

After 30 years of experience with the excimer laser in ophthalmology, in 2018 LASIK has developed into a surgical procedure with incredibly good results and equally good patient satisfaction. (For more on the history of LASIK, see the accompanying excerpt below.) With recent reports of Snellen visual acuity results such as 22% of patients achieving 20/10, 81% achieving 20/12.5, and 95% reaching 20/16 visual acuity,1 the bar has been set to a very high level.
Development of LASIK
Refractive surgery’s historical timeline is marked by several milestones.
By Ioannis G. Pallikaris, MD
More than 50 years ago, José I. Barraquer, MD, of Spain, made initial strides in lamellar refractive surgery and proposed the theory that adding or removing corneal tissue can modify the refractive power of the eye.1 From the start, Dr. Barraquer realized the importance of preserving each layer of the cornea—a milestone in the development of modern lamellar refractive procedures.
KERATOMILEUSIS IN SITU
Dr. Barraquer’s original technique included the creation of a corneal lamellar disc followed by the removal of stroma, either from the bed (keratomileusis in situ) or the stromal surface of the corneal lamellar disc. In the late 1980s, lamellar refractive surgery evolved in two directions: freezing and nonfreezing procedures. According to reports, freezing lamellar procedures were often associated with corneal haze and induced irregular astigmatism.2-6
In contrast, nonfreezing techniques offered major advantages, including rapid patient recovery and fewer complications,2,3,5 but these procedures were technically difficult to perform. They involved the use of a manual keratome to perform a second cut on the stromal side of the resected lamellar disc.2,3,5
Luis A. Ruiz, MD, of Bogota, Colombia, developed a nonfreeze procedure based on keratomileusis, known as automated lamellar keratoplasty (ALK). This procedure involved a primary keratectomy with an automated microkeratome to create a corneal disc (Figure), followed by a second keratectomy on the corneal bed that removed a small central piece of cornea to create a flatter central cornea when the corneal disc was replaced. The major complication associated with ALK, however, was induced corneal irregular astigmatism.
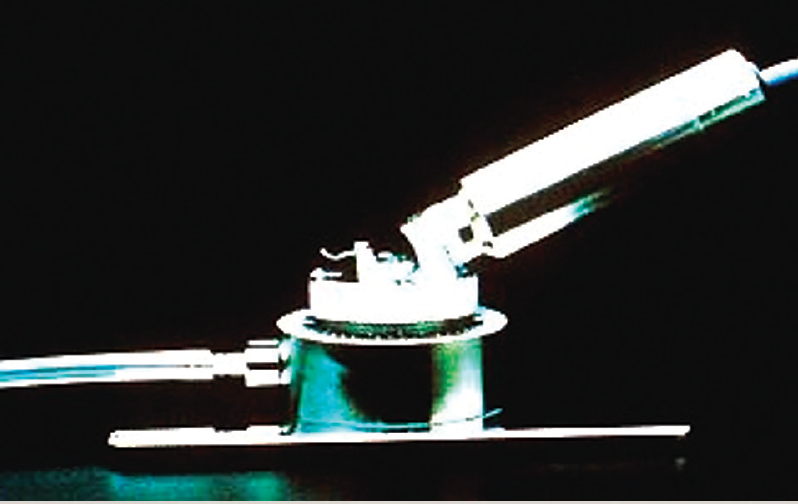
Figure. Early microkeratomes, like the Barraquer-Krumeich-Swinger, utilized a nonfreeze keratomileusis technique.
