Medical education permeates our daily lives. Opportunities ranging from large conferences to small meetings, peer-reviewed to trade publications, and countless digital forums have expanded since March 2020 when the COVID-19 lockdowns began. The options for medical education can feel overwhelming and often are presented as standalone tactics instead of a cohesive strategy to accomplish a measurable goal.
Medical education is designed to enhance the knowledge and influence the opinions and practice patterns of clinicians to improve patient care. In order to achieve this goal, it is critical to understand current education needs, devise precise educational goals, and identify outcome measures from objective data.
A five-step strategic process can be used to develop a structured plan to achieve medical education goals.
No. 1: Survey doctors. Get a baseline by evaluating surgeons’ factual knowledge of, clinical opinions on, and practice patterns for current and relevant topics.
No. 2: Assess education gaps. Use the survey data to create clear goals for change from the baseline.
No. 3: Develop a customized educational strategy. Address education gaps with an expert, diverse faculty.
No. 4: Execute compelling educational activities. Appeal to a broad audience by offering a mix of live, print, and digital programs.
No. 5: Measure outcomes. Assess the short- and long-term impact of the educational activities on learners.
STATISTICAL SIGNIFICANCE FOR
EDUCATIONAL OUTCOMES
What drives clinicians to improve their understanding and change their opinions and behaviors? The latest surveys from The Fundingsland Group (TFG) showed that published clinical data, the opinions of leading experts and peers, wet and dry lab demonstrations, and clinical observation have the greatest influence on surgeons’ decision-making about a new technology.
The five-step strategic process outlined earlier can be used to identify the long-term and statistically significant impact of an educational initiative on learners. Statistically significant data usually are not considered for something as difficult to measure as the impact of medical education, but it is possible to conduct a P value–level statistical analysis of the impact of education on doctors’ opinions and behavior. This involves assessing learners before and both immediately and 8 weeks after an educational intervention (Figure 1).
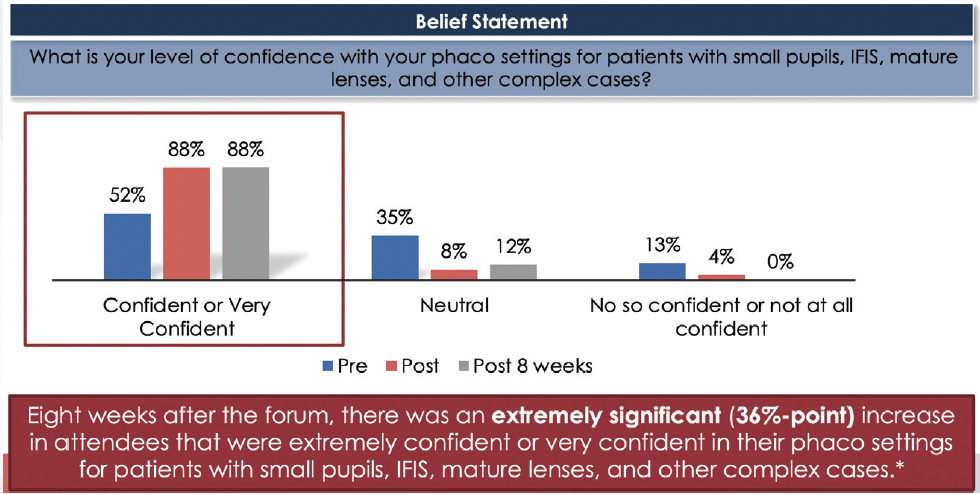
Figure 1. A statistically significant impact (P < .0001) on phaco setting confidence was achieved 8 weeks after an educational symposium. Abbreviation: IFIS, intraoperative floppy iris syndrome
EDUCATION IMPROVES PATIENT ACCESS
TFG reviewed its database of more than 25,000 global doctor surveys to evaluate participants’ clinical opinions on and practice patterns for toric IOLs. Key questions asked regarded rotational error tolerance, axial alignment techniques, diagnostics for axis identification, and preferences for surgically induced astigmatism calculations (Table).
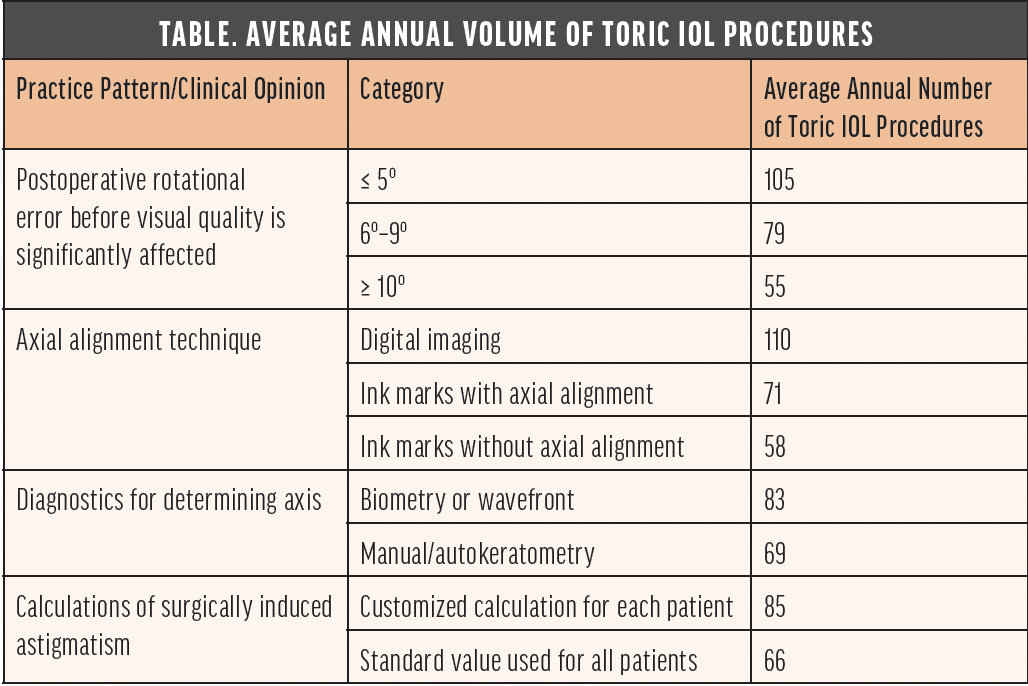
The average annual volume of toric IOL procedures was analyzed for the subgroup of respondents who answered all four questions. Those who demonstrated more advanced opinions or practice patterns had a significantly higher annual toric IOL volume. One possible explanation is that doctors who achieved better outcomes had greater confidence in their methods and therefore offered toric IOLs to more patients. Another possibility is that improved outcomes led to more patient referrals (Figure 2).
