Scott M. MacRae, MD, spoke with CRST about his pioneering work on laser-induced refractive index change (LIRIC), which can noninvasively alter the refractive properties of the human cornea. His research has the potential to revolutionize refractive surgery.
CRST: What is LIRIC? What technology is used to perform it?
Dr. MacRae: Clerio Vision’s LIRIC is a minimally invasive method to correct the eye’s aberrations with a laser. This is a [potential] paradigm shift in how we correct the eye’s refractive error. With all previous refractive surgery techniques, a laser such as an excimer or femtosecond is used to cut and ablate tissue. What we’re doing is different; with LIRIC, a femtosecond laser is used at low energy levels, below the ablation threshold.
LIRIC is performed at a wavelength of 405 nm, which is at the blue end of the visible spectrum. At this wavelength, LIRIC is a 2-photon absorption process, resulting in highly localized refractive index changes. Within the laser focus volume (approximately 5–10 µm in diameter and length), instead of removing or disrupting tissue, we are altering collagen fibril density.1-3 LIRIC is relatively noninvasive in that we are using pulse energies that are 1/100th to 1/1,000th those used to create a femtosecond laser flap. During LIRIC, the laser alters the refractive index in a highly localized fashion—akin to using a fine-point pen.
CRST: What need is this procedure designed to meet?
Dr. MacRae: We are in the early days, and there is still a lot of work ahead of us. If LIRIC delivers on its potential, however, it will be a game changer because it is relatively noninvasive and because it could be used as first-line therapy to treat myopia, hyperopia, astigmatism, and higher-order aberrations. In addition to addressing the problem of patients’ fear of surgery, LIRIC expands the number of treatable patients. For example, thin corneas could be treated without the risk of inducing ectasia because the procedure does not remove any tissue. Moreover, presbyopic correction could be performed in the cornea by creating a multifocal pattern in the tissue based on diffractive designs similar to those successfully employed in multifocal IOLs.
CRST: Who would be a candidate for LIRIC?
Dr. MacRae: The inclusion criteria are quite broad because the procedure is so minimally invasive. Interestingly, the first LIRIC patients were older pseudophakes who had received monofocal IOLs. They recovered quickly without complications. A diffractive multifocal pattern was imparted to their corneas with LIRIC, thereby increasing their depth of focus (Figure 1).
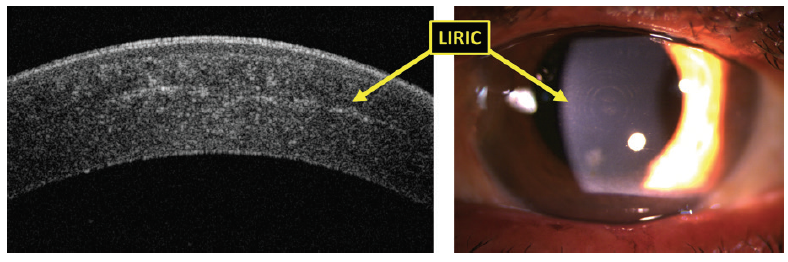
Figure 1. OCT (left) and slit-lamp (right) images of eyes with a diffractive multifocal pattern imparted by LIRIC for presbyopic correction.
CRST: What are the study results so far?
Dr. MacRae: Late in 2018, we completed our first application of LIRIC to live humans (N = 27). The results so far indicate that the multifocal LIRIC procedure for presbyopic correction imparted an approximately 1.5-line benefit to distance-corrected near visual acuity without any degradation of distance vision. Corneal thickness and curvature were unaffected. Endothelial cell density was also unaffected, suggesting a good safety profile.
We recently presented some of our results at a few conferences, including the 2019 Winter Symposium of the American-European Congress of Ophthalmic Surgery,4 and we will be making additional presentations at the 2019 ASCRS and ARVO meetings. We have not yet published human data (Figure 2).
