
José Ignacio Barraquer, MD, is generally considered to be the father of refractive surgery. He coined the term refractive surgery 80 years ago when he developed keratomileusis to reshape the cornea to correct refractive error. Following in his innovative footsteps, Sir Harold Ridley, Charles D. Kelman, MD, and Svyatoslav Fyodorov, MD, pioneered lens implants, phacoemulsification, and radial keratotomy, respectively. Injectable astigmatism- and presbyopia-correcting IOLs were introduced thereafter, followed by the excimer laser in the 1980s to change corneal shape and correct myopia, hyperopia, and astigmatism with PRK and LASIK. By the end of the 20th century, the groundwork had been laid for refractive surgery as a specialty.
We are in the midst of a new renaissance in refractive surgery owing to myriad technology-driven innovations. Refractive surgery is part of the mainstream and accepted by the general public. Its benefits for patients are undeniable.
THE GREAT PANDEMIC
2020 should have been a watershed year for refractive surgery. Many of us anticipated that the demand for refractive surgery would finally rebound after its collapse with the recession of 2008. Innovations such as the development of femtosecond lasers for cataract surgery, an explosion in presbyopia-correcting IOL technology, advances in laser platforms and diagnostic technologies, a renewed interest in phakic IOLs, new laser procedures for presbyopia correction, the introduction of SMILE, and the public’s growing trust in LASIK pointed toward the specialty’s recovery. Myopia control, CXL, and presbyopia drops expanded the burgeoning field of medical refractive treatments. Many ophthalmologists began to recognize that refractive surgery was the best way to grow their practices as traditional insurance reimbursement declined. We were poised for refractive surgery to be recognized as a full-fledged specialty.
Then SARS-CoV-2 shook the world, changing the hopes we had for refractive surgery in 2020 and creating a vacuum both politically and educationally. A positive effect of the COVID-19 pandemic is that education and training have become ubiquitous and far more cost- and time-effective than ever before. Smaller, curated virtual events are providing a high-quality experience at a much lower cost than attendance at many of the largest meetings, allowing us to expand our knowledge and advance our practices by learning about disruptive innovations in refractive surgery.
A NEW COLLEGE
The primary interest of the World College of Refractive Surgery & Visual Sciences (WCRS) is to teach, promote, and expand the specialty and science of refractive surgery globally. The college aims to increase the number of trained refractive surgeons and to establish refractive surgery as a standalone medical specialty by providing oversight, evaluation, credentialing through education, training, and certification.
The WCRS works with its affiliated foundation, the Visual Freedom Foundation, to achieve maximal social impact and advocacy for refractive surgery with the joint goal of combating preventable blindness due to unaddressed refractive errors.
Established refractive surgery practices that meet baseline requirements can be grandfathered into the WCRS if they adopt facility standardization requirements. The college also provides a path for young surgeons and residents to become certified refractive surgeons and accreditation to educational programs and teaching organizations.
THE BLACK SWAN
In his influential book The Black Swan, Nassim Nicholas Taleb stated that a black swan event is rare, highly improbable, and unexpected and causes massive consequences.1 The three attributes of this sort of event are that it is outside the realm of regular expectations, it has an extreme impact, and people’s instinct is to explain the event in attempt to make it more predictable in the future.
The pandemic is a black swan event, and it raises two questions regarding its effect on the renaissance of refractive surgery:
No. 1: How and why did the pandemic change the status quo of refractive surgery?
No. 2: What lessons did we learn, and what do we have left to learn?
A small group of international refractive surgeons, of which we are members, is looking past the pandemic and meeting regularly to answer these questions. The World College of Refractive Surgery and Visual Sciences was created with the goal of establishing refractive surgery as a standalone specialty (see A New College). Much of this article describes our plans for the future of refractive surgery.
BRAND AND IDENTITY
Branding is what the public thinks you are. We identify ourselves as refractive surgeons, but our patients identify us as LASIK or cataract surgeons. Similarly, annual society meetings host refractive surgery specialty days, but refractive surgery is not recognized as a specialty by the American Board of Medical Specialties.2 We have branding and identity problems.
The rise of virtual education has allowed refractive surgeons to gain information and opinions from an international range of colleagues. That connectivity has changed the worldview of refractive surgery as a global specialty. Refractive surgeons are unifying—giving us an opportunity to establish our identity—but refractive surgery education, training, and credentialing lag decades behind other specialties in ophthalmology.
