
According to Cathleen M. McCabe, MD, correcting astigmatism at the time of cataract surgery is more than a mere convenience—it may be morphing into a patient expectation.
“Astigmatism now has become a fundamental part of how we take care of patients with cataract surgery,” Dr. McCabe said in a recent episode of Innovation Journal Club.
A significant number of cataract patients, as many as 1/3 if not more, have visually impactful amounts of astigmatism. Left uncorrected, even the tiniest amount of astigmatism may result in postoperative refractive surprise. In essence, why take a chance on not correcting astigmatism at the time of cataract surgery in order to deliver the best possibility for a good visual result?
“I think that we have this perception that correcting astigmatism is some mysterious thing, where you have to have all kinds of different preoperative technologies and diagnostics to do a good job in delivering for those patients,” Dr. McCabe said. She pointed out that today’s biometers excel at identifying an eye’s axis and magnitude of astigmatism, and that the technology for IOL calculations has likewise advanced to provide durable image quality.
Don’t Avoid Torics for Fear of Rotation
Astigmatism correction can take many forms, including the use of toric IOLs. Historically, torics have tended to induce anxiety among surgeons, as the lenses demand precise placement and carry a risk of rotating postoperatively. However, according to a recent study by Kramer et al, rates of repositioning surgery in the first 12 months after cataract surgery with toric IOLs are low, which suggests that the two toric models in the study exhibited good rotational stability.1
The first notable thing about the study, Dr. McCabe said, was use of the IRIS Registry Data, resulting in a study population of over 17,000 eyes. Second, although the rate of repositioning surgery in the first 12 postoperative months varied among the two toric IOL models (Figure 1), overall the rate was 1.3%, suggesting excellent rotational stability.1
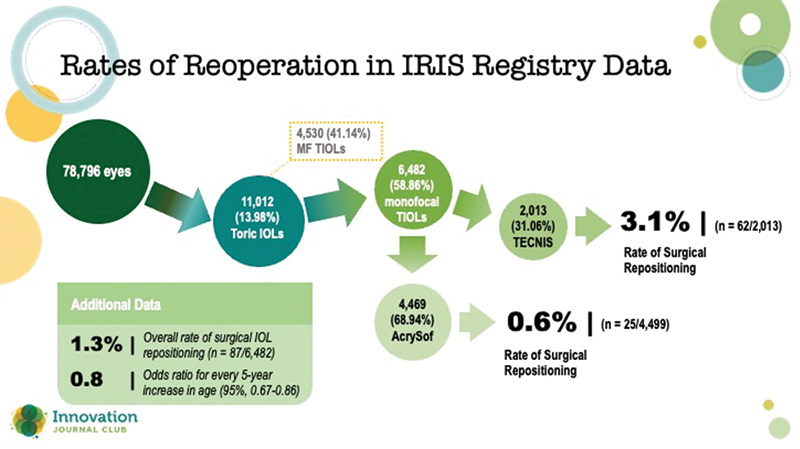
Figure 1. The rate of repositioning surgery in the first 12 postoperative months.1
In cases where she does detect postoperative IOL rotation, Dr. McCabe proceeds with a stepwise approach. She begins by determining the refraction, which she admits can be challenging in the early postoperative period because of surface dryness. “I want at least two consistent refractions that say, 'This is where the refractive astigmatism is.'” Then, she uses the Toric Check on the iTrace aberrometer (Tracey Technologies) to find the location of the lens’ axis and power.
Dr. Singh also employs the iTrace, because it can be used without dilating the eye, and it indicates whether the issue with the IOL is its position or power. Both surgeons also use the device to educate patients about how much their vision will improve by correcting it. “It’s all about the value-add,” said Dr. Singh. “We want to do our best to help educate, so the patient can make an informed decision.”
Study: FSAK Vs. Toric IOLs
Another method of astigmatism correction, femtosecond laser-assisted arcuate keratotomy (FSAK), has recently come into clinical use, although where it fits in the treatment algorithm is not formally established. One question with FSAK is how it might compare to toric IOLs in the correction of moderate amounts of astigmatism.
A recent study by Hernandez and colleagues provides some data.2 The single-center clinical research study enrolled 67 patients with age-related cataracts and preoperative corneal astigmatism of 1.25 to 3.00 D to either a toric IOL (n = 38) or FSAK (n = 37). At 3 months, patients’ mean residual refractive astigmatism was -0.63 D in the toric IOL group and -0.90 D in the FSAK group. In the toric group, 84% (32 eyes) achieved ≤ 1.00 D, versus 64% (25 eyes) in the FSAK group.
Dr. McCabe felt that the outcomes of this study confirmed what many surgeons already think: a number of factors affect the healing response with limbal relaxing incisions, and results vary.
“I think this study showed conclusively that the outcomes were better with toric lenses in those moderate amounts of astigmatism,” she said. “It's exactly what I would've expected.”
Despite her preference for torics, Dr. McCabe said still uses FSAK, such as for low amounts of astigmatism for which lens options do not exist, in combination with toric IOLs in patients with ≥4.00 D of astigmatism.
More important than modality, though, is to adopt a mindset where astigmatism correction is a first priority, and then to work within the options to find the right method for each patient. Considerations for premium lenses and other add-ons are a nice value for cataract patients, Dr. McCabe said, but surgeons should really think about starting every patient with a focus on correcting the cylinder that may impact the final visual outcome.
“You can add to it if you want, but fundamentally, let's correct your astigmatism,” she said.