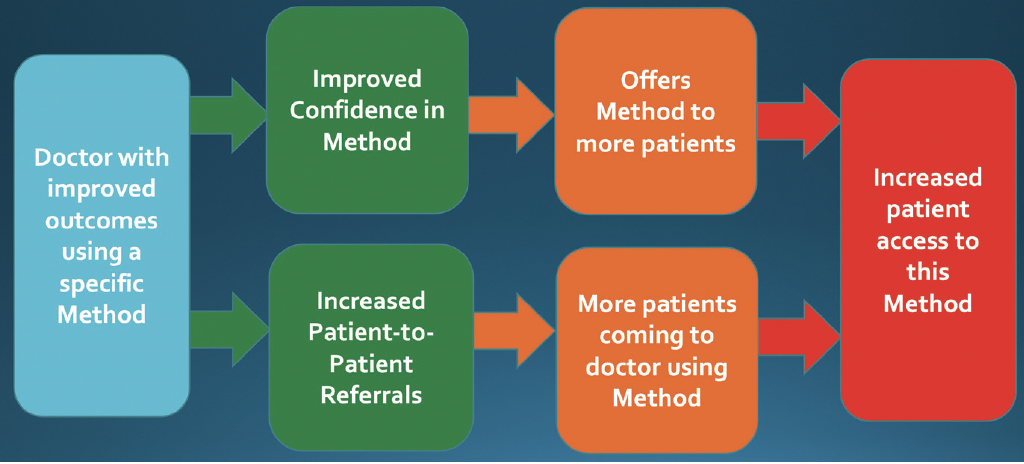
Figure 2. Theoretical diagram of how a doctor with improved outcomes can expand patient access to technology.
EVOLVING ROLES FOR FACULTY
Faculty for educational programs are typically assigned a topic and asked to produce content by a certain date without much context or support. This can lead to presentations being developed without a strong understanding of the program’s educational goals and sometimes with content that overlaps with other presentations.
The use of data-driven medical education can improve the faculty dynamic. Faculty become involved in the five-step strategic process, and they understand why a gap in education exists, how their role in the educational program can address the gap, and how outcomes will be measured to assess the impact of the education that they provide. A trained educational professional can assist the faculty by providing resources such as recent publications and research as well as the perspectives of other colleagues on a similar topic. The result is an evolved interactive relationship supporting the faculty to help create a dynamic education program.
Increased diversity is crucial to the future of medical education. The inclusion of a faculty that is representative of different sexes and genders, demographic backgrounds, practice settings, and ages, for example, provides the broadest viewpoint and greatest level of relevance to learners. The development of a diversity statement is central to this process (see Sample Diversity Statement).
Continued measurement of progress in diversity is important to move forward. For example, the percentage of female faculty in TFG’s US programs has grown from 23% in 2018 to 38% in 2021.
Sample Diversity Statement
At The Fundingsland Group, we believe our commitment to diversity, equity, and inclusion is essential to providing exceptional professional education. We believe that leveraging a variety of perspectives fosters creativity and innovation, advances the medical specialties we serve, and ultimately improves patient care.
Diversity. We commit to embracing diversity in myriad forms, including race, ethnicity, sex, sexual orientation, age, country of origin, and practice location and setting, among other areas. We consciously pursue diversity in our hiring, contracting, and selection of faculty.
Equity. We pledge to create a more level playing field for historically underrepresented voices in the specialties we serve and to challenge and respond to bias, harassment, and discrimination when they arise.
Inclusion. We commit to fostering a culture of belonging. We increase the reach of our educational activities when they are welcoming to and respectful of all, and we actively support and foster the capabilities and experiences of a wide variety of educators.
We believe that striving to affirm and expand our commitments to diversity, equity, and inclusion allows us to provide best-in-class professional education that has a positive impact on learners and effectively changes practice patterns.
SUPPORTING DATA-DRIVEN EDUCATIONAL STRATEGIES
One way industry can support medical education is to organize programs that are coordinated and developed by a single company. These programs can promote understanding of features and functionality of technologies, but the educational content is highly regulated by the manufacturer.
Another effective approach is for companies to support independent data-driven educational strategies that develop effective, compelling, and compliant medical education programs. The outcome goals of these strategies are designed to close the educational gaps identified in the large doctor surveys. Most data-driven educational strategies are supported by multiple company grants to foster meaningful changes in the knowledge, opinion, and practice patterns of clinicians and enhance patient care.
CONCLUSION
It is time to consider new perspectives on medical education. The use of a focused strategy, precise goals, and data-driven outcomes takes advantage of live, print, and digital education to impact a wider group of doctors and patients than ever before. These efforts can drive measurable improvements in clinical outcomes and practice growth with the support of diverse, strategically integrated faculty and the independent support of industry.