When the capsular bag is not a viable location for IOL implantation, other options must be considered. The risk of retinal tears and detachment must be minimized by eliminating intra- and postoperative vitreous traction. The risk of a suprachoroidal hemorrhage must be reduced by maintaining normotension throughout surgery. Additionally, thorough cleaning of the anterior segment must be performed to reduce inflammatory sequelae that can incite macular edema in a one-chambered eye. Lens particles that fall below the posterior capsule into the posterior segment are best left for a secondary, timely vitreoretinal intervention when necessary. Prevent collateral damage to the cornea, iris, and capsule. Never intentionally sacrifice a continuous curvilinear capsulorhexis (CCC). Rather, enlarge it if necessary, no larger than a capturable opening for the intended optic using a continuous technique. An instillation of triamcinolone acetonide for particulate identification can help with removal of prolapsed vitreous.1
When feasible, an IOL with an acrylic optic is the best choice in these eyes. An anterior chamber IOL may be an option, but it is generally undesirable due to the large incision required, sizing difficulty, and its proximity to the endothelium. Scleral fixation of an IOL requires performing a more extensive anterior vitrectomy when only simple removal of prolapsed vitreous may be required and prolongs the duration of surgery. A third alternative is to implant a three-piece IOL in the sulcus—an off-label use of an IOL in the United States.
One-piece acrylic and plate haptic IOLs are contraindicated for placement in the sulcus.2 Standard three-piece acrylic IOLs with posteriorly angulated 13-mm PMMA haptics do not fit securely in the sulcus of many eyes and can cause subclinical uveitis or uveitis-glaucoma-hyphema syndrome because of micromovements. The use of an IOL with an optic that has rounded anterior edges, such as the Tecnis series (Johnson & Johnson Vision) or enVista (Bausch + Lomb), may reduce iris chafing. It is important to note that an unsecured IOL in the sulcus may rotate and subluxate postoperatively. To achieve the targeted postoperative refraction, it is often necessary to decrease the power of an unsecured IOL in the sulcus by 0.50 to 1.00 D.3 Optic capture or another form of fixation is therefore prudent and has the advantage of not requiring a dioptric power change.
First described by Howard V. Gimble, MD, MPH, FRCSC, optic capture is defined as a configuration in which the IOL optic and haptics are positioned on opposite sides of a tear-resistant opening in the capsular membrane.4 This technique should be considered whenever placement of an IOL in the bag is deemed unsafe. Click here to view a compilation of videos demonstrating optic capture techniques.
STANDARD OPTIC CAPTURE
In the most frequently employed capture configuration, the haptics of a three-piece IOL are placed in the sulcus, and the optic is prolapsed behind an intact CCC and into the bag. If the patient has megalocornea or high myopia with an abnormally large bag, optic capture of a three-piece IOL with a large optic may be the primary procedure of choice. Anecdotally, primary anterior optic capture (with a capsular tension ring in the bag) may be more stable, blocking phimosis in cases of significant zonulopathy. More often, however, this technique is performed in the setting of a broken posterior capsule.
Optic capture requires a reasonably centered CCC that is at least 1 mm smaller than the IOL optic. The difference in dioptric power for an IOL fixated in this manner versus one implanted in the bag is trivial.
When properly configured, the captured CCC assumes the shape of a cat’s eye or football as it is anchored from one optic-haptic junction to another. This is achieved by gently depressing the optic 90º away from one optic-haptic junction so that it pops under the CCC rim. The maneuver is then repeated for the far and near edges. If the posterior capsule is intact, the OVD in the bag should be removed before capture to prevent postoperative capsular bag distension syndrome.
REVERSE AND POSTERIOR OPTIC CAPTURE
Reverse optic capture. A one- or three-piece IOL may be employed in reverse optic capture, but loop haptics instead of plate haptics are required. The lens is fully inserted into the capsular bag and then cantilevered forward so that the optic is in the sulcus while the haptics remain sequestered in the bag, away from uveal tissue. Reverse optic capture can be useful if the posterior capsule ruptures or a break in the capsule is detected after a one-piece IOL has been placed in the bag.
A similar result can be achieved with a haptic tuck technique. The IOL is placed in the sulcus, and each haptic is tucked into the bag, leaving the optic anterior to the CCC edges.5 This can be useful when the posterior capsule is already compromised; however, a one-piece IOL is desired for the refractive technology it supports.
