Clear corneal incisions are a routine aspect of cataract surgery but one that entails a learning curve. This article outlines some of the challenges associated with corneal incisions, including how to avoid and address an overly anterior placement.
1. PROPER KERATOTOMY PLACEMENT
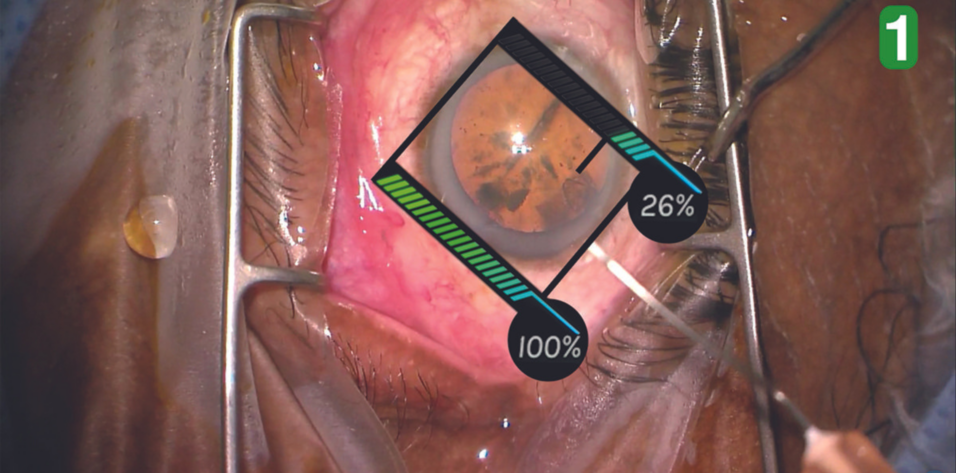
A keratotomy is typically made at the temporal or superior aspect of the cornea. If the location of the incision is too anterior, a shadow across the reduced red reflex often results, making it difficult to see what is happening during the capsulorhexis (Figure 1). Shadows do not always occur in this scenario, but they frequently do as a result of inadvertent depression of the corneal surface by the capsulorhexis forceps. The depression distorts the direction of the light reflecting off the back of the eye and decreases the amount of light arriving at the microscope, affecting the shadows (Figure 2).
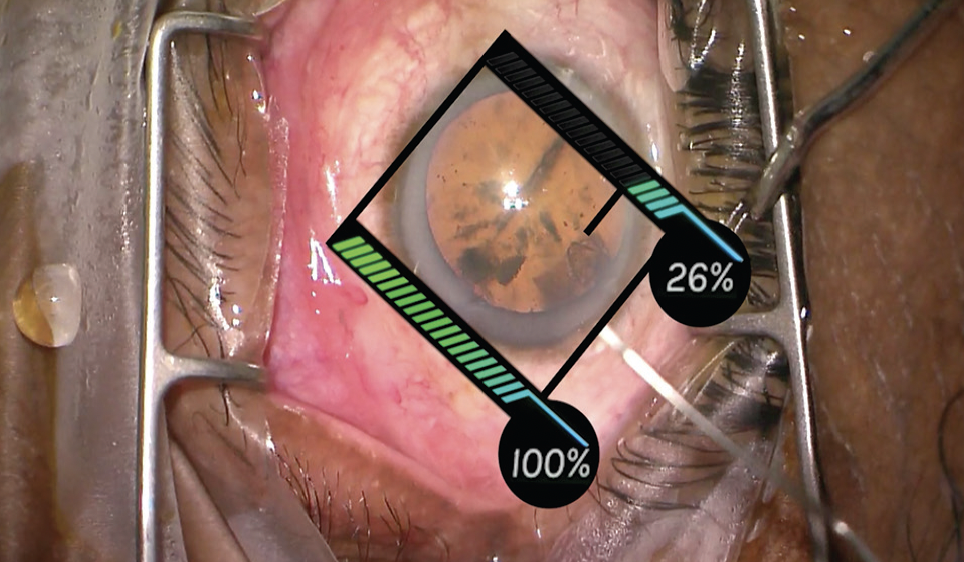
Figure 1. An overly anterior keratotomy creates shadows and reduces the red reflex.