THE CURRENT STATUS OF TRAINING
There is little to no residency training for refractive surgery. According to the Accreditation Council for Graduate Medical Education, the requirement to graduate with a core competency in refractive surgery is to perform or assist in six keratorefractive procedures, which includes observing an attending perform a limbal relaxation incision.3 In 2019, the national median for graduating US residents for total keratorefractive surgical procedures performed as a primary surgeon was two. The national median for either LASIK or PRK performed by graduating US residents as the primary surgeon in ophthalmology was zero.
The lack of exposure to refractive surgery during residency leaves young ophthalmologists both uninformed and poorly trained. No formal postgraduate education and training requirements therefore exist for refractive surgery. Knowledge, curriculum, and training remain informal, fragmentary, and noncompulsory, and they are left up to individual doctors. An ophthalmologist fresh out of medical school with no residency training in refractive surgery could attend a few hours of specialty day and claim to be a refractive surgeon. This would be unthinkable for retina and other specialties.
Each ophthalmology specialty sets its own guidelines and standards for knowledge, training, and skills transfer and has unique credentialing, certification, and qualification standards. Refractive surgery is the only ophthalmic specialty that has no such board. Therefore, there are limited fellowship opportunities, and no academic institutions offer refractive surgery fellowships.
The failure to recognize refractive surgery as a specialty is not limited to the United States. The field is also not recognized as a specialty by medical boards in Europe, Asia, and other parts of the world, and it has not been treated as a specialty by ophthalmology governing bodies on a global scale.
The AAO, ASCRS, American-European Congress of Ophthalmic Surgery, and myriad small organizations offer excellent courses, lectures, webinars, and corporate-sponsored training in refractive surgery. The problem is there is no internationally standardized curriculum that has ever been recognized or even proposed. No scope of practice, training, or experience in refractive surgery has ever been defined or required by the Board of Ophthalmology, the AAO, the ASCRS, or their contemporary counterparts in other countries.
HISTORICAL BIAS AND LACK OF GROWTH
OF REFRACTIVE SURGERY
Bias. Both lens- and cornea-based refractive surgery procedures were met with significant opposition initially. General ophthalmologists questioned the ethics and propriety of cash-pay procedures for refractive vision correction on healthy eyes and considered the risks involved to be greater than the benefits to patients. Inadequate education and training biases remain prevalent in general ophthalmology.
Lack of growth. In the past 25 years, between 20 and 25 million LASIK procedures were performed.4 Since 2008, however, fewer than 800,000 LASIK procedures have been performed annually on average.5 The total market penetration is only 0.2% per annum.4 COVID-19 led to an increase in LASIK numbers, but when both population growth and the prevalence of myopia are considered, the statistical penetration of LASIK has not risen (Figure 1). Figures 2 and 3 provide more context in terms of population growth5 and growth of myopia prevalence.6
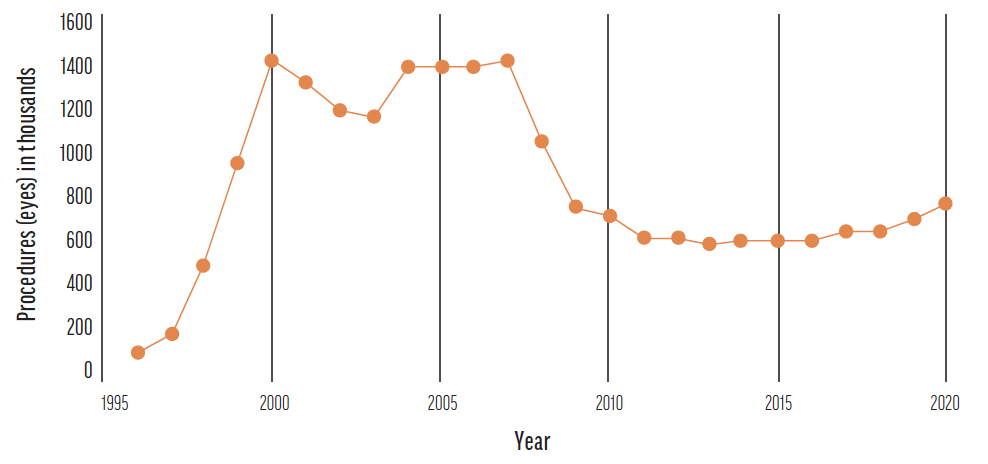
Figure 1. Estimated number of LASIK procedures performed between 1996 and 2020 in the United States. Source: Joffe SN. The 25th anniversary of laser vision correction in the United States. Clin Ophthalmol. 2021;15:1163-1172.