Posterior optic capture. When the anterior CCC is too large or incomplete to permit anterior capture of the IOL optic, a posterior optic capture configuration (also referred to as a posterior optic buttonhole; Figure) may be employed. Hyaloid-sparing posterior optic capture is a safe primary choice, even in uncomplicated cases, because it offers the advantages of reducing or eliminating visual axis obscuration and maintaining a two-chambered eye for life.6 One major advantage of the technique is that it permits the implantation of a one-piece acrylic IOL, including toric and presbyopia-correcting designs, despite a complication. Although capture maneuvers that place the haptics of a one-piece acrylic IOL in the bag are possible owing to a broad optic-haptic junction, there are greater risks of lost capture and migration of endothelial cells onto an intact vitreous face compared to a three-piece IOL. The power of a posteriorly captured IOL should be reduced by 0.50 D for lower-powered lenses and 0.75 D for higher-powered lenses from calculations for placement in the bag (personal communication with Rupert M. Menapace, MD).
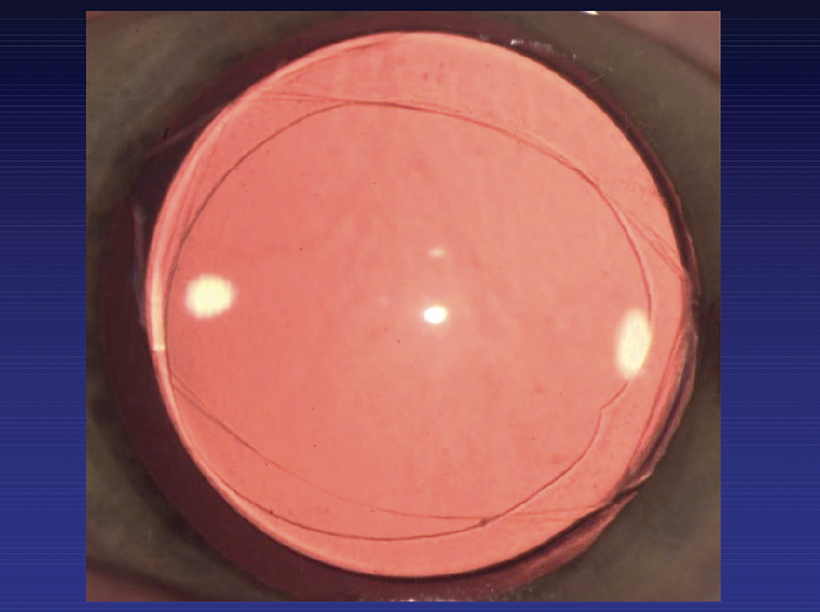
Figure. A posterior optic capture configuration.
Courtesy of Rupert M. Menapace, MD
Construction of a posterior CCC (PCCC) permits placement of the haptics in the bag while the optic is captured in the Berger space (behind the posterior capsule and in front of the hyaloid face). Even in the setting of a ruptured hyaloid face, after the removal of prolapsed vitreous, the capsular tear can be converted into a PCCC, allowing optic capture. An anterior vitrectomy performed from a bimanual limbal approach will usually enlarge the tear, even when the vitrector is directed downward through the rent. Vitreous typically comes forward and backward in this configuration. A one-port pars plana approach with irrigation through an anterior paracentesis and the vitrector through a trocar system cannula once incisions are sutured and the eye is made firm enough to tolerate the insertion pressure (or a direct microvitreoretinal blade pars plana sclerotomy if not possible) will not enlarge the tear, making it amenable to conversion to a continuous tear with forceps.
If the posterior capsule is intact, OVD is placed in the sulcus to flatten the anterior and posterior capsules into one planar membrane. An opening flap in the posterior capsule is created with a 30-gauge bevel-up needle so as not to engage the delicate hyaloid membrane, which may be directly behind. A cohesive OVD is instilled through the opening into the Berger space to push back the diaphanous anterior hyaloid membrane. A PCCC is then created with forceps, using the anterior capsulorhexis as a guide for sizing to allow capture. Next, the fornix of the capsular bag can be expanded with a cohesive OVD to allow IOL insertion. The haptics are placed in the bag, and the optic is positioned behind the opening in the posterior capsule. Posterior optic capture may be performed even after an IOL has been implanted. The lens is compartmentalized in the anterior chamber with an OVD during PCCC creation and then placed in the bag and captured.
