”
The answer? Most of the time, they don’t. The average age for LASIK has historically been from the mid-30s up. We know that when patients return unhappy with their vision about 10 years after a LASIK procedure, the chief suspects are presbyopia and cataract. So the answer is: “It’s almost always the lens, not the LASIK.”
THE WORKUP
When we see patients today who had corneal refractive surgery many years ago, they are typically in their late 40s, 50s, or 60s. The workup for them is quite similar to that for any patient seeking refractive surgery, with a few important additions.
The first thing we do, as for any patient, is to obtain a history. An important question is: “What is it about your vision that you wish was better?” We follow this with a comprehensive exam, including manifest refraction, measurement of accommodative amplitude, and corneal topography. Topography allows us to screen for sufficient corneal thickness if we want to go back to the cornea again (for example for blended vision or corneal inlays) and to rule out other rare conditions such as postrefractive surgery keratoconus that may require CXL.
DYSFUNCTIONAL LENS SYNDROME
Important diagnostic modalities that we use for these patients in addition to our routine refractive surgery workup may include measuring objective scatter index (OSI) and performing noninvasive tear breakup time measurement using the HD Analyzer (Visiometrics).
Keeping in mind that aging of the lens is often the culprit, several factors can help us choose whether to steer our management toward a second corneal procedure or a lens-based procedure. Three factors in particular influence this decision: the goals of the patient, the corneal thickness, and the OSI (Figure 1).
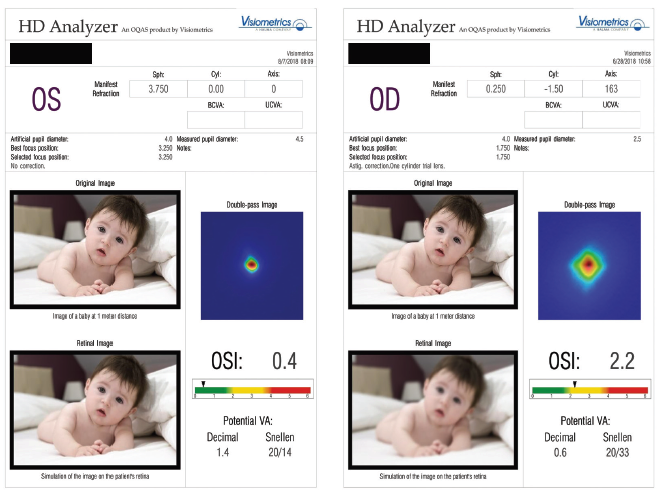
Figure 1. Low (left) and high (right) OSI scores. A low score indicates the presence of stage 1 dysfunctional lens syndrome—a safe stage for corneal surgery. A higher score indicates the presence of stage 2 or stage 3 dysfunctional lens syndrome—stages in which refractive lens exchange and refractive cataract surgery, respectively, may be more appropriate options.
Young patients with early onset of presbyopic stiffening of the lens and an OSI of less than 1.0 have what we consider stage 1 dysfunctional lens syndrome (DLS). In these patients—who are simply experiencing the first onset of presbyopia—we consider returning to the cornea. However, before we proceed with repeat corneal surgery, we always demonstrate blended vision with a contact lens trial to make sure the patient can neurally adapt to a refractive offset.
For patients with higher OSIs and/or thinner corneas, we advise against corneal refractive surgery and either go straight to refractive lens exchange (RLE) or advise patients of a pharmaceutical presbyopia treatment option as a holdover strategy until they’re ready for a bigger step.
When the patient’s OSI is high but visual acuity is correctable to 20/20, the patient is categorized as being in stage 2 DLS. These patients often report worsening of night vision, needing more light to read, and noticing an impact on distance vision quality. We offer lens-based refractive surgery for patients in stage 2 DLS. Importantly, patients are not required to wait until some arbitrary cutoff point, such as decline of BCVA to worse than 20/40.
CHOICE OF IOL
Patients who desire RLE after LASIK are often good candidates for a variety of advanced-technology IOLs—of course depending on the nature of their previous refractive surgery. For example, we have seen great results using extended depth of focus and even low-add multifocal IOLs in patients with previous myopic ablations, especially if they were originally low myopes. We have found that patients who have had higher refractive treatments, particularly hyperopic ablations, may do better with monofocal IOLs or a small-aperture IOL such as the IC-8 (AcuFocus; not available in the United States).
The Three Milestones of Human Vision Development and Their Most Applicable Procedures
Milestone No. 1: Ocular Maturity
- Modern LASIK
- SMILE
- PRK
- Phakic IOL
Milestone No. 2: Presbyopia/Stage 1 DLS
- Corneal procedures
- Refractive lens exchange
- Pharmaceutical options
Milestone No. 3: Cataract Development
- Refractive cataract surgery
We use intraoperative aberrometry with the ORA System with VerifEye+ Technology (Alcon) to achieve results as close to target as possible with the initial IOL procedure, but we have corneal laser vision correction in reserve to fine-tune the refraction if needed after the primary lens surgery.
REPEAT CORNEAL SURGERY
When we go back to the cornea for a second laser vision correction procedure years after an initial LASIK, several options exist. If we have records or evidence of a successful original flap creation, especially if it was made by femtosecond laser, we are comfortable finding the edge of the flap with a Sinskey hook and unzipping the flap edge circumferentially so that we can lift the flap with a Seibel spatula.
Our preference is to do any type of hyperopic or hyperopic cylinder ablation under a flap if possible. If the enhancement needed is a myopic ablation, and/or if the correction is to be done in an eye with a flap from the past and we do not have records, or if the flap was done using a microkeratome, our preference is to use surface ablation with application of mitomycin C.
If we are considering a corneal inlay approach, such as the Kamra (CorneaGen), we perform corneal OCT to measure the earlier flap depth in order to ensure that a pocket created under the previous flap will have at least 100 µm of clearance below and be at least 250 µm from the endothelium below.
SETTING EXPECTATIONS
One of the things I love most about modern refractive surgery is that the number of conditions we are able to help our patients with seems to be ever-expanding. In the past, the definition of refractive surgery started and ended with LASIK and PRK. Today, there are at least eight modern procedures in the comprehensive refractive surgeon’s tool kit to help our patients. This means it is well past time to start educating our young patients differently when they undergo their first refractive surgery.
We have found success educating all our patients, young and old alike, about what Erik L. Mertens, MD, FEBO, first described as the three milestones of human vision development. We add that there is a set of procedures applicable to each milestone. The first milestone is ocular maturity, at which time any one of several procedures—modern LASIK, SMILE, PRK, or phakic IOL—may be the ideal solution for full distance correction. The second milestone is presbyopia (or stage 1 DLS), at which time corneal and lenticular procedures and pharmaceutical options may be appropriate. The benefit of opting for RLE at the second milestone is that it prevents cataracts. If the patient gets to the third milestone, cataract development, before having RLE, then refractive cataract surgery is an effective solution to cure any refractive pathology with a refractive surgery–like outcome for most patients. (See The Three Milestones of Human Vision Development and Their Most Applicable Procedures.)
PUTTING IT ALL TOGETHER
Patients who desire quality of life with the benefits of refractive surgery every waking minute have many options. There are ideal ages and ideal procedures for distance correction, presbyopia treatment, and even cataract, depending on clinical variables. The good news for patients is that refractive surgery options exist for nearly everyone, even those dealing with lenticular changes after age 40 such as presbyopia and cataract. By setting expectations ahead of time and employing all the procedures applicable to each individual clinical situation, refractive and cataract surgeons can achieve success and satisfaction for patients, even when they return years after a LASIK procedure asking for renewed vision.