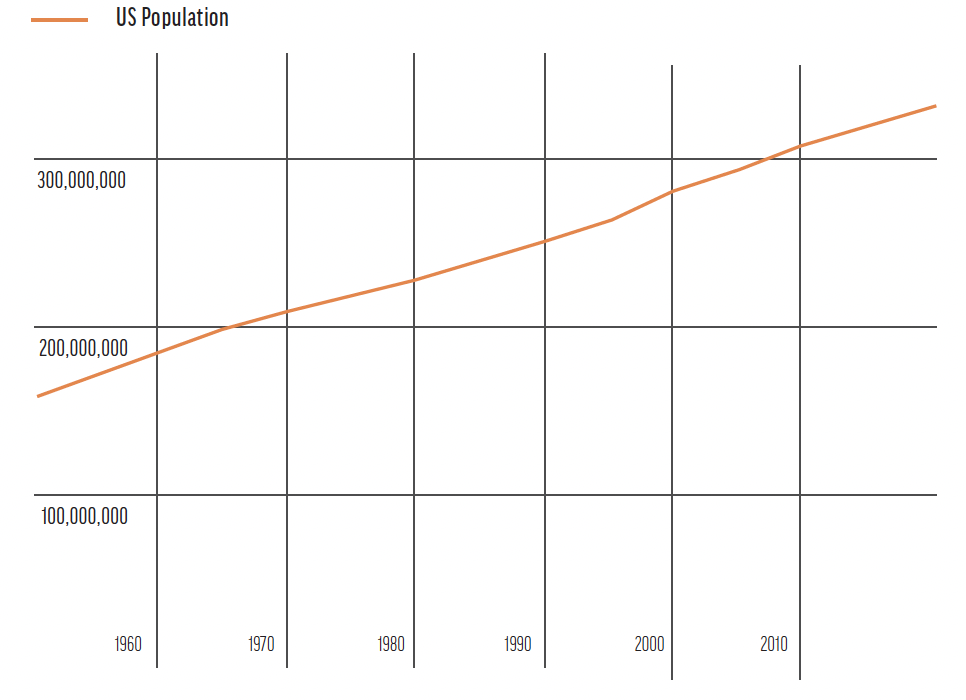
Figure 2. Growth in the US population from 1950 to 2020. Source: Stewart C. Number of LASIK surgeries in the United States 2020. Statista. July 18, 2016. Accessed May 7, 2022. https://www.statista.com/statistics/271478/number-of-lasik-surgeries-in-the-us
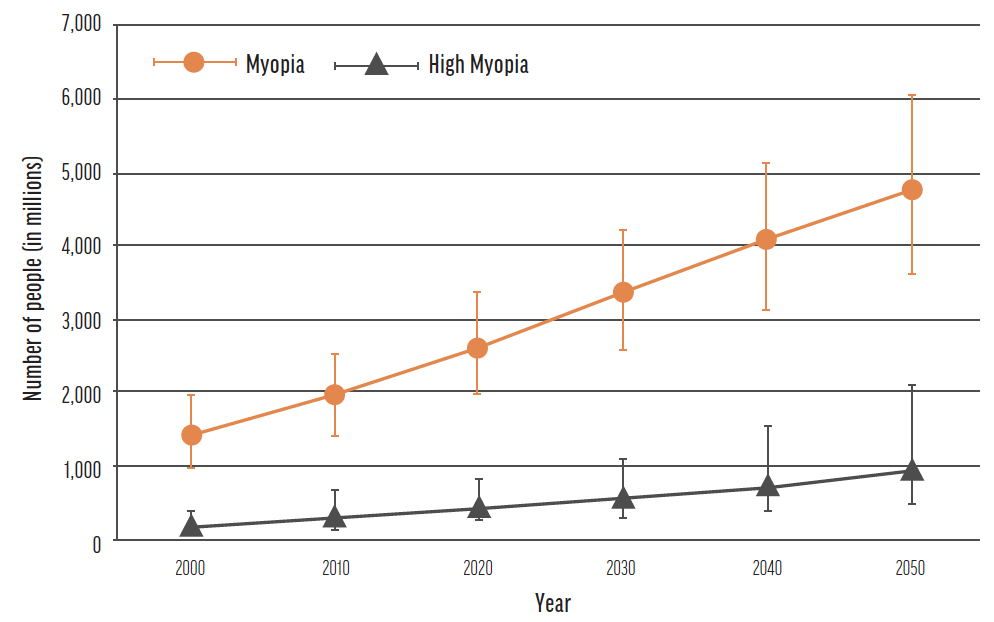
Figure 3. The current and projected growth of myopia from 2000 to 2050. Source: Holden BA, Fricke TR, Wilson DA, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042.
