CASE PRESENTATION
A 74-year-old White man presents for an evaluation of a dislocated one-piece toric IOL in the right eye. The patient underwent penetrating keratoplasty (PKP) for keratoconus in 2007, cataract surgery and toric IOL implantation in 2009, repositioning of the IOL with iris sutures in the right eye in 2009, and scleral fixation of the same IOL in 2013.
On examination, the patient’s BCVA is -3.25 +3.25 x 178º = 20/80 OD. A slit-lamp examination reveals a clear, well-positioned corneal transplant without sutures and a dislocated hydrophobic acrylic toric IOL that exhibits superior-posterior tilt. Iris sutures are present at the 11 clock position (Figures 1 and 2). The anterior capsulotomy has ragged edges.
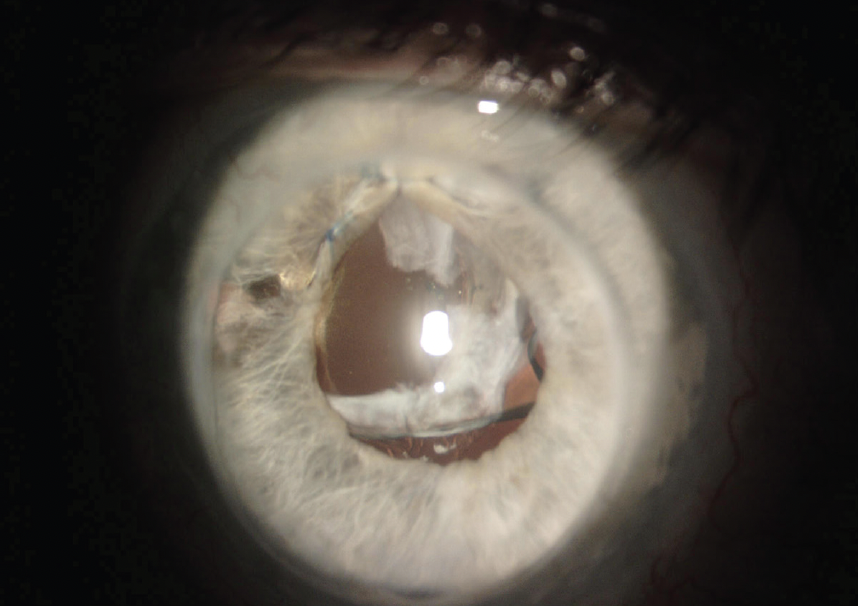
Figure 1. The toric IOL has dislocated and exhibits superior-posterior tilt.

Figure 2. Imaging of the right eye with the Pentacam (Oculus Optikgeräte).
How would you proceed? Which IOL and fixation technique would you select? Would you factor a future Descemet membrane endothelial keratoplasty (DMEK) or Descemet stripping endothelial keratoplasty into the IOL calculation?
— Case prepared by Audrey R. Talley Rostov, MD

S. ASHA BALAKRISHNAN, MD
The dislocated toric IOL would be explanted. Scleral fixation of a CT Lucia 602 (Carl Zeiss Meditec) with the Yamane technique1 would allow a large corneal incision to be avoided in the setting of a PKP.
The tilt and malposition of the dislocated toric lens is causing increased astigmatism that is noted on manifest refraction. Astigmatism correction would be based on the 1.20 D measured with corneal topography. The latter (comparatively lower) amount of astigmatism would be amenable to correction with 45º limbal relaxing incisions made in the 164º meridian. An alternative, off-label approach would be to implant a monofocal toric IOL that has holes at the optic-haptic junctions and perform scleral fixation with PTFE sutures (Gore-Tex, W.L. Gore & Associates). The lens would be aligned with the 164º axis, eliminating the need for limbal relaxing incisions. Because the CT Lucia 602 is a one-piece IOL, it should be positioned carefully 3 mm posterior to the limbus to prevent iris chafing. Whichever approach is used, the placement of iris hooks would increase visibility of the posterior space. The capsular material that remains within the pupil would be removed to improve the view further.
The edge of the anterior capsulorhexis can sometimes be used to provide additional support of a scleral-fixated IOL. In the current situation, the material would obscure the patient’s view through the new lens. The risk of graft failure merits consideration because surgery is being performed underneath the PKP. A refractive target of -0.50 to -0.75 D could compensate for a possible hyperopic shift after DMEK or ultrathin Descemet stripping endothelial keratoplasty.

CULLEN RYBURN, MD
When considering the management of a dislocated IOL, I look for a capsular tension ring. If one is present, either scleral fixation of the IOL with an 8-0 PTFE suture or four-point fixation of the IOL with a 6-0 polypropylene suture (Prolene, Ethicon) with the Canabrava double-flanged technique is performed.2 A capsular tension ring does not appear to be present here, so an IOL exchange, anterior vitrectomy, and intrascleral haptic fixation of a three-piece IOL with the Yamane technique would be performed.
Approaches to intrascleral haptic fixation continue to evolve. I currently favor a modification of the Yamane technique developed by D. Brian Kim, MD, that allows gentle docking of the IOL haptics (video demonstration below).
The accuracy of IOL calculations when intrascleral haptic fixation is performed is highly variable, especially if the cornea is irregular. When I use the Yamane technique, my refractive target is typically -1.00 to -1.25 D. I would target -2.00 D in this case, however, given that the patient will likely undergo endothelial transplantation in the future.
Currently, the most popular IOL for intrascleral haptic fixation is the CT Lucia 602 because of the forgiving nature of the polyvinylidene fluoride haptics. Any three-piece IOL, however, can work.
I counsel patients with irregular corneas like this one that they will need to wear a rigid gas permeable or scleral lens after surgery to achieve the best visual acuity possible.

WHAT I DID: AUDREY R. TALLEY ROSTOV, MD
An IOL exchange with a refractive target of -1.50 D was planned. The patient was counseled that he would need spectacles postoperatively for optimal vision. He was also advised that he might require a DMEK in the future.
A peribulbar block was administered. The conjunctiva was marked in anticipation of intrascleral haptic fixation of a CT Lucia 602 three-piece IOL. Paracentesis incisions were then created nasally and at the 6 and 12 clock positions with a diamond blade. A temporal incision was made with a diamond keratome blade, and a dispersive OVD was injected. The original IOL and capsular bag were removed with microscissors and microforceps (both from MicroSurgical Technology). The IOL–capsular bag complex was cut partially in three places and then twisted under an OVD and removed. Triamcinolone acetonide (Triesence, Alcon) was injected, and a bimanual vitrectomy was performed.
Intrascleral haptic fixation of the CT Lucia 602 IOL was performed. Postoperatively, the patient’s BCVA was -2.00 +1.75 x 170º = 20/30 OD.
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
2. Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique: no flaps, no knots, no glue. Cornea. 2020;39(4):527-528.




