CASE PRESENTATION
A 12-year-old boy was referred to us for progressively worsening vision and suspected keratoconus in his right eye. The patient was not wearing glasses or contact lenses to correct his visual acuity. He had no significant ocular surgical or medical history. His father stated that the patient rubbed his eyes aggressively at night.
On presentation, the patient’s uncorrected distance visual acuity (UDVA) was 20/50 OD and 20/20 OS. With a manifest refraction of +0.75 -3.75 x 015º OD, his best corrected distance visual acuity (CDVA) was 20/40, and with a manifest refraction of +0.25 -0.75 x 160º OS, his CDVA was 20/20. Anterior and posterior segment examinations were unremarkable.
At the patient’s first visit, the thinnest pachymetry reading was 514 µm OD, with a maximum keratometry (K) reading of 51.20 D OD. Imaging with the Pentacam (Oculus Optikgeräte) demonstrated an inferior cone and steepening, confirming the diagnosis of keratoconus (Figures 1 and 2). Measurements using the Atlas Corneal Topography System (Carl Zeiss Meditec) showed a steep K of 45.44 D @ 104º and a flat K of 41.27 D.
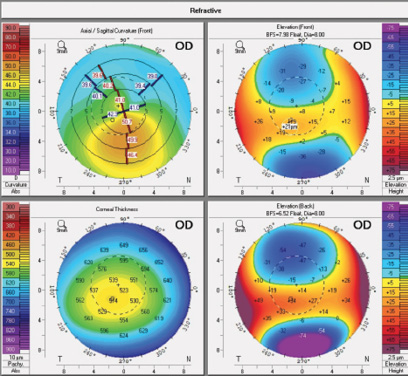
Figure 1. At the patient’s initial visit, imaging of his right eye with the Pentacam demonstrated significant astigmatism, a steep maximum K reading, and inferior steepening.
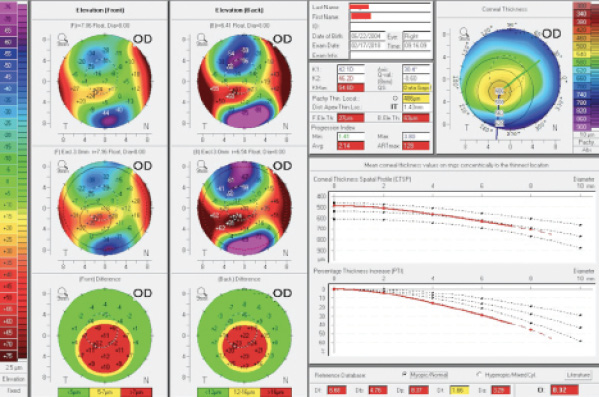
Figure 2. The Pentacam’s Belin/Ambrósio Enhanced Ectasia Display showed keratoconus during the patient’s initial visit.
The patient’s left eye appeared to be without significant pathology. A diagnosis of keratoconus was made for his right eye, and the patient underwent conductive keratoplasty (CK) on his right eye, followed 1 day later by epithelium-on (epi-on) CXL. The CK procedure is noted in Figure 3. The epi-on CXL treatment was performed as part of the CXL USA clinical trial, with that company’s proprietary riboflavin formulation. Light energy of 4 mW/cm2 was cycled on and off at 15-second intervals for 20 minutes.
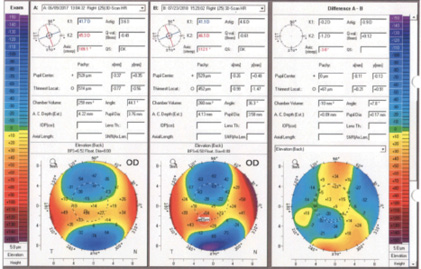
Figure 3. Pentacam corneal densitometry images before (left) and after (right) CXL. Four CK spots were placed inferiorly, corresponding to the relatively elevated inferior cone shown on the preoperative Pentacam elevation map in Figure 1.
