CASE PRESENTATION
A 46-year-old man presented with foreign body sensation and blur in his left eye. The patient stated that the symptoms had developed 1 week earlier. He reported no trauma or inciting event.
His history was significant for PRK 5 months earlier. According to the history, 1 day after surgery, bandage contact lenses (BCLs) were in place, and UCVA was 20/30 OU. At 1 week and 3 months, UCVA was 20/20 OU, and the postoperative drug regimen was complete.
The patient had not worn contact lenses since undergoing laser vision correction (LVC). He stated that he was instilling besifloxacin ophthalmic suspension 0.6% (Besivance, Bausch + Lomb) hourly in the left eye in accordance with a prescription issued by his outside provider 4 days earlier.
On examination, UCVA was 20/20 OD and 20/200 OS, not improved with pinhole testing. The pupillary examination was normal. IOP was 7 mm Hg OU. An examination of the left eye was notable for +1 edema in the upper eyelid and +2 conjunctival injection, which was most significant adjacent to the 10 clock position, where there was a peripheral 2.5-mm circumferential corneal ulcer. Seventy percent thinning of the ulcer was evident in the superior nasal aspect of the lesion. There was no obvious infiltrate, but there was +1 corneal edema with Descemet folds tracking to the location of the ulcer. A 1.5-mm hypopyon with +2 cell and flare was observed in the anterior chamber (Figure 1). An examination of the crystalline lens, iris, and posterior segment was normal.

Figure 1. Slit-lamp photograph of the left eye.
How would you proceed?
—Case prepared by Casey Komm, DO, and Karl G. Stonecipher, MD

FRANCIS S. MAH, MD
Without a distinct infiltrate and although a bacterial, fungal, or even parasitic pathogen cannot be excluded, my thinking would shift to a viral, inflammatory, or autoimmune cause; a masquerader such as tuberculosis; or syphilis. I would obtain a panculture for bacteria, fungus, and Acanthamoeba in addition to sending swabs for herpes simplex virus (HSV) and varicella-zoster virus (VZV) for testing using polymerase chain reaction (PCR). I would also refer this patient for a rheumatology consultation to rule out a cause for peripheral ulcerative keratitis (PUK).
I would prescribe topical fortified tobramycin and cefazolin hourly, bacitracin ointment four times daily, oral valacyclovir 1 g three times daily, oral doxycycline 100 mg twice daily, and vitamin C 1,000 mg daily. Because of the significant melting and the possible risk of perforation, I would place either a BCL with high oxygen transmissibility or a self-retaining amniotic membrane.
The fact that the patient reports foreign body sensation but not significant pain despite the corneal melting, edema, and exuberant inflammatory response makes me suspect a neurotrophic issue. It is well documented that PRK, and more so LASIK, can affect the corneal basal nerve plexus, which can result in neurotrophic or even neuropathic issues. Acanthamoeba is low on the list of possible etiologies because it is associated with significant pain, out of proportion to the appearance. Moreover, this is not the classic way that Acanthamoeba presents. PUK is also usually extremely painful, but the significant melting and the spot on the cornea still have me suspicious. On initial examination, I would lean most toward HSV or VZV in concert with the recent PRK’s causing a neurotrophic issue.