LASIK
The growing need for a safe and predictable corneal refractive procedure led our group (the Pallikaris group) to design and develop laser in situ keratomileusis (LASIK) in 1988 at the University of Crete, Greece. We combined lamellar refractive corneal surgery with excimer laser photoablation of the cornea under a hinged corneal flap.7 The first animal studies, which were intended to determine the wound-healing response after LASIK, began in 1987 and involved a Lambda Physik excimer laser and a microkeratome designed to produce a 150-mm corneal flap.8 The original idea of manually creating a corneal cap and removing central tissue from the bed was first described by Nikolai P. Pureskin, of Moscow, Russia, in 1967.9
We believed that a mechanically cut flap would ensure better tissue alignment after the intrastromal photoablation. Furthermore, we expected that this type of flap would barely affect the anatomical relations of the corneal layers because it would preserve the Bowman layer and preserve greater integrity of the superficial nerve plexus of the cornea through the base of the flap. In June 1989, the first LASIK on a blind human eye was performed at the University of Crete, as part of an unofficial blind eye protocol. Human studies began in 1990.10,11 Three months after creating the flap, we observed that the cornea remained transparent and noted no significant irregular astigmatism on corneal topography. The safety of sutureless LASIK was also suggested by Dr. Ruiz and perhaps others at that time.10
Buratto et al12 introduced an excimer laser for intrastromal keratomileusis of the corneal button in 1992, and suggested the term laser intrastromal keratomileusis. The next year, Stephen G. Slade, MD, of Houston, Texas, used the automated microkeratome to create a flap. He called the procedure excimer ALK (E-ALK) or flap and zap.13 In 1994, our team reported the early experience of LASIK on sighted eyes as well as the first study comparing LASIK and PRK.14,15 LASIK proved superior to PRK in terms of stability and predictability for the correction of myopia greater than 10.00 D. In 1999, the SVS Apex Plus Excimer Laser (Summit Technology) was FDA-approved for LASIK.16
THE FUTURE OF LASIK
We believe LASIK will remain the most popular corneal refractive procedure. We can expect ongoing evolution in the field of microkeratomes, excimer lasers, and wavefront technology. These technologies should ensure high levels of patient satisfaction after LASIK.
1. Barraquer JI. Queratoplastia refractiva. Estudios Inform. 1949;10:221.
2. Swinger CA, Barker BA. Prospective evaluation of myopic keratomileusis. Ophthalmology. 1984;91:785-792.
3. Nordan LT, Fallor MK. Myopic keratomileusis: 74 consecutive non-amblyopic cases with one year follow-up. J Refract Surg. 1986;2:124-128.
4. Maquire LJ, Klyce SD, Sawelson H, et al. Visual distortion after myopic keratomileusis: computer analysis of keratoscope photographs. Ophthalmic Surg. 1987;18:352-356.
5. Nordan LT. Keratomileusis. Int Ophthalmol Clin. 1991;31:7-12.
6. Barraquer C, Guitierrez A, Espinoza A. Myopic keratomileusis: short term results. Refract Corneal Surg. 1989;5:307-313.
7. Pallikaris I, Papatzanaki M, Stathi EZ, et al. Laser in situ keratomileusis. Lasers Surg Med. 1990;10:463-468.
8. Pallikaris I, Papatzanaki M, Georgiadis A, Frenschock O. A comparative study of neural regeneration following corneal wounds induced by argon fluoride excimer laser and mechanical methods. Lasers Light Ophthalmol. 1990;3:89-95.
9. Pureskin N. Weakening ocular refraction by means of partial stromectomy of the cornea under experimental conditions. Vestn Oftalmol. 1967;8:1-7.
10. Pallikaris IG, Papatzanaki ME, Siganos DS, Tsilimbaris MK. A corneal flap technique for laser in situ keratomileusis. Arch Ophthalmol. 1991;109:1699-1702.
11. Siganos DS, Pallikaris IG. Laser in situ keratomileusis in partially sighted eyes. Invest Ophthalmol Vis Sci. 1993;34:800.
12. Buratto L, Ferrari M, Rama P. Excimer laser intrastromal keratomileusis. Am J Ophthalmol. 1992;113:291-295.
13. Slade SG. Lamellar refractive surgery. Semin Ophthalmol. 1994;9(2):117-124.
14. Pallikaris IG, Siganos DS. Excimer laser in situ keratormleusis and photorefractive keratectomy for the correction of high myopia. J Refract Corneal Surg. 1994;10:498-510.
15. Pallikaris IG, Siganos DS. Corneal flap technique for excimer laser in situ keratomileusis to correct moderate and high myopia: two-year follow-up. Paper presented at: the ASCRS Symposium on Cataract, IOL and Refractive Surgery, 1994. pp. 9-17.
16. FDA Talk Paper. FDA’s report on new health care products approved in 1999. Available at: http:// www.fda.gov/bbs/topics/ANSWERS/ANS00998.html. Accessed March 9, 2004.
