To kick off 2019, CRST is honoring some of the notable contributors to the BMC Vision family of publications with the Resolute Award.
We invited a few of these notable contributors to comment on their best time-savers in the OR, and we are pleased to share their replies here.

LISA BROTHERS ARBISSER, MD | JOHN A. MORAN EYE CENTER, SALT LAKE CITY, UTAH
Efficiency and Communication in the OR
I believe that an important way to promote efficiency in the OR is to make sure everyone is on the same page at all times. This is helpful for the staff, and it serves to improve the patient’s confidence. Before surgery, I initiate routine conversation with the patient and the patient’s family members if they will be viewing through a feed from the microscope in a remote room. In my experience, patients gain a sense of safety and control when they are informed beforehand of what to expect during their procedure. They also feel more empowered to communicate discomfort, which helps improve cooperation during the procedure. Just as a flight crew makes a scripted announcement to passengers about safety before taking off, I go through a routine conversation to keep everyone well-informed about our goals in the OR.
I tell patients, “Naturally, you will be aware of my presence, but you should feel no pain. If anything bothers you, let us know, and we will do something about it right away. The light is bright, but you will rapidly adjust; it may come and go and change color, and that is normal. You might feel a slight sting. If you do, it is us administering extra anesthetic for your comfort, and it will only last a moment. Look toward the light. Even if it appears to move, your goal is to hold your eye steady just as you have it. Look straight ahead and enjoy the light show.”
My conversation often continues during surgery, depending on the patient’s anxiety level, with every word chosen for its psychologic effect and describing our efficient progress. The staff finds it very comforting as well, and my monologue tells them exactly which step of the procedure I am performing.
In the event of a complication, I simply say the word “timing.” Everyone knows this is the cue to get the vitrectomy kit and to suspend draping in the other OR.
Additionally, we have a personal hearing device with a speaker earphone, which is used to replace the patient’s hearing aid on the side of the draped eye. A microphone is attached to my surgical mask, so the patient hears only my voice. For deaf or hard-of-hearing patients, I designate signals preoperatively: Touching the tip of the nose means “look straight ahead”; touching the forehead means “hold still”; and touching the shoulder assures him or her that “all is going well.”
There is no anesthetic as safe and effective as the vocal local.

ARTHUR CUMMINGS, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin) | WELLINGTON EYE CLINIC AND BEACON HOSPITAL, DUBLIN, IRELAND
Keeping Things Moving
There are two significant steps my team and I take to improve efficiency in the OR:
No. 1. My team takes care of the signing of necessary consent forms, as well as the marking of the patient’s eye, before the patient is moved into the OR. When the patient arrives, he or she is ready to go, which really helps speed up the process.
No. 2. I have a summary sheet with the names of the patients to be treated and relevant information, including which eye is having surgery, IOL selection and power, choice of anesthesia, and more. My OR team and I routinely reference this summary during the session.
In a specialized eye unit, one can go a lot further than I can do in the hospital I work in, where a lot of general surgery is also performed. In hospitals that I have worked in previously, the scrub nurse would start cleaning and draping the patient while I was still writing my notes from the previous case. By the time I had scrubbed and entered the OR, I was basically ready to make the first incision (ie, the eye had been cleaned and draped and was ready for surgery).

STEVEN J. DELL, MD | DELL LASER CONSULTANTS, AUSTIN, TEXAS
Many Little Things Add up
When it comes to workflow efficiency in the OR, it is not one thing but rather the sum of many little things that contributes to better performance. For surgeons working with a high volume of cases, small inefficiencies add up to a lot of lost time. This does not mean I recommend rushing through cases. Rather, in my experience, the best way to speed up is to slow down. Be mindful, contemplative, slow, and deliberate with all of your movements in the OR. If your scrub technicians are constantly rushing to keep up with you, they will likely be flailing all over the place and making errors. Tell them to slow down, and they will be faster.
Pay attention to where your toughest cases occur in the day’s surgical lineup. Some surgeons prefer to schedule tough cases at the end of the day to allow for unpredictable complications. Other surgeons prefer to have these cases at the beginning of the day. Some days, it seems that all of the cases are unusual and require special considerations. Find the pattern that works best for you and adhere to it.
Teach your staff where you want the height of the surgical table, microscope, and chair when you enter the room. Pay attention to ergonomics. Have someone photograph you sitting at the surgical microscope from different angles, both at the beginning and toward the end of a case. Avoid raised shoulders, a hunched back, and a hyperextended neck. If necessary, invest in better chairs. Take some time in an empty OR to figure out a comfortable ergonomic position, and re-create that configuration during surgery.
Before you enter the OR, have your staff coach patients on what they should and should not do during surgery and where they should attempt to fix their gaze. Take a few extra seconds to carefully plan your wound construction. This will pay dividends later in the case. The nature of cataract surgery is such that each step either provides a good foundation or complicates the subsequent steps.
Don’t waste effort during a case. I often see surgeons perform a maneuver such as hydrodissection and then reperform it once or twice more, just to be sure. In most cases, this is wasted energy and effort. Perform each step properly and confidently and then move on to the next step. If you perform a phaco-chop technique, one good chop beats a dozen tentative, ineffectual ones. Your goal should be to operate steadily, calmly, and efficiently. Get in and out of the eye before it has a chance to know you’ve been there.

