
The accuracy of toric IOL calculations has improved during the past 10 years largely owing to the recognition of the significance of posterior corneal astigmatism (PCA)1 and the development of formulas such as Abulafia-Koch, Barrett, Emmetropia Verifying Optical (EVO), and Kane that take PCA into account. These formulas perform well for normal eyes, but the following five situations are inherently more complex and difficult.
FIVE COMPLEX SITUATIONS
No. 1: Atypical PCA. In 2012, Koch and colleagues reported that PCA is steep vertically (with the rule) in most eyes (86.6%).1 Several modern toric formulas use this finding theoretically or through vectorial regression methods in their predictions. The assumption, however, may not apply to all eyes. Scheimpflug topographers and swept-source OCT biometers that can measure the posterior cornea may therefore be of benefit.
In a study of 602 eyes, the Barrett toric calculator performed better when PCA measurement from the IOLMaster 700 (Carl Zeiss Meditec) was used instead of predicted PCA.2 Similarly, Reitblat et al reported that the Barrett toric calculator performed better with measured versus predicted PCA in eyes with high PCA (> 0.80 D).3 I have also found higher prediction accuracy with measured versus predicted PCA in eyes that are steep horizontally (against the rule). Currently, both the Barrett and EVO toric calculators can use PCA measured by different machines.
No. 2: Low astigmatism. Eyes with low astigmatism are not considered complex but can pose a challenge. It is more difficult to measure low than high astigmatism consistently. Dry eye disease and meibomian gland dysfunction exacerbate the problem and should be treated before measurements are obtained.
In my practice, eyes are measured with two optical biometers and a Scheimpflug corneal topographer. Comparing measurements of the magnitude and axes of corneal astigmatism obtained with three machines helps establish consistency and eliminate outliers. The Barrett Integrated K calculator can be used to automate the decision-making process by calculating the vectorial median keratometry (K) readings and axes based on three different measurements. This can avoid surprises due to erroneous single measurements.
No. 3: Keratoconus. IOL power and toricity calculations can be difficult in keratoconic eyes, and corneal irregularity increases as the condition becomes more severe. Most standard IOL formulas tend to produce hyperopic refractive surprises.
Condition-specific formulas such as Barrett True-K and Kane for keratoconus have been developed. Health et al recently showed that the Barrett True-K keratoconus formula with measured posterior cornea from total K (TK) performed best for all severities of keratoconus and that the EVO formula with TK or K could be used for IOL power calculations in eyes with nonsevere disease (K ≤ 50.00 D).4
Corneal topography is key to determining whether the astigmatism is sufficiently regular to be corrected with a toric IOL. I concentrate mainly on the tangential map and its appearance within the pupillary zone because it is representative of the patient’s line of sight. My decision to implant a toric IOL or not depends largely on the regularity of the cornea within this zone.
A recent case of mine underscores the value of topography and measured PCA. Corneal topography demonstrated inferior corneal steepening (Figure 1). The tangential map indicated that the astigmatism was largely regular within the pupillary zone. K1 was 39.19 D @ 89°, and K2 was 49.36 @ 179° with astigmatism of -10.43 D @ 89°. The patient’s measured PCA was -1.56 D @ 179°, which was against the rule. A toric IOL with 12.00 D of cylinder was implanted at the 178° axis. One month after surgery, the patient’s refraction was plano -1.00 x 80°, and her uncorrected distance visual acuity was 6/7.5. The Table shows the prediction errors of toric formulas with predicted and measured PCA. The Barrett and EVO toric formulas with measured PCA performed the best, which shows the benefit of using measured PCA in eyes with high and against-the-rule PCA.
