
A 69-year-old woman with a history of monovision LASIK presented for a cataract surgery evaluation with a desire for postoperative spectacle independence. Corneal topography revealed significant higher-order aberrations (HOAs). Calculated at a 4-mm pupil, the root mean square (RMS) of the HOAs in the left and right eyes was 0.137 and 0.242 µm, respectively.
Clinical experience cautioned me against selecting a diffractive multifocal IOL for the patient—my mother—and led me to choose a Light Adjustable Lens (RxSight). As I considered options, however, I contemplated if there were an accurate way to determine when a diffractive multifocal IOL could benefit patients with HOAs.
There are no real guidelines. A literature review recommended an RMS HOA cutoff of less than 0.3 µm for a multifocal IOL in an eye with a 4-mm pupil.1 Theoretically, this should produce 0.50 D of defocus. No other published study provided recommendations on multifocal IOL use in eyes with HOAs. The only other reference to a cutoff of 0.3 µm was a study presented at the ASCRS annual meeting in 2011.2
MY RESEARCH
I pulled pre- and postoperative HOA data on 378 patients with no history of refractive surgery who underwent either refractive lens exchange or cataract surgery and received a multifocal IOL at my practice. Most of them (63.8%) received a Tecnis ZKB00 (Johnson & Johnson Vision). Others received a Tecnis Symfony (Johnson & Johnson Vision), AT LARA 829 (Carl Zeiss Meditec), or Tecnis ZLB00 (Johnson & Johnson Vision).
I evaluated the eye of each patient with the greater HOA value. The mean preoperative 4-mm RMS HOA value was 0.22 ±0.11 D (median, 0.20 D; range, 0.09–1.22 D). Sixty-six patients (17%) had HOA values greater than 0.3 µm. At 3 months postoperative, patients had good binocular uncorrected near visual acuity regardless of the IOL design (Table 1). When I looked at patient-reported outcomes, I observed no difference in HOA values across the groups of patients who reported being very satisfied, somewhat satisfied, and neither satisfied nor unsatisfied (Figure 1).
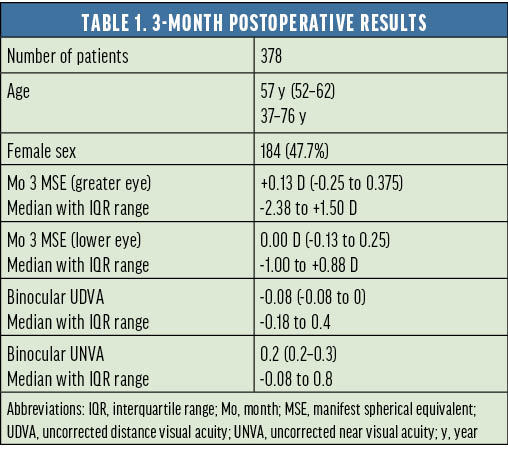
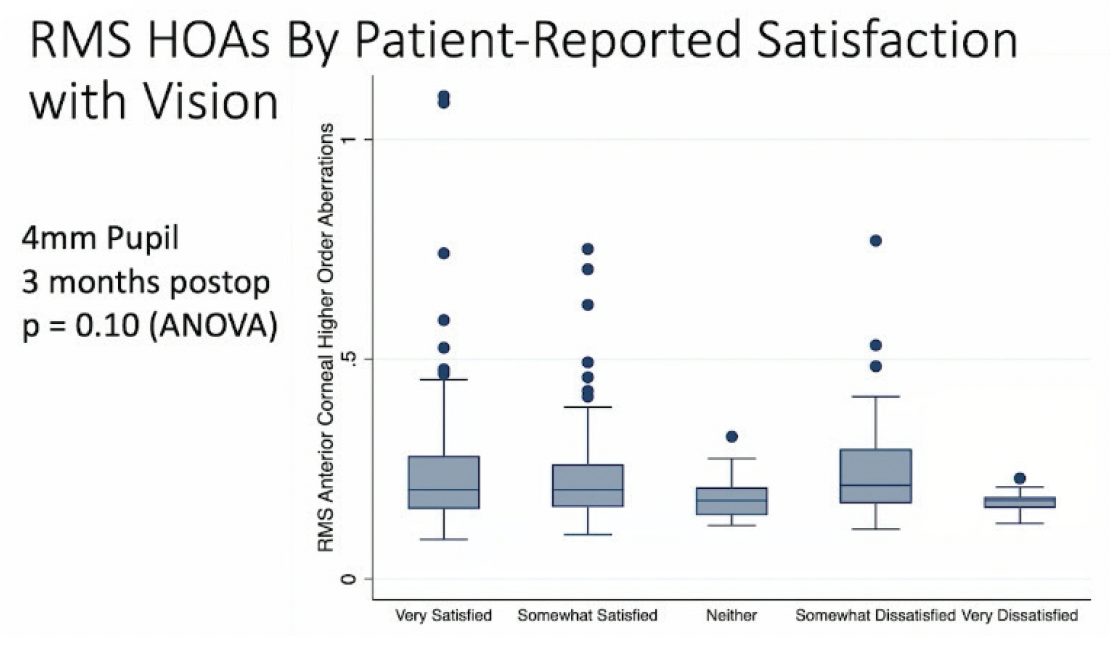
Figure 1. Patient-reported satisfaction according to RMS HOAs.
A multivariate regression model of the results is shown in Table 2. Older patients tended to be more satisfied with diffractive multifocal IOLs. Surprisingly, there was no correlation between HOAs and patient satisfaction. In fact, I observed a wide confidence interval and significant scatter in the data. Uncorrected near and distance visual acuity had the greatest effect on patient satisfaction with diffractive multifocal IOLs. The discriminatory value on a receiver operating characteristic curve unexpectedly got worse as pupillary diameter increased (Figure 2).
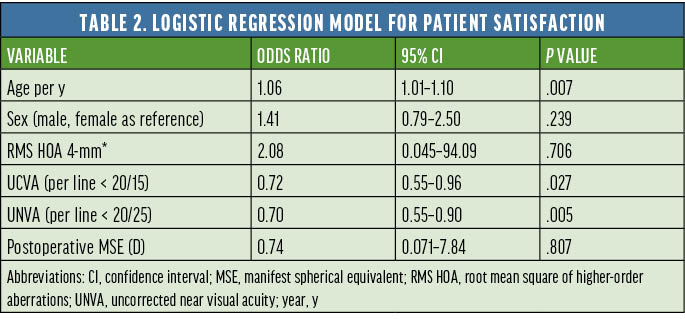

Figure 2. Discriminatory values on a receiver operating characteristic curve at different pupillary sizes.
CONCLUSION
In the population that I studied, HOAs did not influence patient-reported satisfaction with diffractive multifocal IOLs. It would be interesting to see if satisfaction is influenced by higher HOA values or a smaller pupillary aperture. As found in many other studies, however, uncorrected distance visual acuity remains the biggest factor in patient satisfaction.
1. Goto S, Maeda N. Corneal topography for intraocular lens selection in refractive cataract surgery. Ophthalmology. 2021;128(11):e142-e152.
2. Hamza I, Aly MG, Hashem KA. Multifocal IOL dissatisfaction in patients with high coma aberrations. Paper presented at: ASCRS Symposium on Cataract, IOL, and Refractive Surgery; March 25-29, 2011; San Diego.




