Laser Cataract Surgery for Traumatic Cataracts
Some common presentations of traumatic cataract are best managed by laser cataract surgery.
By Sartaj Grewal, MD; and Surendra Basti, MD


Traumatic cataracts usually present with a wide variety of associated ocular morbidities, and they pose a challenge for even the most experienced cataract surgeons. Some of the challenges surgeons can face are white intumescent cataracts, tears in the anterior or posterior capsule, subluxated lenses, zonular dehiscence, and vitreous in the anterior chamber. We believe laser cataract surgery is an excellent choice in such situations to help reduce the risk of complications and improve outcomes.
A closed-chamber capsulotomy and nuclear fragmentation are only possible with laser cataract surgery, and they can increase the chance of successful IOL implantation in the bag. Integrated, high-resolution, 3D spectral-domain OCT and infrared imaging are helpful in planning and monitoring laser treatment in the setting of diverse traumatic cataracts. Published case studies show that laser cataract surgery has been used successfully in eyes with damaged lens capsules, posttraumatic subluxated cataracts, and traumatic cataracts with corneal scars after trauma.1-7
Our section of this article outlines three common presentations of traumatic cataract and discusses the value of laser cataract surgery in such cases.
PRESENTATION NO. 1
Intumescent and white traumatic cataracts with intact capsules are a common presentation after blunt trauma. Intumescent cataracts make it difficult to achieve an optimally sized and centered continuous curvilinear capsulorhexis (CCC). The increased intralenticular pressure increases the risk of an errant CCC. Laser cataract surgery has the advantage of creating a circular, perfectly centered capsulotomy in these eyes, significantly reducing the chance of complications. These lenses are usually soft and easily managed with aspiration alone.1-3
PRESENTATION NO. 2
A second scenario after blunt or nonpenetrating trauma is a closed-globe injury resulting in posterior capsular rupture (PCR) with an associated cataract. The challenge in these cases is to remove lenticular material while minimizing the transfer of forces to the margins of the ruptured posterior capsule and zonules. Hydrodissection and nuclear rotation during phacoemulsification increase the risk of extending a preexisting PCR.
Laser cataract surgery can achieve a circular capsulotomy and divides the nucleus into six to eight segments. This permits nuclear removal with gentle hydrodelineation alone, and laser segmentation of the nucleus combined with low-flow techniques permits nuclear removal without the need for rotation. It is important to increase the posterior capsular safety margin from the conventional 500μm to minimize laser energy delivery and cavitation near the posterior lens surface. Lens fragmentation should be minimal, and softening should be avoided to prevent the formation of excessive cavitation bubbles. Segment repetitions can also be reduced to help reduce gas bubble formation. A well-centered and properly sized capsulotomy made with a laser facilitates optic capture of an IOL placed in the sulcus (Figure 1).6
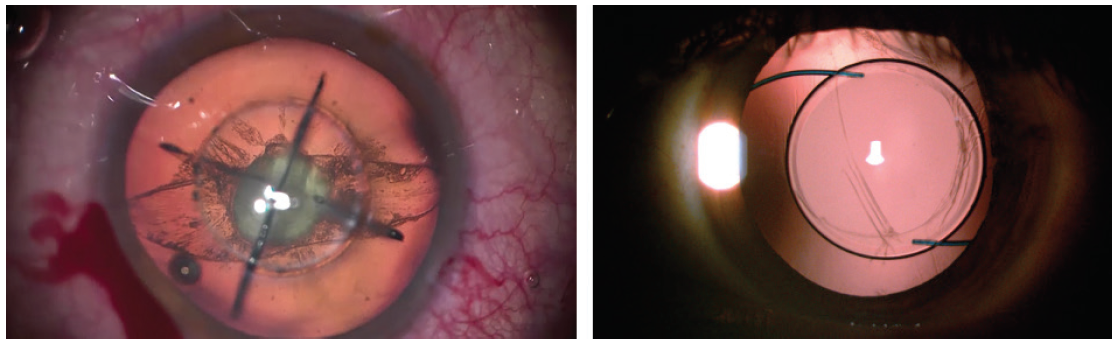
Figure 1. Preexisting PCR and a large equator-to-equator posterior capsular tear. A complete and free-floating 5-mm capsulotomy and quadrant fragmentation of the lens are also visible (left). Postoperatively at the slit lamp, optic capture of the IOL is visible with 360º capsular overlap of the IOL optic (right).
