Cataract surgery is one of the most successful and most frequently performed invasive procedures in contemporary medicine. Because nearly every operation is also a refractive surgical procedure, we not only cure a predominantly age-related disease but also provide the patient with complete or at least partial spectacle independence, depending on the type of IOL chosen for implantation.
But, even a huge success story like modern state-of-the-art cataract surgery has a downside. In many cases, surgeons pave the way toward a second intervention: Nd:YAG laser capsulotomy to treat posterior capsular opacification (PCO). There is no denying that this treatment, although generally considered safe, nevertheless carries the potential for serious complications. Complications can include damage to the IOL, subluxation of the IOL, retinal detachment, and spikes in IOP. After Nd:YAG laser capsulotomy, some patients can also experience floaters.1,2
Even if removal of the PCO is successfully performed without subsequent problems, the period between cataract surgery and this secondary intervention does not contribute to patient satisfaction. Instead of enjoying good visual function, these patients experience visual deterioration, discomfort, and additional examinations that they had not expected.
A DIFFERENT APPROACH TO PCO
When the femtosecond laser was introduced to cataract surgery a decade ago, high-volume users soon learned that this technology provides the possibility for further applications beyond performing capsulotomy and lens fragmentation in uncomplicated cataract cases. Among these promising off-label procedures is the use of the laser in pediatric cataracts.
There is also an intervention that we have termed primary posterior laser capsulotomy (PPLC), which may be a step toward drastically reducing the incidence of PCO.
Manipulating the posterior capsule is probably not among the most popular procedures for many cataract surgeons. Many surgeons are, as Scott and Scott have correctly observed, not confident in their ability to perform a consistently accurate posterior capsulorhexis.3 After all, for many surgeons, the only time they perform this maneuver is in cases in which a posterior capsule complication has occurred.
The femtosecond laser can perform a posterior capsulotomy safely and precisely; however, it requires some inventiveness on the part of the surgeon. That is, we must dupe the software into believing that the posterior capsule is the anterior capsule and perform all necessary measurements.
The splendid imaging systems of these femtosecond laser platforms, such as built-in spectral-domain OCT, have given us new insight into a generally overlooked anatomic feature, Berger space, which is the space between the posterior capsule and the anterior hyaloid. In almost three out of four patients, this void is deeper than 400 µm intraoperatively.
A combination of factors may lead to this intraoperative anatomic feature. Removing the natural lens creates more space. The space is also expanded by fluid that moves through the zonules while the cataract operation is underway. In addition, gravitational forces in a patient lying flat on his or her back are pulling the vitreous toward the posterior pole.
Injecting OVD behind the IOL in the capsular bag provides a safe distance between the posterior capsule and the IOL (Figure, left). Based on our new knowledge of the Berger space, an image-guided, laser-assisted technique makes it possible to perform PPLC at the end of surgery, leaving the anterior hyaloid membrane intact.
HOW IT’S DONE
To perform PPLC, after the cataract surgery procedure is complete, the eye is redocked to the femtosecond laser system—in our case the Catalys Precision Laser System (Johnson & Johnson Vision). This is done just like it is at the beginning of laser cataract surgery. The cylindrical treatment zone for anterior capsulotomy is manually positioned on the posterior capsule, which is placed in the first inferior third of the treatment zone (diameter 3.5 mm, incision depth 600–800 µm, horizontal spot spacing 5 µm, vertical spot spacing 10 µm, pulse energy 8 µJ). Care is taken to avoid positioning the treatment zone within the IOL optic or the anterior hyaloid.
Immediately before the laser treatment, the capsulotomy position is confirmed with live OCT (Figure; middle). Then the PPLC is performed (treatment time about 2.5 seconds). Immediately after treatment, the posterior capsular disc usually starts to contract, which can be seen on the computer screen (Figure; right). There is no need to remove this disc. It curls up, sinks down, disappears, and cannot move into the vitreous because the anterior hyaloid membrane is left intact.4 It does not cause visual disturbances such as floaters and generally does not bother the patient at all.