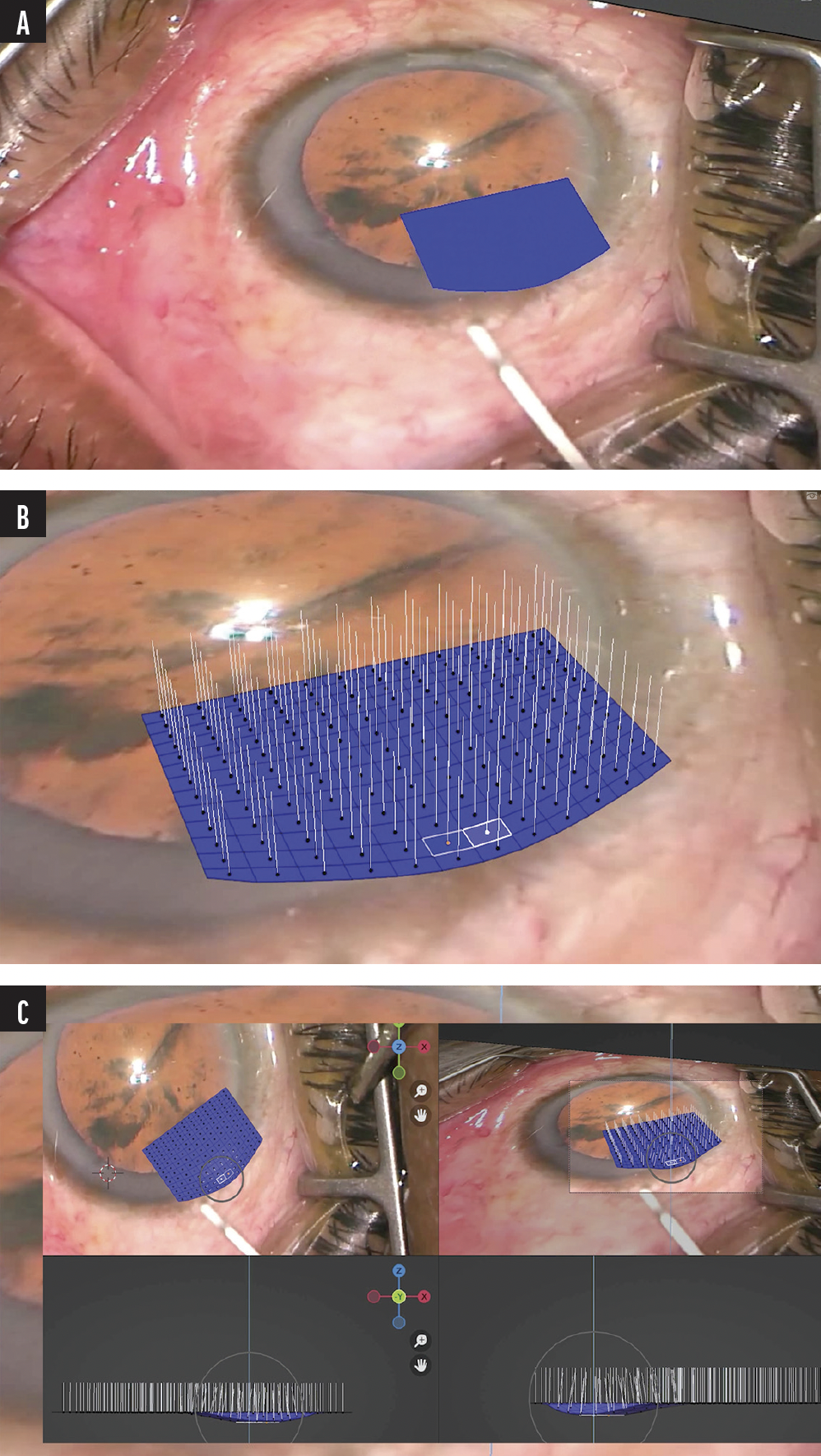
Figure 2. The blue area represents the corneal surface (A-C). Surface normals simulate the path of light from the back of the eye to the microscope (B). Pushing on the corneal surface distorts the light from the back of the eye and creates shadows (C).
