Sealing the microincision at the conclusion of cataract surgery is crucial to maintaining the structural integrity of the eye and preventing complications due to wound leakage such as hypotony, corneal edema, and IOL dislocation. Furthermore, a competent wound prevents postoperative ingress of bacteria that can result in endophthalmitis. In the era of refractive cataract surgery, a well-constructed, astigmatically neutral wound is necessary to achieve the planned refractive visual outcome and satisfy the patient.
The self-sealing clear corneal temporal wound typically incorporates both horizontal and vertical components. It can be created with a diamond or steel keratome or with a femtosecond laser. A wound length of 1 to 2 mm is recommended to ensure adequate wound closure. If the incision is too short, the wound may be incompetent. If it is too long, the length of the tunnel may lead to intraoperative striae or oar-locking of instruments.
STROMAL HYDRATION
At the conclusion of surgery, the wound can be examined for competence by application of fluorescein, gentle indentation of the proximal sclera, or visual inspection after drying with a cellulose sponge (Weck-Cel, BVI).
Stromal hydration is an effective means to stem the leakage from most spontaneously leaking cataract incisions. It is typically employed by delivering balanced salt solution via a 30-gauge cannula into the corners and internal roof of the incision. Stromal hydration swells the corneal lamellae, forcing them to abut and close the incision. The hydration is a temporizing measure until the corneal endothelial pump can further seal the incision. Postoperative corneal OCT has demonstrated that the effects of stromal hydration can last up to 1 week postoperatively.
Stromal hydration should be employed in the main corneal incision and the sideport incisions. A modification of traditional stromal hydration is the Wong pocket.1 This term refers to creation of an extra nonpenetrating incision anterior to the main wound that, when stromal hydration is applied, puts downward pressure on the main wound to achieve good wound closure. The pocket can be created either with a keratome or with a femtosecond laser.
WHEN STROMAL HYDRATION IS INSUFFICIENT
If wound leakage is still present after stromal hydration, further action is needed. Until recently, sutures were the only option to achieve better closure. Radial, mattress, x-shaped, and other suture techniques, using 10-0 nylon or other materials, can be effective in sealing the wound. However, sutures can induce astigmatism and, if not tended to postoperatively, can break and lead to foreign body sensation, suture abscess, or worse.
Recently, the concept of using adhesive ocular sealants for watertight corneal wound closure was introduced. As of this writing, there is one FDA-approved product for this indication: ReSure Sealant (Ocular Therapeutix). Studies have shown that this sealant has excellent efficacy in both stemming wound leak and preventing conjunctival fluid ingress. A head-to-head study comparing sutures versus the sealant found that the sealant was more effective in preventing fluid egress with provocation and that it was associated with fewer postoperative adverse events.2
ReSure Sealant is reconstituted by mixing its two components. A few drops are then applied to the cataract and paracentesis wounds at the conclusion of surgery. The sealant has a faint blue dye to enhance visibility. For the patient, the presence of the sealant is asymptomatic, with no foreign body sensation, and it clears in the first postoperative week.
CLINICAL SCENARIOS
An incompetent corneal wound can occur for multiple reasons, including poor architecture or intraoperative tearing, stretching, or thermal injury of the wound. Incisions should be properly sized for the phaco needle and sleeve and for the IOL insertion device to be employed. It is better to have a clean 2.4-mm incision than a stretched and damaged 2.2-mm incision.
Fortunately, the risk of thermal wound injury has been reduced with the introduction of phaco power modulation protocols such as torsional and transversal ultrasound. Thermal injury can be further minimized by ensuring adequate cooling flow through the phaco sleeve. One way to facilitate this is by clearing an OVD-free zone centrally before engaging the ultrasound.
There are other clinical scenarios in which I use ocular sealant even in the absence of a gross leak (Table). For example, in any case in which even modest postoperative shallowing can be deleterious, the incision should be closed with sealant. Examples include most cases with capsular compromise, such as anterior capsular tear, posterior capsular tear, or dialysis. In these scenarios, incidental postoperative shallowing can lead to vitreous prolapse or IOL dislocation.