We monitored the patient closely during the first 6 postoperative months. The result appeared to be stable, and he maintained a UDVA of 20/25 OD. Pachymetry revealed thinning, but we did not believe it indicated keratoconic progression. One year after surgery, UDVA remained 20/25 OD, not improved with refraction, but Pentacam imaging revealed significant corneal changes. The thinnest pachymetry reading had decreased from 486 µm preoperatively to 452 µm (Figure 4). Change in curvature is noted in Figure 5. Despite the use of bepotastine besilate ophthalmic solution 1.5% (Bepreve, Bausch + Lomb) and artificial tears, the patient had continued rubbing his eyes at night, according to his father.
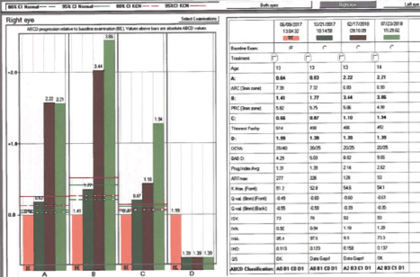
Figure 4. Pentacam comparison (right) of elevation (back) preoperatively (left) and 1 year after surgery (middle). The thinnest pachymetry reading clearly showed more progression than expected after CXL, and astigmatism continued to increase over 1 year.
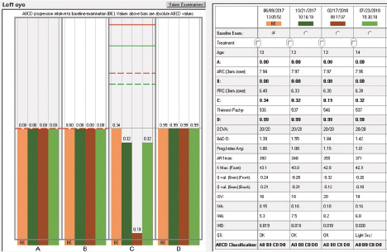
Figure 5. Comparison (right) of axial curvature (front) preoperatively (middle) and 1 year after CXL (left).
Review of the Pentacam’s Belin ABCD Keratoconus Staging Display prompted us to contemplate repeat CXL (Figures 6 and 7). We thought that progression since CXL was clearly evident for all parameters except criterion D (CDVA). Our discussion centered on whether or not to repeat CXL with the epithelium on or off.
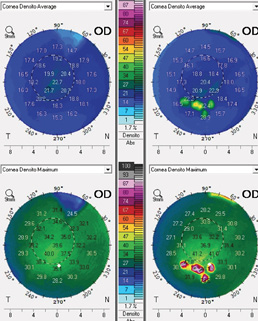
Figure 6. The Pentacam’s Belin ABCD Keratoconus Staging Display for the patient’s right eye clearly indicated significant progression in three of four indices 6 months after initial CXL, with continued progression of two of four indices 1 year after surgery.
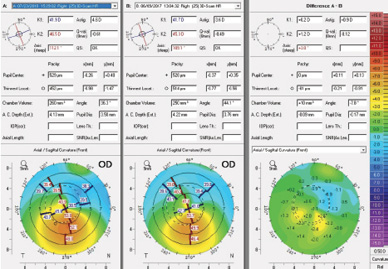
Figure 7. The Belin ABCD Keratoconus Staging Display for the patient’s left eye was normal.
Does one method of CXL have greater efficacy for repeat treatment? Is one method associated with a higher risk of complications? Would you intervene or continue observation in this case?
—Case prepared by Hercules Logothetis, MD; and William F. Wiley, MD

FLORIAN T.A. KRETZ, MD, FEBO
This is a complicated situation. On the one hand, the child is quite young, and his age alone could be responsible for the rapid ectatic progression. Also uncertain is the actual epithelial thickness of the cornea. Maybe the stroma had already thinned significantly more than expected, and the preoperative epithelium was thicker than usual. Considering that all examinations were performed with the epithelium on, perhaps epithelial mapping would have been helpful. Change of posterior elevation shows alteration over the course of 1 year, and progression is evident on the Belin ABCD Keratoconus Staging Display, too.
Debate continues about epi-on versus epithelium-off (epi-off) CXL. At the clinics where I practice, my colleagues and I still mainly use an epi-off approach because we think it improves riboflavin’s penetration of the stroma. In addition, energy absorbance happens in the treatment area, whereas the epithelium might otherwise absorb a significant amount of energy.