Shadows are less of a problem when the keratotomy is optimally placed. In Figure 3, the keratotomy is more relegated to the peripheral cornea, and the shadow is not nearly as obstructive.
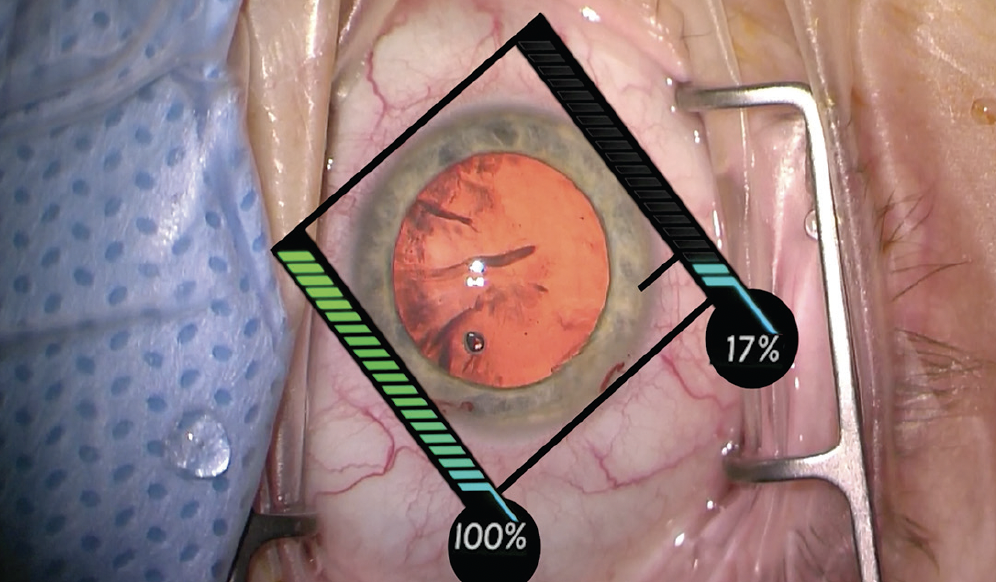
Figure 3. The keratotomy is more peripheral than pictured in Figure 2, and the shadow is not as obstructive.
2. EYE POSITION
The position of the eye may require adjustment with respect to the limbus and the rotation of the blade. The eye’s rotational position affects the length of the keratotomy. If the eye is turned away from the keratome, the wound may be overly long and thus potentially too central.
In Figure 4, the starting position of the keratotomy is too far anterior because the eye is turned too far nasally. As a result, the keratotomy’s extension across the cornea is greater and, while not extremely anterior, still causes some shadow.