D. BRIAN KIM, MD | PROFESSIONAL EYE ASSOCIATES, DALTON, GEORGIA
Leading by Example
As I contemplated my best OR time-saver for this article, I thought about possible things such as a special technique or a pearl on workflow efficiency. But, as I picked the brains of my surgical team—Troy Morrison, CRNA; circulating nurse Luisa Crandell; and surgical technician Shirley Jones—I realized that the best pearl might be something entirely different: demonstrating excellent leadership.
Surgeons are put in positions of leadership and authority, whether we want it or not. I have come to realize and appreciate that I must be cognizant of my behavior and willing to change it to be a better leader. In other words, my behavior has a critical impact on the surgical team, and it can either enhance or undermine the efficiency of the day.
We must be mindful and considerate. Come in early—or at least on time—for surgery. Embody the golden rule and treat others the way you would want to be treated. Be positive, pleasant, patient, encouraging, humble, and enthusiastic, not negative, irritated, impatient, blame-shifting, arrogant, or disengaged.
People want to follow those whom they respect. When you lead by example, the natural outflow from your team will result in more determination and hard work. This is where the synergy between your desires for OR efficiency and the team’s desire to be their very best merge into one. Leading by example is not at all easy, but it is the most valuable way to improve OR efficiency.

CYNTHIA MATOSSIAN, MD, FACS | MATOSSIAN EYE ASSOCIATES, HOPEWELL AND HAMILTON, NEW JERSEY, AND DOYLESTOWN, PENNSYLVANIA
Best Time-Saver in the OR: Plan Ahead
Here are three key ways I save time in the OR:
- Calculate IOL powers and send, fax, or email them to the ambulatory surgery center (ASC) ahead of time. This way, the ASC has time to place the orders without incurring extra overnight delivery charges. Over time, this yields significant monetary savings for the ASC.
- If you are considering the use of any additional devices or products during your cases, communicate this possibility to the ASC in advance: possible Malyugin Ring (MicroSurgical Technology) implantation, possible vitrectomy, possible need for Triesence (triamcinolone acetonide injectable suspension, Alcon), possible need for ReSure Sealant (Ocular Therapeutix), etc. This way, the ASC has adequate time to confirm the availability of these products on your surgery day.
- At the start of the OR day, have a morning huddle with the scrub technician and circulating nurse to review all the cases and to identify any complex cases, need for additional instruments, arrival times of OR visitors, and unusual patient needs such as extra sedation.
Thorough preplanning leads to efficiency and decreases stress in the OR.

ERIK L. MERTENS, MD, FEBOphth | MEDIPOLIS ANTWERP PRIVATE CLINIC, ANTWERP, BELGIUM
Instant Access to Information
To boost efficiency in my clinic, we have implemented an electronic health record and diagnostic interface that provides me with instant access to information in the OR. This is not only helpful for identifying the correct procedure for patients, but it also helps to create a paperless office.
Another innovation that improves OR efficiency is use of the CapsuLaser (Excel-Lens, not FDA approved). This device, attached to the microscope, allows me to create a selective laser capsulotomy without moving the patient from the operating table during surgery.

P. DEE G. STEPHENSON, MD | STEPHENSON EYE ASSOCIATES, VENICE, FLORIDA
Creating Quality Time With Use of Scribes
Having a competent scribe who can serve as a written mirror of my voice has enhanced my practice by enabling me to spend much more quality time with my patients. Now that I am no longer simultaneously listening and entering information, I am able to give each patient my undivided attention and focus solely on the patient before, during, and after the examination. I have time to address patients’ concerns, explain findings, and answer questions in greater detail. I pursued a career in medicine because of the reward it brings by helping others, and now, with more time for each interaction, this satisfaction is magnified. Patients leave the office knowing that they, and not the computer, were my primary concern.
Life is short. I am a surgeon, but I am also a mother, daughter, sister, and aunt. Having a scribe has afforded me much more daily and treasured time with my patients and loved ones, which has been my greatest joy this year!