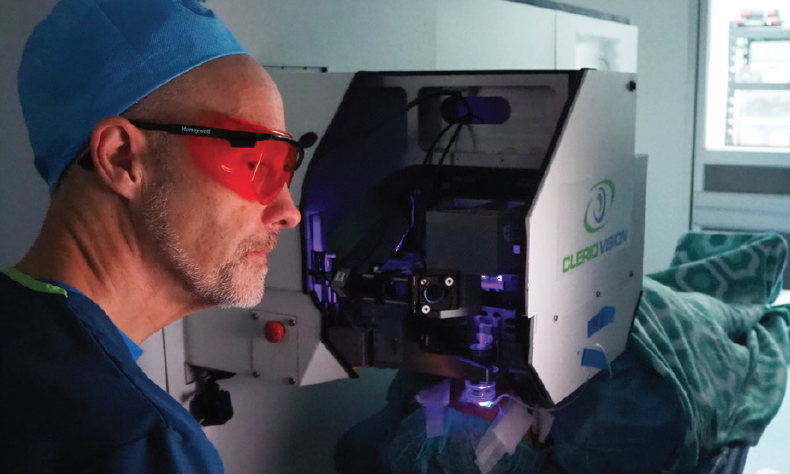
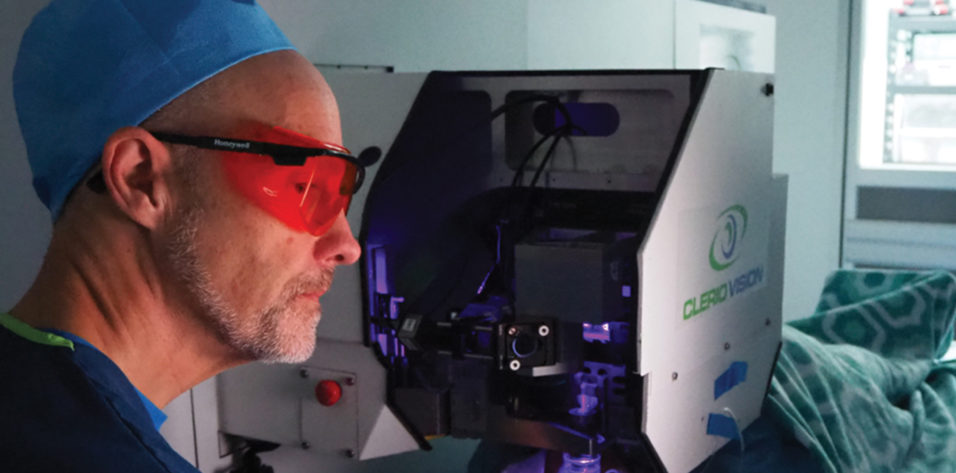
Figure 2. Dr. MacRae performing the first-in-human LIRIC procedure.
CRST: How long does the procedure take?
Dr. MacRae: Treatment time for our first-in-human presbyopia treatment was approximately 1 minute. We anticipate that treatment time will decrease to well below that as the technology matures.
CRST: Is there a healing response? What postoperative management is needed?
Dr. MacRae: In our clinical and preclinical work to date, we have not seen any induced inflammation or wound-healing response. Posttreatment corneas were clear, and they [exhibited] no light scatter or signs of inflammation. Histologic studies have shown that LIRIC results in significantly less cell death than cutting a flap with a femtosecond laser.1
Our early clinical observations in humans indicate that corneas are quiet and clear right after the treatment and at 1 day, 1 week, and 1 month after treatment.
CRST: Is the procedure permanent? Is it reversible?
Dr. MacRae: Our preclinical models have shown stability out to over 2 years. Because the LIRIC pattern occupies a very thin cross section of the cornea, repeat treatments are possible at a different depth. The LIRIC treatment consists of a modified layer of stroma that is approximately 10 µm thick, which corresponds to only a small percentage of the entire cornea. We have not done reversibility studies, but we believe that the procedure is reversible.
CRST: What challenges have been identified with LIRIC that must be addressed?
Dr. MacRae: The technology is still young. We’ve only just completed the first procedures in humans. We are closely tracking these patients. Although this study consisted of a multifocal treatment with 2.50 D add power, the limit to how many diopters can be imparted is yet to be seen. Contact lenses have been written up to about 10.00 D of single-vision spherical correction.
CRST: How might this procedure fit with currently available options and with other adjustable options like RxSight’s Light Adjustable Lens (RxLAL) or the Perfect Lens laser system (not FDA approved)?
Dr. MacRae: The RxLAL is an exciting technology that increases cataract surgeons’ flexibility, but it requires having the patient avoid UV light exposure and can require repeat treatment. Moreover, the procedure is limited to a specific IOL, and the range is limited. Perfect Lens is working on modifying IOLs, and the company has reported some positive results. (For more information on the Perfect Lens, see Different Approaches to the Same Problem.)
Different Approaches to the Same Problem
By Nick Mamalis, MD
The Perfect Lens system and Clerio Vision’s laser-induced refractive index change (LIRIC) of the cornea (neither FDA approved) offer two different ways of solving the same problem: refractive error after cataract surgery. No matter how good ophthalmologists are at performing preoperative measurements and IOL power calculations and how skillfully they operate and use lens implants, there are still patients who experience refractive surprises after cataract surgery. The ability to correct refractive error after cataract surgery without having to reenter the eye would represent a major advance in these patients’ care.
What is interesting is that, instead of acting on the entire curvature of a surface (IOL or cornea), refractive indexing works much like a Fresnel prism. A small change in the lens material or corneal tissue can yield a much larger change in refraction. For example, my colleagues and I working with the Perfect Lens system found that a refractive index change of 0.01 could provide 3.30 D of actual change.