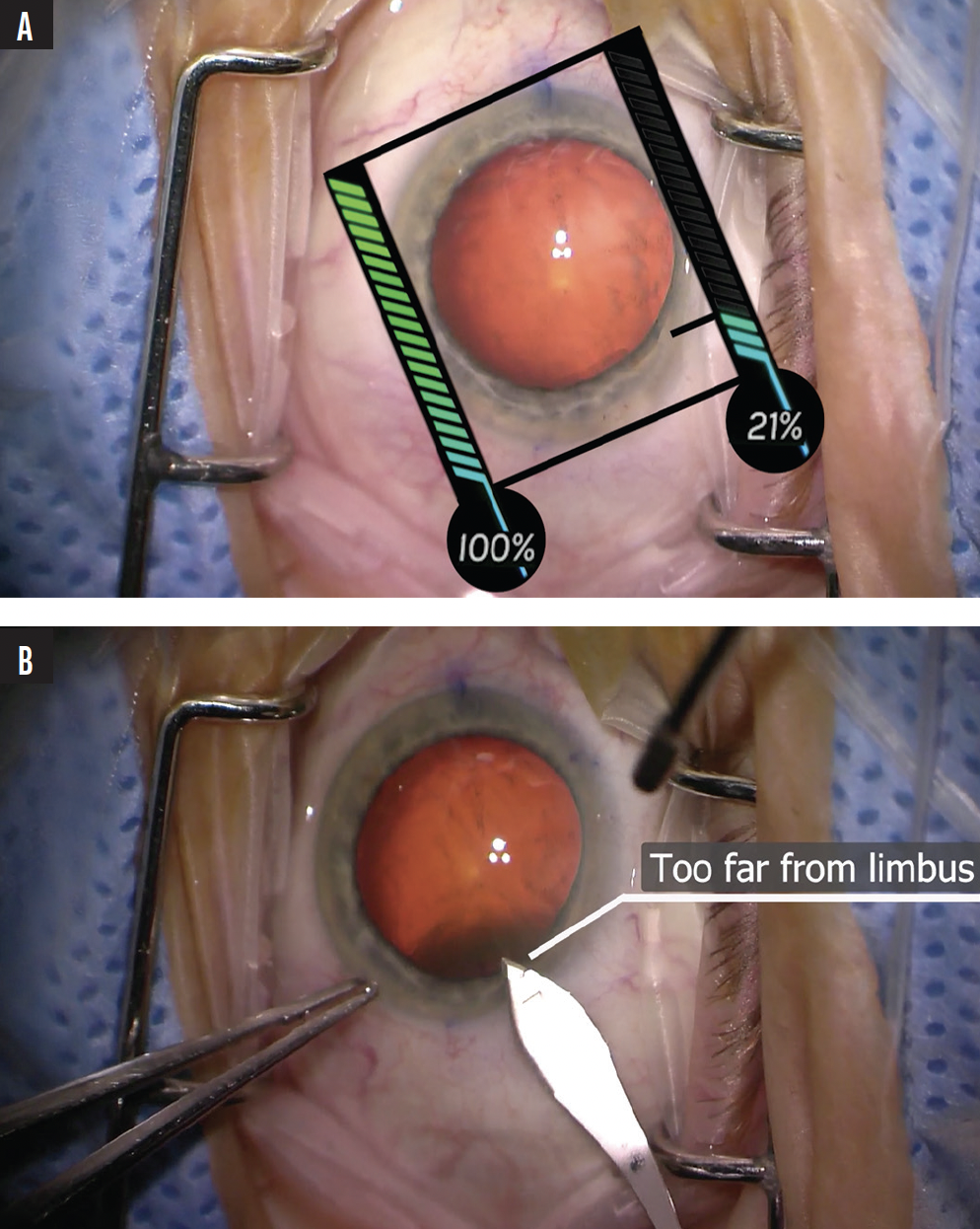
Figure 4. The clear corneal incision is started too far from the limbus while the eye is turned nasally (A), creating an overly anterior keratotomy (B).
3. BLADE POSITION
Proper orientation of the blade is required to make an effective keratotomy. If the incision starts too superficially, the blade can stutter through the epithelium and not engage the stroma early enough, which can result in an overly central keratotomy.
4. THE INCISION
In addition to avoiding a poor start, it is important to recognize when the blade takes too long to traverse the cornea and enter the anterior chamber. Ideally, the surgeon should be cognizant of a halting passage and redirect the blade into the anterior chamber or even subtly retract it and enter the anterior chamber.
5. ApproachING an OVERLY ANTERIOR KERATOTOMY
One approach to an overly anterior keratotomy is to reenter the original incision and puncture through its floor with the keratome blade, effectively shortening the passage for forceps and other surgical instrumentation. This can reduce the shadows. Of course, extra care must then be given to the incision at the end of the case to ensure appropriate closure. It may be necessary to place a suture.
CONCLUSION
Keratotomy creation may appear to be relatively straightforward in the hands of an experienced surgeon. For a young surgeon, however, the clear corneal incision can have challenging components. Successful execution requires an awareness of the eye’s rotational status, appropriate placement of the blade within the context of any ocular rotation, and an awareness of the blade’s trajectory as it traverses the cornea.