RICHARD TIPPERMAN, MD | WILLS EYE HOSPITAL, PHILADELPHIA
Predilation for Laser Cataract Surgery Patients
How fast patients reach full pupillary dilation can vary greatly. Patients whose pupils are not adequately dilated for their scheduled cataract surgery can not only delay their own procedure; they can bottleneck the entire surgical schedule—especially in an ASC where more than one surgeon uses the femtosecond laser during the same block time. We avoid this problem by purchasing small bottles of cyclopentolate 1% in bulk and giving them to our cataract surgery patients with instructions to instill one drop on the day of their surgery before they travel to the ASC. We do not charge the patients for these drops, but I feel that the nominal cost is well worth it in terms of maximizing ASC efficiency.

VANCE THOMPSON, MD | VANCE THOMPSON VISION, SIOUX FALLS, SOUTH DAKOTA
Improving Efficiency in Premium Cataract Surgery Through Capsulotomy
I am a believer that the perfect capsulotomy can help to optimize any cataract surgery. I define a perfect capsulotomy as one that is centered as close as possible on the visual axis for the best optical outcome and on the center of the capsule for the best anatomic (and optical) outcome. If the capsulotomy does not fulfill both criteria, the patient has an increased risk of experiencing glare and halos.
When I was doing capsulotomies manually, I used to center them on the pupil. With this approach, I found that I often did not achieve 360º of anterior capsular overlap of the IOL optic in cataract surgery, resulting in capsular fibrosis and contraction. Therefore, I had a higher incidence of lens tilt and decentration than I would have liked.
When I became involved in the research and development of femtosecond laser technology for cataract surgery in 2011, I found that I was able to consistently get a round capsulotomy of the proper size with the laser. However, I was still centering on the pupil, resulting in inconsistent anterior capsular overlap of the optic.
I then began using a femtosecond laser platform that utilized OCT to position the capsulotomy on the center of the lens. This helped improve my anterior capsular overlap rate, but there was still a significant number of cases in which I did not achieve overlap because the patient could not fixate when the device applied suction to hold the eye still. As a result, I still had more instances of not achieving anterior capsular overlap than I would have liked.
The article by Chang and Waring,1 describing the use of the subject-fixated, coaxially sighted corneal light reflex as a clinical marker for centration of refractive treatments, taught me why centering the capsulotomy manually, or with a laser, on the pupil did not give me consistent overlap. It also taught me the importance of patient fixation on the microscope light during capsulotomy. As a result, I went back to performing manual capsulotomies, marking the cornea with an optical zone marker centered on the visual axis to take advantage of the subject-fixated, coaxially sighted light reflex.
However, now that I was back to performing manual capsulotomies, I did not achieve the roundness and consistent size that I enjoyed with the laser. My anterior capsular overlap rate did improve, but it still was not as consistent as I would have liked.
When I incorporated the Zepto capsulotomy system (Mynosys) into my surgical routine, a few things happened that were game changers. First, I realized that I didn’t have to try to follow a corneal mark to do lens surgery. I was now working directly on the lens capsule with a round device of the proper size, and I could create a consistently centered capsulotomy to achieve 360º of anterior capsule overlap of the optic (Figure).
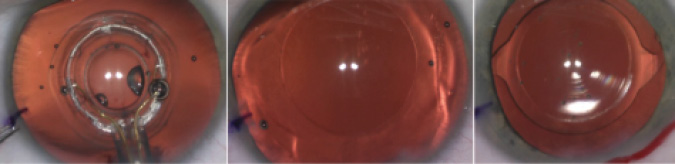
Figure. Zepto capsulotomy improves surgical efficiency, the accuracy of centering the capsulotomy in cataract surgery, and the rate of achieving 360º of capsular overlap to optimize long-term implant stability.
Second, my surgical efficiency improved. With manual capsulotomies, I had to mark the cornea and, while performing the capsulotomy on the lens, continually reposition the eye so that the corneal light reflex was centered as well as possible. With the femtosecond laser, I had to go into a separate room with the patient, which slowed down the process. With Zepto, I can operate directly on the capsule, and it fits right into my surgical routine in the OR.
My rate of anterior capsular overlap of the optic increased with this technology, and use of the Zepto is now a mainstay in my practice. Because it allows me to achieve consistent overlap of the optic, I believe that there is less chance of patients’ experiencing dysphotopsias from tilting and decentration of the optic—problems that can occur when the anterior capsule does not overlap the optic.2
1. Chang DH, Waring GO IV. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol. 2014;158:863-874.
2. Thomson VM. Streamlined method for anchoring cataract surgery and intraocular lens centration on the patient’s visual axis. J Cataract Refract Surg. 2018;44(5):528-533.