PRESENTATION NO. 3
A posttraumatic subluxated cataract presents challenges. Successful cataract surgery in such cases requires an adequately sized and well-centered CCC to allow use of endocapsular support to stabilize the capsular bag. A CCC can be difficult to perform in the absence of zonular countertraction, and excessive manipulation can further weaken zonular support. Entering and decompressing the anterior chamber can precipitate the prolapse of vitreous through the area of zonular dialysis, further complicating surgery. Even the use of excessive OVD to help stabilize the chamber during CCC can place additional stress on the zonules, push the lens posteriorly, and worsen tilt.
Laser cataract surgery allows the ophthalmologist to create a capsulotomy and fragment the nucleus in a closed chamber prior to opening the anterior chamber. This reduces stress on the zonules and decreases the chance of anterior prolapse of the vitreous. Intraoperative 3D OCT allows the surgeon to center the capsulotomy on the capsular bag rather than the pupil, and he or she can use capsular hooks to support the capsular bag before attempting to manipulate the lens. Fragmentation of the nucleus in adult patients further reduces intraoperative stress on the zonules. A closed-chamber capsulotomy that is centered on the subluxated capsular bag and nuclear fragmentation can be achieved only with laser cataract surgery (Figure 2).7
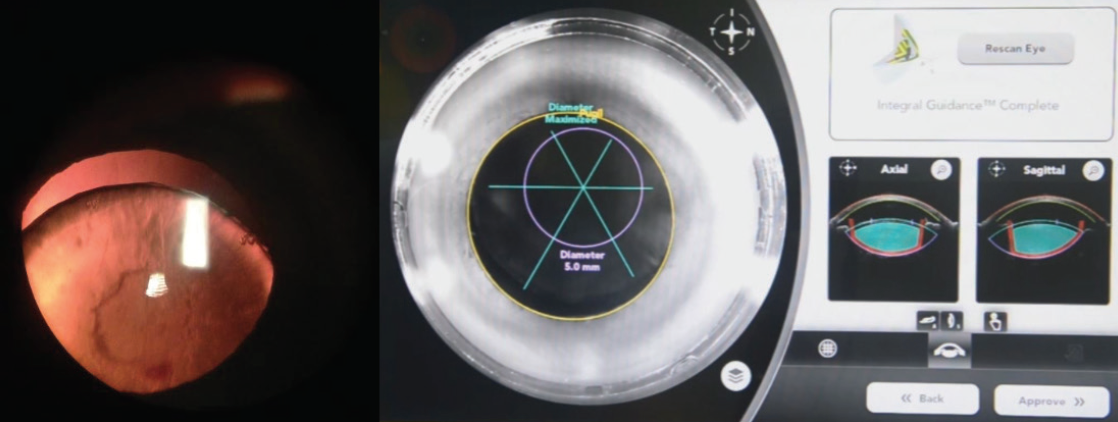
Figure 2. Preoperatively, a subluxated traumatic cataract and loss of zonules are evident (left). An intraoperative infrared camera and anterior segment OCT imaging show a 5-mm capsulotomy centered on the capsular bag instead of the pupil. Lens fragmentation is centered on the capsular bag (right).
CONCLUSION
Femtosecond laser treatments can be customized to help achieve many advantages over phaco cataract surgery in most cases of traumatic cataract. Laser cataract surgery is of no significant value in eyes that have traumatic cataracts and extensive tears of the anterior capsule, but the approach has advantages over manual techniques for several common presentations of traumatic cataracts as discussed earlier. Experience with the laser platform is imperative, and surgeons should understand the various modifications that are possible to achieve desired outcomes in such cases.
1. Nagy ZZ, Kránitz K, Takacs A, et al. Intraocular femtosecond laser use in traumatic cataracts following penetrating and blunt trauma. J Refract Surg. 2012;28(2):151-153.
2. Conrad-Hengerer I, Hengerer FH, Joachim SC, et al. Femtosecond laser-assisted cataract surgery in intumescent white cataracts. J Cataract Refract Surg. 2014;40(1):44-50.
3. Titiyal JS, Kaur M, Singh A, et al. Comparative evaluation of femtosecond laser-assisted cataract surgery and conventional phacoemulsification in white cataract. Clin Ophthalmol. 2016;10:1357-1364.
4. Conrad-Hengerer I, Dick HB, Schultz T, Hengerer FH. Femtosecond laser-assisted capsulotomy after penetrating injury of the cornea and lens capsule. J Cataract Refract Surg. 2014;40:153-156.