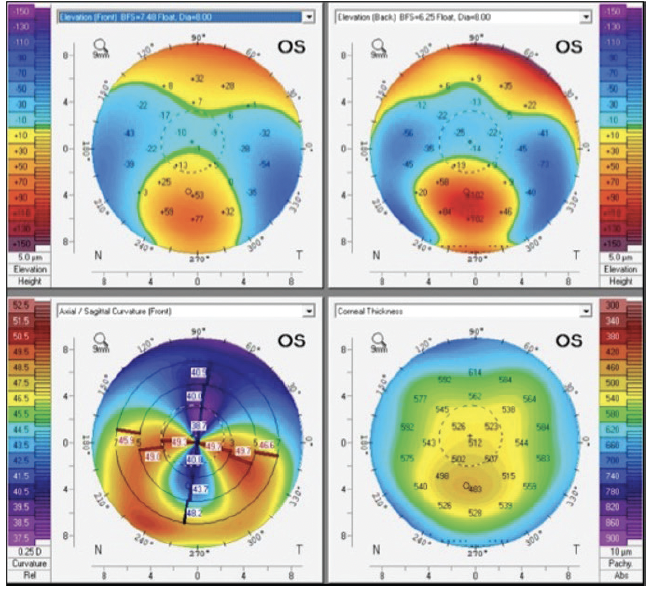
Figure 1. Corneal topography of a keratoconic eye.

No. 4: History of laser vision correction. Although most patients who have undergone laser vision correction have low astigmatism, it is still worthwhile to correct any existing astigmatism. Both the Barrett True-K and EVO toric calculators are able to predict for eyes with previous laser vision correction. It is important to perform corneal topography to determine regularity and exclude corneal pathologies such as ectasia. Coma must also be distinguished from astigmatism because the former cannot be corrected with a toric IOL. A patient of mine had horizontal coma due to a decentered laser ablation (Figure 2). Despite simulated K readings indicating -1.50 D of cylinder, the patient did well with a nontoric monofocal IOL.
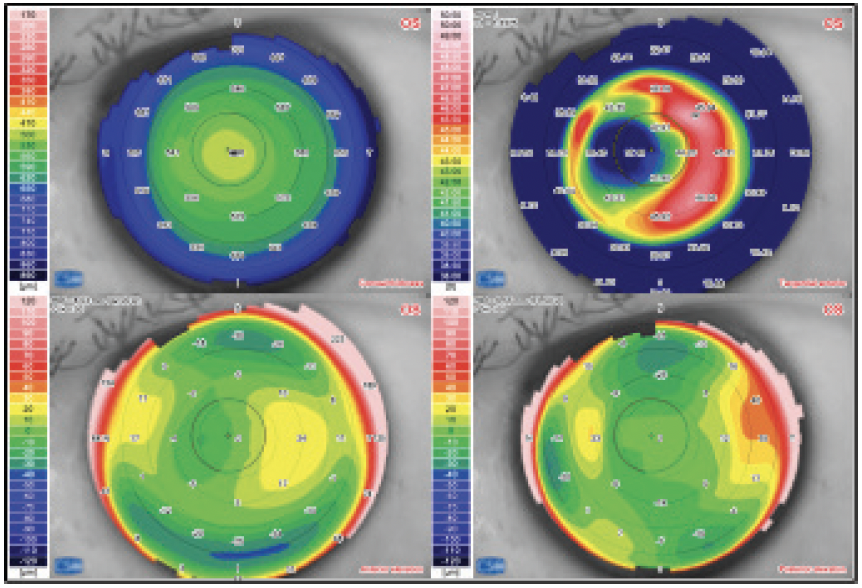
Figure 2. Corneal topography showing a decentered laser ablation.
No. 5: Highly irregular corneas. Some patients with highly aberrated corneas from scars, penetrating keratoplasty, radial keratometry, or severe keratoconus can benefit from a toric IOL. Suitability largely depends on the amount of corneal regularity determined by topography. Evidence of some degree of correctable astigmatism from previous manifest refraction can also be helpful. In severe cases, however, it may be safer to implant a neutral aspheric or pinhole IOL.
1. Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080-2087.
2. Wang L, Koch DD. Comparison of accuracy of a toric calculator with predicted vs measured posterior corneal astigmatism. J Cataract Refract Surg. 2023;49(1):29-33.
3. Reitblat O, Levy A, Megiddo Barnir E, Assia EI, Kleinmann G. Toric IOL calculation in eyes with high posterior corneal astigmatism. J Refract Surg. 2020;36(12):820-825.
4. Heath MT, Mulpuri L, Kimiagarov E, et al. IOL power calculations in keratoconus eyes comparing keratometry, total keratometry, and newer formulae. Am J Ophthalmol. Published online April 10, 2023. doi:10.1016/j.ajo.2023.03.037