While awaiting the results of laboratory testing and the rheumatology consultation, I would assume that the diagnosis is neurotrophic keratitis and plan my next steps to heal this gentleman. I would continue the doxycycline, vitamin C, and either the BCL or the self-retaining amniotic membrane. Serum drops at 75% to 100% concentration or amniotic extract drops could be considered. Another option is cenegermin-bkbj ophthalmic solution 0.002% (20 µg/mL, Oxervate, Dompé), which is a recombinant nerve growth factor. This relatively new drug represents a huge advance in the management of neurotrophic keratitis. In clinical trials performed in the United States and Europe, more than 72% of patients with persistent epithelial defects, frank ulceration, and corneal melting experienced healing within 8 weeks with treatment six times a day. More astounding was that, of the 72% who healed, 80% maintained the integrity of their corneal epithelium for up to a year after the cessation of treatment.1


NEEL S. VAIDYA, MD, MPH, AND PARAG A. MAJMUDAR, MD
Ulcerative keratitis after LVC is a rare but potentially devastating complication. As with any surgical procedure, thorough preoperative preparation of the surgical field (ocular surface, lids, and lashes) and proper sterilization of all surgical equipment are of paramount importance. Infectious keratitis after LVC has been linked to a variety of pathogens. Aggressive keratitis that presents early in the perioperative period is often bacterial in nature, with gram-positive Staphylococcus and Streptococcus species predominating (although gram-negative pathogens have been implicated as well). Keratitis that occurs weeks or months after LVC has been associated with both gram-positive and gram-negative bacterial pathogens as well as atypical mycobacteria and fungi. Viral keratitis, primarily keratitis associated with HSV or VZV, has also been reported. There are case reports of autoimmune noninfectious (sterile) keratitis after LVC in the literature. As such, a history of autoimmune disease should be carefully considered in any LVC candidate.
This patient presented with diffuse injection, a peripheral corneal ulcer with substantial thinning, and a hypopyon. Given the delayed onset of presentation and the peripheral nature of the ulcer, it is possible, if not likely, that the process may be unrelated to the history of LVC. Although the absence of posterior segment findings is reassuring, the corneal and anterior segment examination dictates that time is of the essence.
Cases such as this one must be treated as infection until proven otherwise. As with any corneal ulcer, samples should be obtained and sent for aerobic/anaerobic and fungal culture as well as HSV and VZV PCR. Given the delayed presentation, an evaluation for mycobacterial species should also be obtained. If the patient were status post-LASIK and inflammation were confined to the flap interface, the LASIK flap could be carefully lifted, and the flap bed could be swabbed and then irrigated with antibiotic solution. Because of the substantial thinning of the peripheral cornea and the postoperative nature of the ulcer (albeit several months after LVC), fortified antibiotics should be initiated and administered hourly. Empiric oral coverage for HSV and VZV (acyclovir, valacyclovir, famciclovir) may be initiated as well. If an impending perforation is suspected, the cornea can be temporized with the application of cyanoacrylate glue. Owing to their anticollagenolytic properties, oral doxycycline and vitamin C can help delay further corneal thinning. If endophthalmitis is suspected, a vitreous tap and intravitreal injection of antibiotics should be pursued.
The patient should be seen daily and monitored closely for further corneal thinning or perforation. Culture results and sensitivities should help direct management. A lack of improvement or progression with the management strategy just described should prompt further workup, possibly including a corneal biopsy. Once an infection has been ruled out, sterile keratitis secondary to autoimmune disease should be considered. A laboratory evaluation for rheumatologic disease (antinuclear antibodies test, erythrocyte sedimentation rate, C-reactive protein, cytoplasmic antineutrophil cytoplasmic antibodies [ANCA], perinuclear ANCA) should be performed. If clinical suspicion of an inflammatory etiology is high and an infection has been ruled out, topical and/or systemic steroids (in conjunction with rheumatology) can be cautiously initiated.

AUDREY R. TALLEY ROSTOV, MD
Any time a patient presents with an infiltrate and hypopyon, a diagnosis of microbial keratitis should be considered. This patient has had good UCVA and an unremarkable postoperative course since undergoing PRK. It is unlikely that a refractive procedure performed 5 months ago is related to the current acute corneal infiltrate. Unusual features of this case are the 70% thinning and the very peripheral location of the infiltrate.
I would culture the eye for bacterial and fungal pathogens and perform gram and fungal stains. The hourly administration of besifloxacin can affect culture results, producing a false negative for bacteria. I would therefore start the patient on fortified vancomycin and fortified tobramycin instead, await the culture results, and monitor his clinical response.