5. Grewal DS, Basti S, Grewal SPS. Customizing femtosecond laser-assisted cataract surgery in a patient with a traumatic corneal scar and cataract. J Cataract Refract Surg. 2014;40:1926-1927.
6. Grewal DS, Grewal SPS. Femtosecond laser-assisted cataract surgery in pre-existing posterior capsule rupture following closed globe injury. Clin Exp Ophthalmol. 2015;43(5):478-480.
7. Grewal DS, Basti S, Grewal SPS. Femtosecond laser-assisted cataract surgery in a subluxated traumatic cataract. J Cataract Refract Surg. 2014;40:1239-1240.
Traumatic Cataract Surgery Made Safer
The miLoop can eliminate the need for phacoemulsification in eyes with dense nuclei.
By Michael Patterson, DO

Advances in phaco technology have made cataract surgery much safer over the years. Improved efficiency means less energy is needed in the eye, further enhancing safety and likely speeding up the healing process. Cataract surgery with phacoemulsification is not an option in some parts of the developing world, however, because of the machines’ size and cost. Additionally, even with the best phaco technology available, some patients require an exceedingly gentle procedure that minimizes manipulation during lens removal and lessens trauma to the endothelium and zonules.
The miLoop (Carl Zeiss Meditec, formerly IanTech) allows mechanical cataract disassembly with minimal use of phaco energy. The single-use, disposable device has a microthin, elastic, self-expanding nitinol filament (the loop) that is used to fragment any grade of cataract. The surgeon deploys the retractable loop in the capsular bag to encircle the cataractous lens. Retracting the loop effectively bisects the lens. The loop can be redeployed multiple times to break a lens into smaller, more manageable pieces. The loop’s shape is meant to complement the anatomy of the capsular bag for safety. Nitinol is stiff enough to allow manipulations in the bag, but it is also flexible enough to avoid damaging the bag and zonular structures.
VERSATILITY, CONVENIENCE, AND SAFETY
I participate in medical mission work where we do not usually have access to a working phaco machine. The machines are much too large and expensive to travel with, not to mention the need for surgical packs. Using the miLoop for cataract surgery in the jungles of Montellano, Guatemala, for example, without the need for phacoemulsification, will be a game-changer for humanitarian work. I believe the device could have an important role in US cataract practices as well.
I can use the tool to safely cut up cataracts in eyes with very dense nuclei, pseudoexfoliation, and loose zonules. The device puts minimal, if any, stress on the zonules, and it bisects the lens with a smooth cut. In my experience, many patients who would benefit from laser surgery cannot afford it. I have found cataract fragmentation with the miLoop to be efficient, and, by the time I am finished disassembling the lens, it is easily removable with the phaco tip needle or simple irrigation and aspiration.
PEARLS FOR USE
Because it eliminates the need for pushing and pulling on the bag with a phaco tip and a chopper, the miLoop provides an advantage in eyes with traumatic cataracts and loose zonules.
I deploy the device under the capsule with a slow, sweeping motion, stripping the cortex. I find that irrigation and aspiration are almost instantaneous. The cataract can be rotated with a second device or with the miLoop during retraction of the loop. I then slice the nucleus into a couple of pieces, and the nitinol filament pops back up into the anterior chamber. At this point, I can easily aspirate the pieces with very little energy. Even for dense brunescent cataracts, I use much less energy, which is safer for the cornea.
I slice the cataract into two pieces by cinching the miLoop, while applying slight downward pressure so the device does not rise too quickly. I can then rotate the loop, move the lens, and slice it again. The tool can be deployed over and over during the procedure. Once the dissection is finished, I pull the device out of the eye. The pieces move easily to the phaco tip, and the entire procedure is quick; I have found that surgery takes about 5 to 6 minutes from my first cut to drape removal.
The miLoop can be used in eyes with small pupils, it loosens cortical material, and it works independently of nuclear density. There is no variability in a hard cataract, and the device is gentle on ocular structures.
CONCLUSION
With the nitinol loop designed to slip under the anterior capsule and fully ensnare the lens, the miLoop enables surgeons to achieve full-thickness lens fragmentation no matter the density of the cataract. The tool minimizes the need for phaco energy, thereby lessening ultrasonic vibration in the eye and making surgery safer in eyes with small pupils, traumatic cataracts, loose zonules, and other complexities.