Individual refractive surgery practices are flourishing owing to a rapid expansion of IOL technologies and the resurgence of LASIK, but this has had little effect on the overall market penetration of refractive surgery.
Of the 1,000 fixed laser sites in the United States, 65% are owned by surgeons, 25% are corporate, and less than 10% are owned by the military or hospitals. More than 6,000 US ophthalmologists have received training on laser vision correction procedures, but only 700 of them account for approximately 80% of the procedures performed.4 The data for procedures performed in Europe mirror those in the United States (Figure 4).5
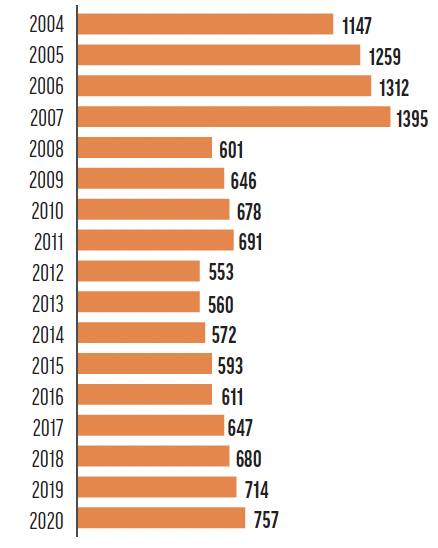
Figure 4. Number of LASIK procedures in thousands performed in Europe from 2004 to 2020. Source: Stewart C. Number of LASIK surgeries in the United States 2020. Statista. July 18, 2016. Accessed May 7, 2022. https://www.statista.com/statistics/271478/number-of-lasik-surgeries-in-the-us
The market penetration of premium IOLs was around 15% and 16% in 2017 and 2021, respectively. The United States accounted for 33.5% of all premium IOL implantation procedures performed in 2021 (data from Market Scope). There is a nearly fivefold difference between market penetration and the level of acceptance by refractive cataract surgeons (Figure 5).
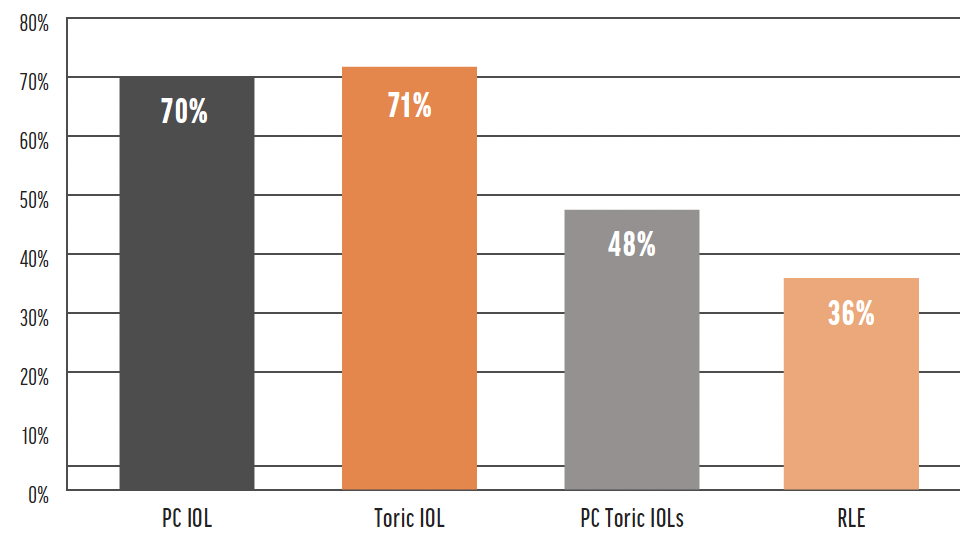
Figure 5. US surgeon adoption rate of premium IOLs. Abbreviations: PC, presbyopia-correcting; RLE, refractive lens exchange Source: Market Scope
According to longtime industry insider J. Andy Corley, most cataract surgeons currently offer premium IOLs, but 75% of them implant fewer than 40 premium IOLs a year. Technology has vastly improved but only a minority of surgeons embrace the commitment required to be dedicated refractive surgeons.7
THE LACK OF REFRACTIVE SURGEONS AND THE SOLUTION
According to Market Scope, of the 27,000 ophthalmologists practicing in the United States, fewer than 2,800 identify as refractive surgeons. An estimated 280,000 ophthalmologists worldwide are in practice, but only 10% to 12% in the developed world claim to practice some refractive surgery.8 In the developing world, the statistics are more dire: There are only 3.7 ophthalmologists per 1 million people and only one refractive surgeon per 3 million people.9 This has exposed the need to address the causes of preventable blindness worldwide.