GEORGE O. WARING IV, MD | WARING VISION INSTITUTE, MOUNT PLEASANT, SOUTH CAROLINA
Benefits of EHRs
The combination of a scribe and an intelligent, automated, hybrid electronic health record (EHR) has been a game changer for my practice. With the implementation of a hybrid cloud-based EHR, practice management software, and trained scribes, I have more face time with our clients and increased efficiency in the OR and clinic. We utilize Modernizing Medicine’s hybrid electronic health record system, their practice management software, and revenue cycle management.

ROBERT J. WEINSTOCK, MD | THE EYE INSTITUTE OF WEST FLORIDA, LARGO, FLORIDA
OR Efficiencies Include a Traffic Cop
Trying to perform eight to 10 cataract surgeries per hour is no easy task. Very few surgeons or surgery centers are able to meet this benchmark. Speed is not the No. 1 goal, but running a highly efficient and streamlined surgical process does provide benefits to the patients, doctors, surgery center, and practice. It takes a tremendous amount of planning, skill, coordination, teamwork, and execution to achieve, and it often takes years of refinement to truly accomplish.
We use video monitors in every OR to improve efficiency. We have multiple cameras stationed throughout our ASC to see what is happening in different areas and rooms. For example, in one of the ORs, the TV monitor that is mounted in the corner can be split to one, four, or nine different views, depending on our goals. We typically split it into four views: one is a wide view of the femtosecond laser room, and the other three quadrants are wide views of the other ORs and sterile hallway.
In the hallway, we have a monitor split into nine views, where all three ORs, the femtosecond laser room, the preoperative and postoperative holding areas, and the hallway can be seen. This allows everyone to be on the same page and to know exactly what is going on, which helps surgical flow tremendously. The nurses and scrub technicians find this very helpful with regard to the timing of preparation, draping, and speculum insertion.
Another way we improve efficiency in our surgery center is by using a person who serves as a traffic cop. This person dictates the flow and decides where the fellow and the surgeon should go, depending on which patient is prepped and draped, and he or she also coordinates the intraoperative aberrometry measurements that are needed during surgery. The person in this position monitors the video feeds of the whole surgery center and sometimes makes on-the-fly adjustments depending on how long cases are taking in different rooms.
These two processes in our surgery center play a critical role in our efficiency and our ability to deliver the outcomes and experiences that today’s patients expect and deserve.

BLAKE K. WILLIAMSON, MD, MPH, MS | WILLIAMSON EYE CENTER, BATON ROUGE, LOUISIANA
It’s All About Your Staff
For busy refractive surgeons, time is one of the most valuable commodities. There are many things one can do to save time that do not require the surgeon’s attention so that he or she can focus on operating and serving patients. Within the clinic setting, I have found that the biggest time saver of all is having a competent scribe. This teammate navigates the EHR system and ensures all information is entered properly, allowing me to concentrate on the patient and establish a rapport. The scribe also handles all of my patient’s pharmacy needs.
Another time-saver is having your own clinical team who works with only you and not different surgeons on a rotating basis. In this way, my team is acutely aware of all the testing and details I will want for our most common evaluations.
Finally, hiring a surgery scheduler is extremely helpful if you perform a high volume of cases. With this team member, my technicians and scribe do not need to spend time going over paperwork once the consultation is over. We simply leave the room, and the scheduler takes care of the rest.
You need to have a rock star team who believes in you and what you are trying to accomplish and is willing to work hard to reach your practice’s goals. Saving time is paramount when you are managing two ORs on a busy day. My team will prepare and drape our patients so that, when I walk into the room, I walk immediately into my surgical gown and begin operating. I also allow my scrub technician to remove the eyelid speculum at the end of cases so that I can quickly move to the waiting room to speak with patients’ families before starting the next case.
Another huge time-saver has been the implementation of a two-surgeon shooter system for our femtosecond laser program. I have a second surgeon operate the laser in the femtosecond laser suite while I perform manual surgery in one of the ORs. This saves me from having to walk back and forth from the femtosecond laser suite to the OR. While I prefer to speak to each patient’s family members between cases, I like to save all the charts until the end of the day for sign-off. This allows me to get through the day more quickly.
Lastly, I like to call every patient later that evening on their surgery day. Many times, I can answer questions over the phone and reassure patients, which will save chair time at their postoperative visit. Not only does this gain personal time for the surgeon, but patients love it because it shows how much you care.