Because of the dramatic thinning of the cornea and the peripheral location of the infiltrate, I would initiate therapy with oral doxycycline and obtain a vasculitis workup with an antinuclear antibodies test, ANCA, rheumatoid factor test, C-reactive protein, erythrocyte sedimentation rate, comprehensive metabolic panel, and complete blood count as well as test for fluorescent treponemal antibody absorption and hepatitis C and human immunodeficiency viruses. I would be sure to inquire about symptoms suggestive of rheumatoid arthritis, Crohn disease, ulcerative colitis, sarcoidosis, and Wegener granulomatosis. I would consider obtaining a chest x-ray as well. I would direct therapy based on the results of these tests and the patient’s clinical response.
If the patient’s condition is improving on topical fortified antibiotics, I would stay the course, even if the culture results come back negative. If the culture results are negative and any of the blood work shows active inflammation, I would initiate therapy with oral prednisone. If the culture results are negative and there is no clinical response on fortified antibiotics, I would consider treating the perforation with corneal glue, scheduling a consultation with rheumatology, and, if the condition is worsening, starting antifungal therapy.


WHAT WE DID: CASEY KOMM, DO, AND KARL G. STONECIPHER, MD
The ulcer was cultured for bacterial and fungal species, and samples for HSV and VZV PCR were sent for testing. These all ultimately came back negative. The patient was started on valacyclovir 500 mg three times daily, doxycycline 100 mg two times daily, vitamin C 500 mg daily, and fortified vancomycin and gentamicin drops every hour around the clock.
One day later, UCVA was 20/100, but no improvement in the size of the ulcer or hypopyon was observed. Given the lack of infiltrate and the peripheral nature of the ulcer, our differential diagnosis included an autoimmune etiology and masquerading bacterial species. Samples were sent to the laboratory for a complete blood count, basic metabolic panel, urinalysis, rheumatoid factor test, angiotensin-converting enzyme test, ANCA, QuantiFERON-TB Gold, and syphilis screening.
Examination findings were stable 2 days later. All cultures continued to be negative, and PCRs for HSV and VZV were negative. The results of laboratory testing, however, raised concern. They were positive for ANCA and the proteinase 3 antigen and showed moderate blood in the patient’s urine. Based on these findings, he was admitted to the hospital for further workup and treatment because we considered this to be atypical PUK in the setting of ANCA vasculitis. Upon admission, additional laboratory testing was done, including a toxicology screen that was positive for cocaine and cannabinoids.
The patient was started on intravenous methylprednisolone (Solu-Medrol, Pfizer) 500 mg daily for 3 days, and rheumatology and nephrology consultations were scheduled. After just 1 day of intravenous steroids, the hypopyon resolved, and the corneal edema improved. Persistent corneal thinning at the superior nasal aspect of the ulcer prompted us to apply a tissue adhesive (Histoacryl, B. Braun) to the area of concern and place a BCL (Kontur lens, Kontur Kontact Lens).
After several days, UCVA was 20/40. The patient underwent a sinus evaluation and kidney biopsy to rule out sinus and kidney involvement. Computed tomography showed erosive sinus disease, which was thought to be a result of cocaine abuse, and a kidney biopsy was negative for glomerulonephritis. We hypothesized that the positive results for ANCA and proteinase 3 antigen were a result of his cocaine dependency, which he did not disclose until after a positive drug screen.
