

Managing the business of medicine and practicing medicine are, in many ways, symmetric. To diagnose patient problems, doctors gather information, make a treatment decision, suggest treatment options, monitor the results, and repeat the process if the outcome is not satisfactory. Administrators follow a similar sequence to identify and resolve practice problems for their singular patient—the organization itself.
Patients hold doctors accountable for their actions. If their health problems do not resolve, they likely will not return for continued care. Whether patients are unhappy with their medical treatment or the way the staff treated them, they may write a poor online review that damages a practice’s reputation.
Holding yourself accountable for all significant functions of your practice is a keystone to a successful and well-managed organization. How can physician practice leaders and the management team hold each other and the rest of the staff more accountable in your practice? New problems and unexpected trends can be identified promptly when one person owns the responsibility and regularly monitors priority functions throughout the process.
The following bulleted list includes some examples of accountability standards adopted in some of the best practices we see in our consulting efforts.
- Documented annual goals for administrators and managers set clear expectations and provide a platform for reviewing why the goals were achieved (or why not).
- Written performance appraisals for all employees help to specify goals for the next employment year and suggested steps to meet them. Ideally, appraisals are oriented around each employee’s work anniversary date, and any salary increase is directly tied to measured performance (and not an outdated cost-of-living increase).
- For physicians, a board-approved code of conduct helps set standards that identify whether behaviors are acceptable or not in your practice, such as arriving to the clinic on time, following agreed care pathways, and allowing supervisors to apply corrective actions rather than criticizing staff directly.
Creating a culture of accountability takes a full commitment from the management team, including physician leadership. In this article, we outline several practical accountability tools that can help maintain high standards for patient care and business performance in your practice.
TOOL NO. 1: GOAL SETTING
Set clear performance expectations and specific goals for all practice employees and doctors. Just as doctors are accountable to their patients, the management staff of a practice is accountable to the organization itself. By having clear, specific, and attainable goals in place, the management team can more easily share the practice goals with all staff members. This clarifies how all assignments and expectations connect to the overall practice goals. These goals should be objective. Instead of setting a goal of more cataract surgeries, set one to increase from 1,020 cataract cases in 2018 to 1,100+ cases in 2019.
TOOL NO. 2: BENCHMARKING
Just as ophthalmologists are accustomed to comparing a patient’s IOP to normal pressure standards and comparing a patient’s visual acuity to the standard of 20/20, practice managers should similarly compare benchmark data to national standards and their own internal measures.
There are approximately 50 commonly measured practice benchmarks used in ophthalmology to compare normative values to one’s own practice statistics. Examples include profit margin, staff labor productivity, facility utilization, and surgical density. A complete benchmarking list can be found in John Pinto’s Little Green Book of Ophthalmology, 5th edition, published by the ASOA/ASCRS.1
The administrator is accountable to the board of directors to ensure that the practice is hitting these normative benchmarks, or, if it is not, that a corrective action plan is in place.
TOOL NO. 3: ACTION GRIDs
An action grid, another accountability document, is comparable to a medical record in which history, diagnosis, and progress are documented—but it applies to the business side of the practice. This document contains four columns (Figure). The first column lists the specific task or project, the second column identifies who is responsible for completing the task, the third column posts an agreed deadline, and the fourth column shows progress notes and status updates.
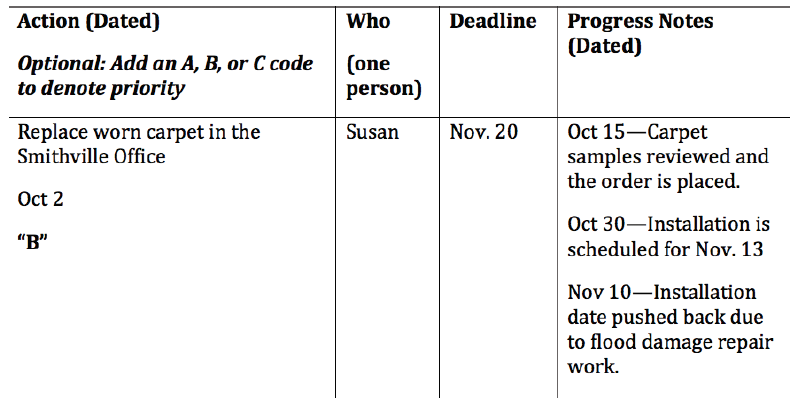
Figure. An action grid contains four columns. The first column lists a task, the second identifies who is responsible, the third lists a deadline, and the fourth shows progress notes.
The progress note section of this document keeps managers and doctors informed about the status of the company’s chief projects. The management team can save a lot of time by reading update notes prior to a meeting rather than listening while each person speaks about every project he or she is working on.
Whereas benchmarking is a quantitative measurement tool, an action grid offers more of a qualitative snapshot of assignments in progress. Another positive feature is that it captures all the great ideas that are generated but are lower on the priority list. Great project ideas will not fall between the cracks and be forgotten because they are stored on this document with a distant due date.
TOOL NO. 4: CHECKLISTS
Checklists are another great written aid to help managers monitor task completion in their departments. Establishing a checklist of the necessary tasks to be completed on a daily or weekly basis keeps the staff organized and goal-oriented. The manager can require that completed checklists be initialed and submitted at the end of the week. Rather than each manager having to verbally check in with multiple staff members, he or she can save time by reviewing the checklists. This tool helps managers and administrators be proactive rather than reactive to assess task completion.
TOOL NO. 5: ACCOUNTABLE COMMUNICATION
Accountable communication includes:
- No triangulation. Talk to each other one-to-one; don’t talk to one person about another.
- No withholding. If it is on your mind, discuss it with the appropriate party.
- No defensiveness. When a patient, doctor, or staff member tells you something you don’t like hearing, especially about yourself, don’t fight back. Instead, say: “You may be right. Tell me more.”
This trio of guidelines must be encouraged, especially with less experienced managers who may be shy about confronting issues directly. Delaying actions or discussions rarely improves a problem situation. We most often hear our clients admit: “I wish I had done that sooner.”
TOOL NO. 6: PERFORMANCE APPRAISALS
Performance appraisals can help guide employees and managers by clearly stating how individual goals tie to the overall goals of the practice. Staff members have the opportunity to grow professionally and become more productive when made aware of their strengths and weaknesses on at least an annual basis. If they are not meeting expectations, management has the opportunity to develop a formal plan for improvement.
Your expectations for every person that you review are more likely to come to fruition when described in measurable ways. Instead of saying: “We want you to become a better biller,” the manager should say: “You are posting 100 charges per day. By April, we would like you to be able to post 150 charges per day.” This sets an objective standard on which future performance reviews can be based.
This applies to MD and OD reviews, too. An instruction such as: “You need to be friendlier to patients,” is not measurable in a way that helps the doctor improve. A better approach is to conduct a patient satisfaction survey and then provide specific ideas and measures for improvement.
THE IMPORTANCE OF ACCOUNTABILITY
The chief benefit of greater accountability for providers and support staff alike is that it fosters a practice with better patient care, more teamwork, and, ultimately, more trust. There are many accountability tools available, as well as ways to use written documentation, that clarify expectations and measure results.
Managing a practice that believes in holding all individuals accountable for their work not only increases work productivity, but, more important, helps align individual and departmental goals with your overall practice goals.
1. Pinto J. John Pinto’s Little Green Book of Ophthalmology, 5th ed. Fairfax, VA: American Society of Ophthalmic Administrators; 2018.