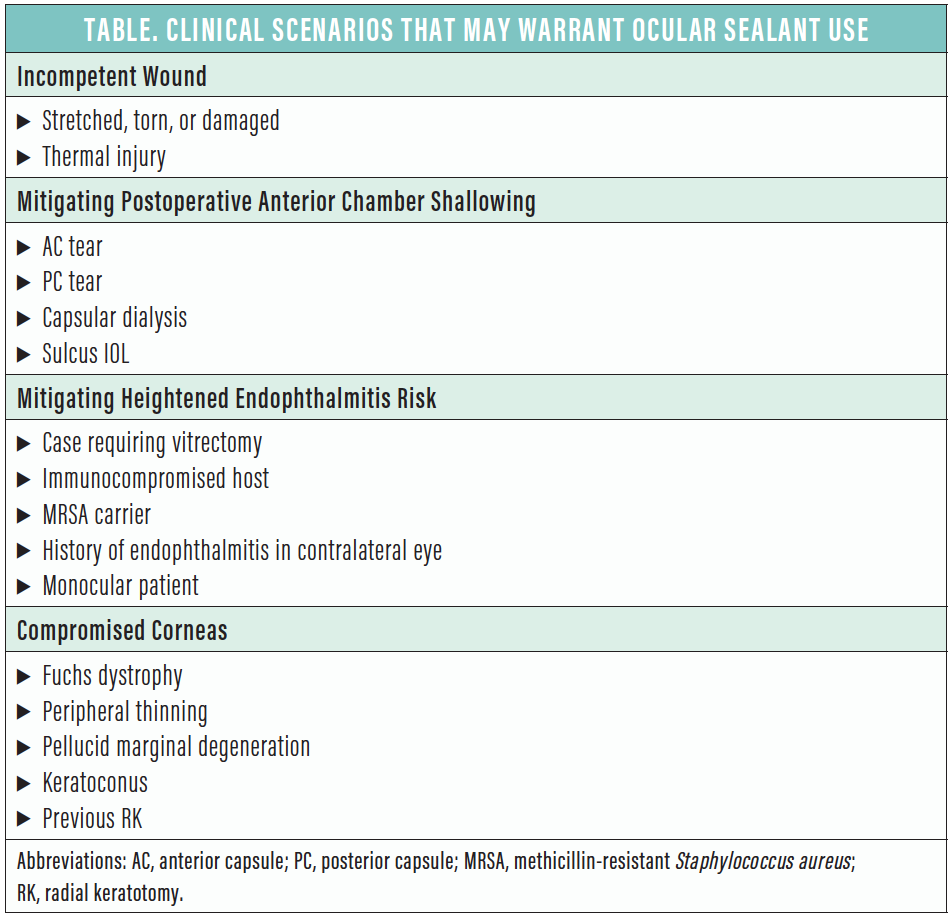
Another instance in which I use sealants is when there is an increased risk of endophthalmitis. This can include any primary case in which anterior vitrectomy was required or many secondary IOL procedures. An immunocompromised patient, a patient with methicillin-resistant Staphylococcus aureus infection, or a patient who has had endophthalmitis in the contralateral eye are also good candidates for use of sealants to ensure the most watertight of wound closures.
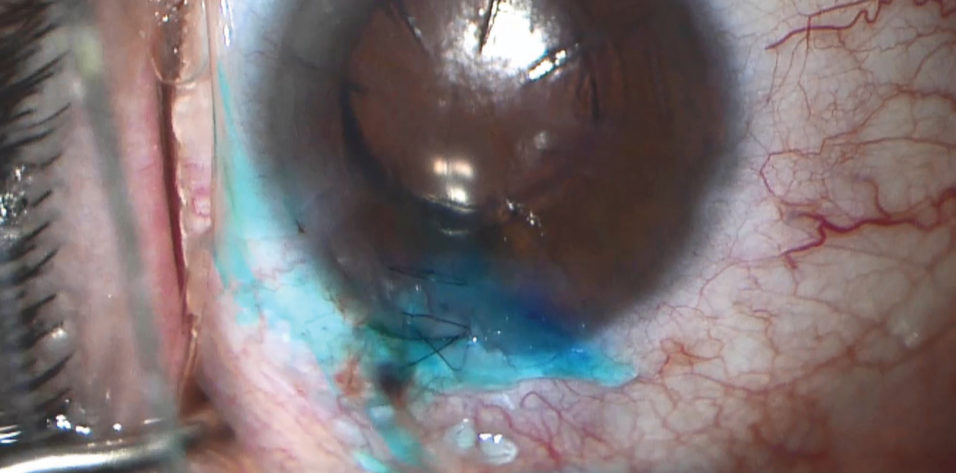
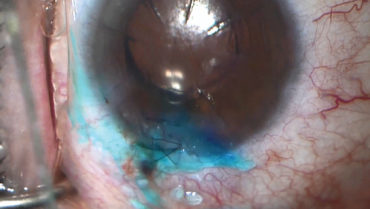
Finally, patients with compromised corneas may also require extra care with a wound sealant. This includes patients with Fuchs dystrophy, in which the eye’s compromised endothelial pump may not adequately seal the wound after stromal hydration has worn off. Corneal wounds in eyes with peripheral thinning, pellucid marginal degeneration, keratoconus, or previous radial keratotomy (RK) can also benefit from closure with sealant. In severe instances such as the intraoperative opening of RK wounds, both sutures and sealant may be needed for the most effective closure (Figure).