Levamisole is an antihelminth drug and a common cocaine contaminant. Levamisole is believed to potentiate cocaine’s euphoric effects, and it is present in an estimated 71% of cocaine samples in the United States (Figure 2).2 The use of cocaine contaminated by levamisole has been linked to an ANCA-associated vasculitis.2,3 The pathogenesis and prevalence of levamisole-induced vasculitis in patients who use cocaine is unclear, but researchers speculate that a byproduct of levamisole may play a role.3,4
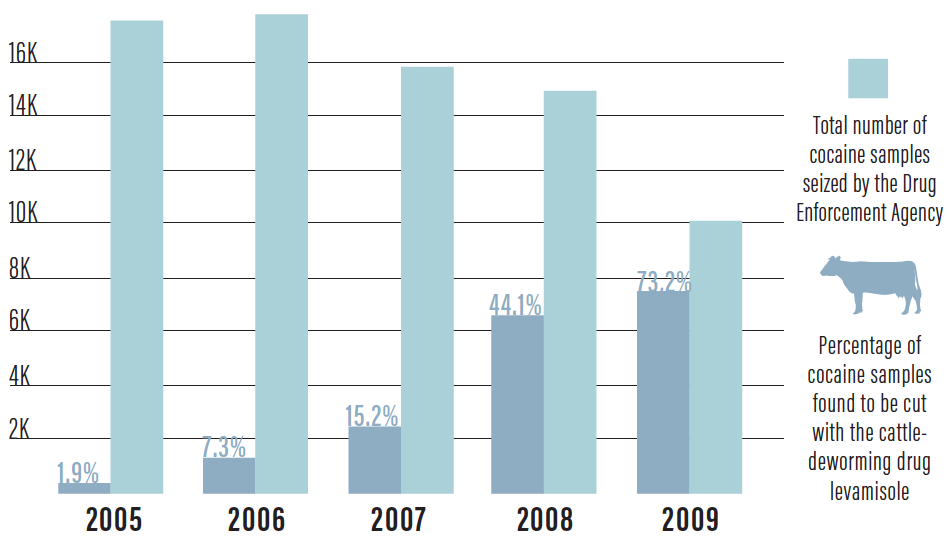
Figure 2. US prevalence of levamisole in cocaine. Adapted from the US Drug Enforcement Agency.
Purpura is the most common initial presentation of vasculitis associated with the use of cocaine contaminated with levamisole.2,5 Although our patient did not have this specific skin finding, cocaine is also associated with autoimmunity formation, and it is conceivable that exposure to both drugs contributes to the formation of ANCA vasculitis.2
The main treatment of cocaine-induced vasculitis is abstinence.4 Systemic corticosteroids are also used in the treatment of this condition,2-4 and a multidisciplinary approach is necessary to properly care for these patients. After 3 days of intravenous methylprednisolone, our patient was transitioned to oral prednisone 1 mg/kg/day and discharged for outpatient follow-up.
One week later, the glue and BCL were still in place, and UCVA was stable at 20/40. At the 3-week follow-up visit, the glue had become dislodged, so the BCL was removed. The conjunctival injection had dissipated. The ulcer was scarred, thinning had improved to approximately 40% depth, and there was corneal neovascularization into the affected area.
Compliance with follow-up visits is a challenge with this patient. We have encouraged him to continue to follow up with our office, with rheumatology, and with his primary care physician.
1. Oxervate (cenegermin-bkbj) ophthalmic solution 0.002% (20 mcg/mL). Package insert. Dompé U.S. Inc.; 2018.
2. Jin Q, Kant S, Alhariri J, Geetha D. Levamisole adulterated cocaine associated ANCA vasculitis: review of literature and update on pathogenesis. J Community Hosp Intern Med Perspect. 2018;8(6):339-344.
3. George TC, Freet DJ, Cross JM, Huzar TF. Levamisole–induced vasculitis. JAAPA. 2019;32(1):23-27.
4. Kiley B. The mystery of the tainted cocaine. The Stranger. August 17, 2010. Accessed August 7, 2020. https://www.thestranger.com/seattle/the-mystery-of-the-tainted-cocaine/Content?oid=4683741
5. Marquez J, Aguirre L, Muñoz C, Echeverri A, Restrepo M, Pinto LF. Cocaine–levamisole–induced vasculitis/vasculopathy syndrome. Curr Rheumatol Rep. 2017;19(6):36.