A 13-year-old child will be very unhappy about the pain induced by an epi-off procedure, but this form of treatment might help to stabilize his condition. Because keratoconic progression was quite significant on the ABCD analysis, I would recommend an epi-off retreatment. If the patient and his family preferred continued monitoring to intervention, I would recommend comparing corneal thickness and epithelial mapping.

AARON WAITE, MD
The patient’s age and history of rubbing his eyes put him at high risk of ectatic disease progression. Treatment with CXL was appropriate. He was also treated with CK, which can help normalize irregular astigmatism caused by keratoconus. Although CK has not been studied in pediatric patients, it has been reported to be effective as an adjunctive treatment of keratoconus in adults.1,2
The Belin ABCD Keratoconus Staging Display, a method of monitoring disease progression, shows progression in the anterior and posterior radii of curvature and progressive thinning of the cornea over 13 months. At the most recent visit, three of the four parameters measured were beyond the 95% confidence interval for progressive keratoconus. In addition, K readings measured by the same instrument increased compared to preoperative levels. Other than visual acuity, all measured parameters showed progressive keratoconus. Fortunately, the patient’s visual acuity improved with treatment and has remained stable.
Considering the patient’s age, I think early intervention is better. Because keratoconus has progressed, I recommend repeat CXL. This patient’s other eye should be monitored closely for changes indicative of keratoconus, even though it currently appears normal. A low threshold for offering CXL at the earliest sign of keratoconus is warranted.


WHAT WE DID: HERCULES LOGOTHETIS, MD; AND WILLIAM F. WILEY, MD
The Pentacam’s Belin/Ambrósio Enhanced Ectasia Display uses a best-fit sphere taken from the central 8-mm zone and creates a reference surface. The software generates a best-fit sphere from a pathologic cornea and creates a false “normal” best-fit sphere to compare with the abnormal cone of the ectatic region of the cornea. The Belin ABCD Keratoconus Staging Display is a more recent alternative for monitoring ectatic disease progression. Criterion A describes the average anterior radius of curvature in the 3-mm zone centered on the thinnest location of the cornea. Criterion B describes the average posterior radius of curvature in that same 3-mm zone. Criterion C describes the thinnest pachymetry reading in microns. Criterion D is the CDVA. On this display, the checkered green lines and the solid green lines indicate the 80% and 95% confidence intervals, respectively, of healthy eyes, and the checkered and solid orange lines indicate the 80% and 95% confidence intervals, respectively, of keratoconic eyes.3
Our review of the Belin ABCD Keratoconus Staging Display in this case prompted us to repeat epi-on CXL in November 2018. The procedure was performed with CXL USA’s proprietary riboflavin formulation. Light energy of 4 mW/cm2 was cycled on and off at 15-second intervals for 30 minutes.
On postoperative day 1, the patient’s UDVA was 20/25, and he reported no pain. He was to continue his care in another state 2 weeks later. He will be monitored thereafter with quarterly Pentacam imaging, using the Belin ABCD Keratoconus Staging Display to look for ectatic disease progression.
Editor’s note: This article discusses off-label techniques such as epi-on CXL and the use of CK for the treatment of keratoconus.
1. Kato N, Toda I, Kawakita T, et al. Topography-guided conductive keratoplasty: treatment for advanced keratoconus. Am J Ophthalmol. 2010;150(4):481-489.e1.
2. Alió JL, Claramonte PJ, Cáliz A, Ramzy MI. Corneal modeling of keratoconus by conductive keratoplasty. J Cataract Refract Surg. 2005;31(1):190-197.
3. Belin MW, Meyer JJ, Duncan JK, et al. Assessing the progression of keratoconus and cross-linking efficacy: the Belin ABCD Progression Display. Int J Kerat Ect Cor Dis. 2017;6(1):1-10.