COMPARING TECHNOLOGIES
Similarities and differences. Both the Perfect Lens technology and LIRIC use a femtosecond laser at a low level of energy to produce a change in refractive index. With the former, laser energy is used to cause photoinduced hydrolysis of the polymetric material of the IOL. The heat causes what is called a phase separation, which produces an increase in the hydrophilicity of the lens material and causes the refractive index to change in this area. The major difference between LIRIC and the Perfect Lens system, not to mention RxSight’s Light Adjustable Lens (RxLAL), is that Scott M. MacRae, MD, and his fellow investigators are using LIRIC on the cornea. The procedure focally alters corneal collagen fibers, which produces local changes in the refractive index.
Advantages. An advantage of the Perfect Lens system and LIRIC is that both may be used on any pseudophakic eyes, whereas RxSight’s technology can be used with only the RxLAL. A further advantage of LIRIC is that IOL material does not matter, whereas the Perfect Lens system is designed for use on only hydrophobic and hydrophilic acrylic lenses—although it should be noted that these are the most common IOL materials worldwide.
Both the Perfect Lens technology and LIRIC have the potential not just to change spherical correction but to add multifocality. This could be a major benefit for patients who are deeply dissatisfied with their lack of near vision after cataract surgery. A possible advantage of the Perfect Lens system, however, lies in the reverse. If a patient who received multifocal IOLs has intractable dysphotopsia, the technology could potentially be used to imbue a laser pattern on the lens to neutralize the multifocality, thereby avoiding the need for an IOL exchange.
CONCLUSION
Refractive indexing technology is promising. With any new technique, however, the most important issue is safety. Results from our rabbit studies using the Perfect Lens system have found no signs of ocular inflammation or corneal toxicity. Similarly, Dr. MacRae reports no evidence of corneal toxicity with LIRIC.
Safety will continue to be an area of focus with both technologies. Because LIRIC is performed on living tissue, investigators will have to monitor patients over time for refractive changes from aging or remodeling of the cornea.
LIRIC can be performed on IOLs, corneas, or contact lenses. Of these, the work on human corneas is the most exciting in my opinion. The corneal procedure promises freedom from spectacles or contact lenses. Moreover, the technology may have a much wider population of potential patients than the RxLAL or Perfect Lens system because it could treat myopia, hyperopia, astigmatism, and higher-order aberrations in pseudophakes and in nonpseudophakes. In addition, LIRIC can treat a wide variety of refractive errors without relying on a particular IOL polymer or on pupillary dilation. Again, LIRIC can be modified or repeated on multiple occasions because it changes the cornea only in a stromal layer that is 10 µm thick.
That said, LIRIC can also modify an IOL’s refractive error as a touch-up correction, which could give the surgeon more flexibility in treating postoperative refractive surprises.
CRST: How could LIRIC change the surgical experience for patients and for doctors?
Dr. MacRae: The relatively noninvasive approach could be very appealing to both patients and physicians. There is no need for antibiotics or steroid drops because no incisions are made and the epithelium is undisturbed. Based on our animal studies, LIRIC has almost no effect on corneal nerves, making it much less likely to cause dry eye, which has been a concern with LASIK, small-incision lenticule extraction, and PRK.5
CRST: What are the next steps?
Dr. MacRae: In terms of clinical development, we are targeting European approval for 2022/2023, followed by US approval. We are currently focusing on upgrading the LIRIC platform to allow a broader therapeutic range as well as additional reductions in treatment time.
CRST: What future directions do you envision?
Dr. MacRae: Our goal is to develop the LIRIC technology into a first-line therapy covering all refractive corrections. This entails depositing diffractive optics into the cornea and developing other noninvasive strategies for simpler refractive corrections. If we are successful, we believe that this research will usher in a new era in ophthalmology that will allow a much larger segment of the patient population to choose noninvasive refractive surgery as their primary form of vision correction.
1. Wozniak KT, Elkins N, Brooks DR, et al. Contrasting cellular damage after Blue-IRIS and Femto-LASIK in cat cornea. Exp Eye Res. 2017;165:20-28.
2. Yu D, Brown EB, Huxlin KR, Knox WH. Tissue effects of intra-tissue refractive index shaping (IRIS): insights from two-photon autofluorescence and second harmonic generation microscopy. Biomed Opt Express. 2019;10(2):855-867.
3. Ding L, Knox WH, Bühren J, et al. Intratissue refractive index shaping (IRIS) of the cornea and lens using a low-pulse-energy femtosecond laser oscillator. Invest Ophthalmol Vis Sci. 2008;49(12):5332-5339.
4. Vukich J. Update on indexing? First in man. Paper presented at: American-European Congress of Ophthalmic Surgery Winter Symposium; February 26, 2019; Aspen, Colorado.
5. Wozniak KT, Butler SC, DeMagistris, et al. Short- and long-term impact of laser-induced refractive index change (LIRIC) on corneal nerve distribution in rabbits. Poster presented at: ARVO Annual Meeting; May 1, 2019; Vancouver, British Columbia, Canada.