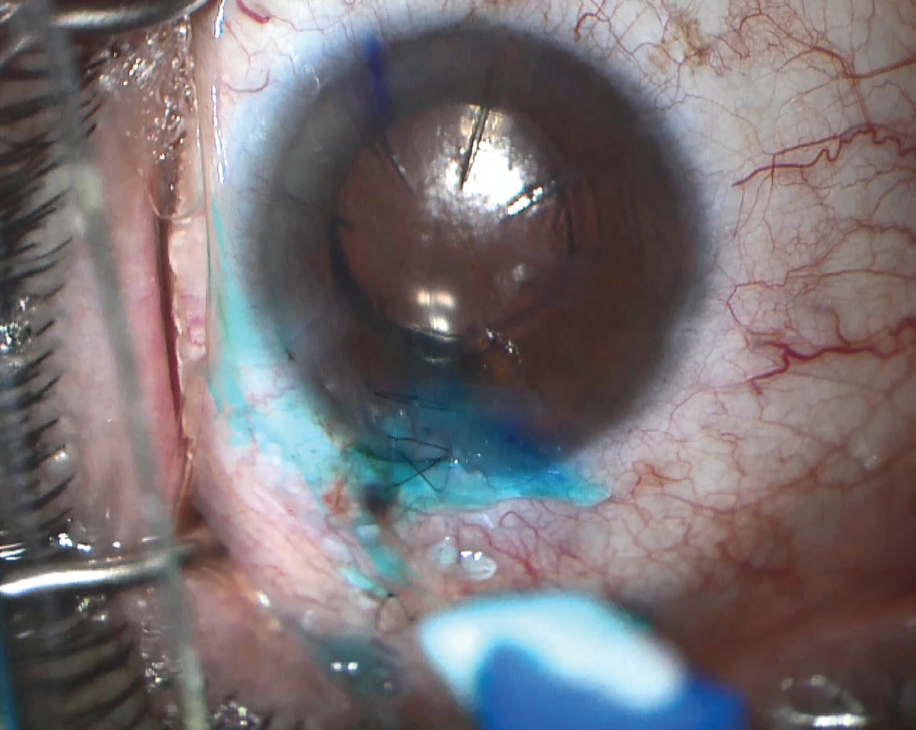
Figure. In this case of an RK incision splitting at the phaco wound, a combination of sutures and sealant was used to achieve a watertight closure without inducing significant astigmatism.
CONCLUSION
With proper wound architecture, good surgical technique, and effective stromal hydration, the vast majority of cataract surgery microincisions seal well and are adequate to prevent postoperative complications. If stromal hydration is insufficient, or in certain clinical scenarios such as those described here, sutures and sealants can be employed to further buttress wounds and ensure excellent outcomes.
1. Wong MY. Securing clear corneal incisions. Cataract & Refractive Surgery Today website. March 2003. https://crstoday.com/articles/2003-mar/0303_051-html. Accessed February 27, 2019.
2. Masket S, Hovanesian JA, Levenson J, et al. Hydrogel sealant versus sutures to prevent fluid egress after cataract surgery. J Cataract Refract Surg. 2014;40(12):2057-2066.