Differences in the thickness and elasticity of the posterior and anterior capsules lead to differences in posterior and anterior optic capture. The posterior capsule has a thickness of 4 µm and is more elastic than the anterior capsule, which has a thickness of 14 µm. A more centripetal direction controls capsulorhexis sizing. During posterior optic capture, the optic edge must be walked under the posterior capsule from one optic-haptic junction to the other to achieve a football-shaped opening. There is no need to remove OVD from behind the captured IOL because it does not have access to the trabecular meshwork and therefore cannot cause an elevation in IOP. Capsular block syndrome cannot occur without an intact capsule.
Forward reverse optic capture can be achieved if the PCCC ruptures during attempted capture of the optic into the Berger space provided the anterior CCC (ACCC) is intact and of adequate size. In this scenario, the haptics remain in the bag, and the optic is lifted from the Berger space, above the broken PCCC and intact ACCC, and into the sulcus. Vitreous rarely presents.
OTHER OPTIONS
Fixation in the presence of a fibrotic capsule. A fibrotic capsule (from prior surgery or trauma) can be strong and resistant to tears. If the IOL cannot be implanted in the bag and membrane optic capture is impossible, then suture fixation of a three-piece IOL to a fibrotic lens capsule with a 10-0 polypropylene suture (Ethilon 7889, Ethicon) on a taper-cut, 13-mm needle (Ethilon CIF-4, Ethicon) may be considered as an alternative option.
Hyaloid-sparing double capture. This technique can be considered if the ACCC and PCCC are intact and appropriately sized. The haptics of a three-piece IOL are placed in the sulcus, and the optic is captured through the anterior and posterior membranes and into the Berger space. There is speculation that this technique may reduce or delay late dislocation of the IOL–capsular bag complex, and a long-term study may soon be initiated with capsular tension ring in patients with pseudoexfoliation. The Bag-in-the-Lens (Morcher) developed by Marie-Jose Tassignon, MD, PhD, FEBO, is placed as a routine surgical choice, although the lens is not available in the United States. In this lens design, the circumference of both capsulorhexis edges are inserted into its collar button haptic. Hyaloid-sparing double capture may also be performed if the vitreous face is open after prolapsed vitreous has been removed.
CONCLUSION
Optic capture is a tried-and-true method of securing and stabilizing an IOL, and its various modifications make it appropriate for a broad range of surgical scenarios. Maintenance of the anterior chamber is crucial during maneuvers following optic capture. Marked shallowing can allow posterior pressure to disengage the optic or lead to vitreous prolapse. Having these techniques at the ready can facilitate optimal outcomes in many difficult surgical scenarios.
1. Arbisser L. Pars plana anterior vitrectomy. In: Fishkind WJ, ed. Phacoemulsification and Intraocular Lens Implantation: Mastering Techniques and Complications in Cataract Surgery. 2nd ed. Thieme; 2017.
2. Chang DF, Masket S, Miller KM, et al; ASCRS Cataract Clinical Committee. Complications of sulcus placement of single-piece acrylic intraocular lenses: recommendations for backup IOL implantation following posterior capsule rupture. J Cataract Refract Surg. 2009;35(8):1445-1458.
3. Arbisser L. What are the earliest intraoperative clues of posterior rupture. In: Chang D, ed. Curbside Consultation in Cataract Surgery: 49 Clinical Questions. 2nd ed. Slack; 2014:135-140.
4. Gimbel HV, DeBroff BM. Intraocular lens optic capture. J Cataract Refract Surg. 2004;30(1):200-206.
5. Gimbel HV, Marzouk HA. Haptic tuck for reverse optic capture of a single-piece acrylic toric or other single-piece acrylic intraocular lenses. J Cataract Refract Surg. 2019;45(2):125-129.
6. Menapace R. Posterior capsulorhexis combined with optic buttonholing: an alternative to standard in-the-bag implantation of sharp-edged intraocular lenses? A critical analysis of 1000 consecutive cases. Graefes Arch Clin Exp Ophthalmol. 2008;246(6):787-801.