Equally impressive is a patient satisfaction rate of 95.4%, gleaned from a meta-analysis of the global LASIK literature.2 These kinds of results were independently confirmed in the Patient-Reported Outcomes With LASIK (PROWL) studies. In the FDA-sponsored questionnaire PROWL 1 and PROWL 2 studies, a patient satisfaction rate of greater than 96% was reported.3 If there is another surgical procedure with a higher satisfaction rate, I am unaware of it.
These achievements have been made possible by continual improvements in LASIK techniques and technologies, including the introduction of the femtosecond laser for flap creation (Figure and video below) and the development of aberrometry-driven excimer laser procedures.4
INCREMENTAL ADVANCES
Current trends in LASIK surgery are focused on incremental advances to improve outcomes by reducing complications, increasing the reach of LASIK to niche populations, and increasing candidacy for LASIK.
One significant advance has been the advent of topography-guided LASIK, based on the theory that laser beam−shaping algorithms, enhanced with information obtained specifically from the cornea, have the potential to improve outcomes. Currently, the most common use of these platforms is in treating abnormal corneas, such as in patients with central islands, decentrations, quality-of-vision issues, keratoconus, and/or irregular astigmatism. As the technology evolves, we may see these types of procedures being used more regularly.
Instruments for advanced aberrometry are also available in 2018. These devices are now capable of performing pupillometry, keratometry, and topography measurements that are coaxial with wavefront measurement. Additionally, they can compensate for eye tilt, and they incorporate all of this new information to enhance the delivery of excimer laser pulses. This technology is primarily aimed at two goals:
No. 1: Overcoming the cosine effect, which diminishes the accuracy of excimer ablations and induces higher-order aberrations; and
No. 2: Improving iris registration rates, which has been shown to decrease enhancement rates and increase the precision of LASIK results.5
Intimately linked with topography-guided LASIK is the concept of using CXL in conjunction with the refractive procedure. The demonstrated strengthening of the cornea provided by CXL may help to prevent the dreaded complication of ectasia. Several studies, some concluded and some ongoing, are exploring the feasibility of this concept.6
Patients with thin corneas and high refractive corrections seem to be the most obvious cohort that might obtain benefit from this theoretical improvement with CXL. It remains to be determined how best to apply the CXL procedure and how to avoid any decrement in today’s outstanding refractive outcomes.
NOT FOR EVERYBODY
Despite all these advances, there is still a patient population for whom LASIK is not a good option. This group includes patients with high refractive errors and thin corneas, occupational risks, or questionable topographies, as well as presbyopic hyperopes.
Other options for these patients include PRK and lens-based procedures such as phakic IOL implants and refractive lens exchange.
CONCLUSION
No article on LASIK in 2018 would be complete without mentioning the new kid on the block: small-incision lenticule extraction (SMILE). (The evolution of the SMILE procedure is discussed by John F. Doane, MD, later in this issue.) In the short-term future, however, LASIK will continue to be the dominant procedure for the correction of refractive errors at the corneal plane due to its excellent results and high patient satisfaction rates. When SMILE or a similar small-incision intrastromal procedure can be driven by aberrometry, that will require a whole new discussion!
1. Tanzer DJ, Brunstetter T, Zeber R, et al. Laser in situ keratomileusis in United States Naval aviators. J Cataract Refract Surg. 2013;39(7):1047-1058.
2. Solomon KD, Fernández de Castro LE, Sandoval HP, et al; Joint LASIK Study Task Force. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116(4):691-701.
3. Eydelman M, Hilmantel G, Tarver ME, et al. Symptoms and satisfaction of patients in the Patient-Reported Outcomes With Laser In Situ Keratomileusis (PROWL) studies. JAMA Ophthalmol. 2017;135(1):13-22.
4. Schallhorn SC. Refractive surgery in the naval aviator: the Binkhorst Medal Lecture. Paper presented at: ASCRS Annual Meeting; April 28, 2007; San Diego.
5. Blanton CL. Outcomes of wavefront-guided LASIK surgery for myopia with and without iris registration. Paper presented at: ASCRS Annual Meeting; April 9-14, 2013; San Francisco.
6. Hersh PS. Corneal collagen crosslinking and LASIK. Cataract & Refractive Surgery Today. July 2015.