For refractive surgery to be established as a standalone medical specialty, its objectives should be aligned with those of other ophthalmic specialties. Oversight, evaluation and credentialing through accreditation of education and training, and certification guidelines must be established. This would build public trust. The board should be independent and only supportive in its role. It should not teach courses or sponsor programs or meetings but rather be collaborative with existing professional teaching organizations, societies, academies, and residency programs to promote and expand refractive surgery. This comprehensive process must involve educational requirements and professional peer evaluation and development for refractive surgeons and other stakeholders who strive to ensure excellence in refractive surgery.
The definition of a medical specialty is “a branch of medical practice that is focused on a defined group of patients, diseases, skills or philosophy.”10 The refractive surgery specialty treats a defined group of otherwise healthy patients who elect to undergo the highly specialized medical or surgical lens- or cornea-based correction of a specific refractive error.
Vision correction should be a basic human right, and refractive surgery should be a primary tier of vision correction instead of prosthetics such as glasses and contact lenses.
The world’s population is a staggering 7.8 billion people.11 Population growth, the explosion of myopia worldwide, and an aging population are creating global imbalances between the demand for and suppliers of refractive surgery. Industry has begun to realize that the inadequate supply of trained refractive surgeons is the root cause of the imbalance. The absolute number of refractive procedures has not kept pace with the variables of population growth and age and the growing prevalence of myopia. The World College of Refractive Surgery and Visual Sciences was established to be the solution to this problem.
LEAVING A LEGACY
Some refractive surgeons and organizations may ask why they should join the effort to make refractive surgery its own specialty and how it may help their practices. The answer is that, for almost a century, courageous doctors have sacrificed everything against great odds to give you the comfortable practice you enjoy today. The need to establish refractive surgery as a specialty is important because it will honor those who have sacrificed much to get us here.
Our attempt to codify the tenants needed and the immersive learning process involved in becoming a refractive surgeon is out of respect for the trust of our patients. For privileged surgeons: This is your legacy to light the path for others to follow your journey. For others, standing for education and training and trying to balance the inequality of this world by addressing the root causes of preventable blindness are important work. No one succeeds alone. We need to create this story together.
1. Taleb, Nassim Nicholas. The Black Swan: The Impact of the Highly Improbable. Random House; 2012.
2. Medical specialties certified by ABMS member boards. American Board of Medical Specialties. Accessed May 7, 2022. https://www.abms.org/member-boards/specialty-subspecialty-certificates
3. Ophthalmology case logs: national data report. Accreditation Council for Graduate Medical Education. Accessed May 7, 2022. https://www.acgme.org/globalassets/PDFs/240_National_Report_Program_Version_2018-2019.pdf
4. Joffe SN. The 25th anniversary of laser vision correction in the United States. Clin Ophthalmol. 2021;15:1163-1172.
5. Stewart C. Number of LASIK surgeries in the United States 2020. Statista. July 18, 2016. Accessed May 7, 2022. https://www.statista.com/statistics/271478/number-of-lasik-surgeries-in-the-us
6. Lipson M, Brooks M, Koffler B. The role of orthokeratology in myopia control: a review. Eye & Contact Lens. 2018;44:224-230.
7. Dell SJ. The premium IOL channel: pitfalls and prospects. Cataract & Refractive Surgery Today. May 2018. Accessed May 7, 2022. https://crstoday.com/articles/2018-may/the-premium-iol-channel-pitfalls-prospects
8. Resnikoff S, Lansingh VC, Washburn L, et al. Estimated number of ophthalmologists worldwide (International Council of Ophthalmology update): Will we meet the needs? Br J Ophthalmol. 2020;104:588-592.
9. Vision impairment and blindness. World Health Organization. October 14, 2021. Accessed May 7, 2022. https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment
10. United States population (live). Worldometer. Accessed May 7, 2022. https://www.worldometers.info/world-population/us-population
11. Lindstrom RL. Refractive cataract surgery will continue to grow, benefiting society. Healio. December 20, 2021. Accessed May 7, 2022. https://www.healio.com/news/ophthalmology/20211216/refractive-cataract-surgery-will-continue-to-grow-benefiting-society