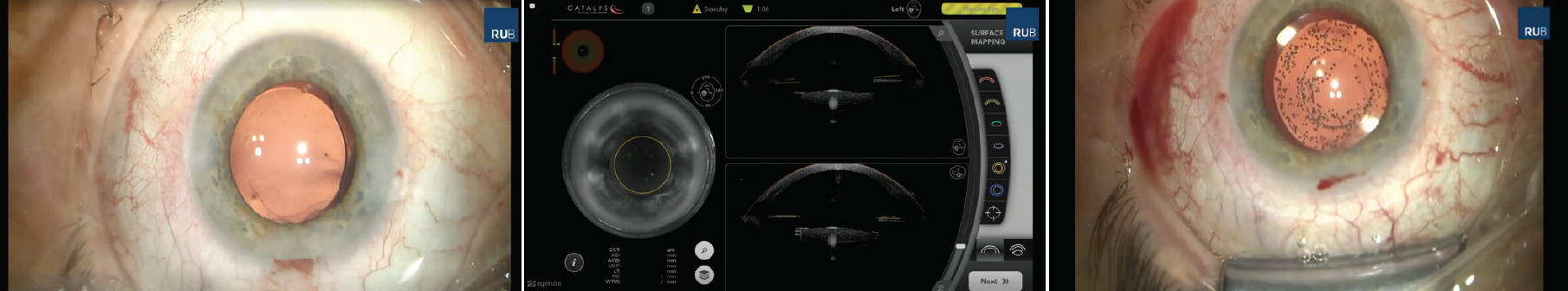
Figure. A small amount of OVD is injected behind the IOL (left). Then, the capsulotomy position is confirmed on the live OCT scan (middle). Following treatment, the posterior capsule contracts and moves out of the optical axis (right).
Next, the eye is undocked, and the patient is moved back under the operating microscope to confirm whether the posterior capsulotomy is well centered and free-floating for 360º. Postoperative management is as usual.
CLINICAL EXPERIENCE
In one of our first prospective intraindividual clinical trials evaluating PPLC, we performed follow-up examinations at 1 week, 2 months, and 6 months postoperative in 28 patients who had received PPLC in one eye and no PPLC in the other eye after routine cataract surgery. Proper IOL centration was achieved in all treated eyes. No damage was seen in the implanted IOLs after PPLC. In the control group, slight and incipient PCO was seen in 11 eyes at 6 months postoperative. In the PPLC group, no PCO was seen.5
Recently, we submitted for publication our 2-year results with this group of patients. There was indeed a significant difference in PCO occurrence between the groups, with no hints of opacification visible in the PPLC eyes, while in the control group all eyes had some degree of PCO.
The PPLC procedure was not only effective but also safe. There were no IOL dislocations, no incidences of elevated IOP, no retinal detachments, no macular edema, and no significant loss of endothelial cell density. No damage to the IOL was caused by the laser in any treated eyes. At the 2-year follow-up, no patients complained of floaters, an indication that the curled-up posterior capsular disc vanishes out of the optical axis.6
CONCLUSION
Our clinical experience gives us a strong sense of the potential of PPLC as a tool to prevent PCO in many patients. By offering a technique that can be performed by all surgeons in a safe way with consistent results, the femtosecond laser may indeed represent the first achievable solution for the prevention of PCO.
Posterior capsulotomy might also facilitate the fixation of toric IOLs, the one type of IOL for which rotation and dislocation can prove visually devastating for the patient.7
But, clinical success is only one factor. The logistics for this indication are currently quite inadequate and must be addressed. Manufacturers of femtosecond lasers have yet to develop software for performing posterior capsulotomy. There are also wide differences among the systems currently on the market when it comes to redocking and the ability to reliably measure the deeper structures of the eye.
More important, the economic situation is unsatisfactory in most countries. It is currently necessary to pay an additional click fee to perform PPLC. Prevention in most health care systems is not rewarded as it should be. On the other hand, Nd:YAG capsulotomy usually is. This is a situation that might be addressed by appeals to health finance authorities in the future.
1. Charles S. Vitreoretinal complications of YAG laser capsulotomy. Ophthalmol Clin North Am. 2001;14:705-710.
2. Awasthi N, Guo S, Wagner BJ. Posterior capsular opacification; a problem reduced but not yet eradicated. Arch Ophthalmol. 2009;127:555-562.
3. Scott W, Scott R. Primary posterior capsulotomy and the femtosecond laser. J Cataract Refract Surg. 2017;43:577-578.
4. Dick HB, Schultz T. Primary posterior laser-assisted capsulotomy. J Refract Surg. 2014;30:128-133.
5. Schojai M, Schultz T, Haeussler-Sinangin Y, et al. Safety of femtosecond laser-assisted primary posterior capsulotomy immediately after cataract surgery. J Cataract Refract Surg. 2017;43:1171-1176.
6. Schojai-Schultz M, Robles A, Schultz T, Dick HB. Primary posterior laser-assisted capsulotomy (PPCL) after cataract surgery: 2-year results. Paper presented at: The European AECOS Symposium; May 31-June 3, 2018; Berlin, Germany.
7. Scott WJ, Owsiak RR. Femtosecond laser-assisted primary posterior capsulotomy for toric intraocular lens fixation and stabilization. J Cataract Refract Surg. 2015;41:1767-1771.