
As we all know, a typical cataract is not simply a lens that is losing clarity; it is a lens also losing its second major function, which is reading range. Patients love learning what their lens functions once were when their lenses were functioning well. And they feel it is important to know now that, because they have lost those two functions, they have a choice to replace one or both of them during cataract surgery.
When a surgeon delivers high-quality presbyopia- and clarity-correcting cataract surgery and understands its nuances, that surgeon’s practice is recognized by patients and referring doctors as one that cares about keeping up with advances. The practice is seen as serving the needs of all patients, including those who are comfortable wearing glasses after cataract surgery and those who want to enjoy life without glasses.
REFRACTIVE VERSUS TRADITIONAL CATARACT SURGERY
For this article, I will define refractive cataract surgery as a presbyopia- and clarity-correcting implant procedure with the goal of letting the patient do a lot without glasses. By contrast, traditional cataract surgery refers to a procedure in which the implant corrects clarity only and the patient is fine with wearing glasses postoperatively. In my practice, 40% of patients choose the presbyopia- and clarity-correcting refractive cataract surgery journey, and 60% choose the clarity-correcting-only traditional cataract surgery journey.
Patients who choose the refractive cataract surgery journey need to understand that it can be a multistep journey that takes more time than they may have contemplated. Patients do not love hearing this, but they appreciate it, and they handle it far better than those who learn this after surgery, when their fancy implants are not giving them the vision they were hoping for. Setting proper expectations is vital in an advanced cataract surgery practice, and it greatly improves patients’ satisfaction during and after their refractive cataract surgery journey.
REFRACTIVE CATARACT PATIENT EDUCATION
It is important to take ample time for patient education for the benefit of patients interested in refractive cataract surgery. In our practice, patients have a website to learn from, mailed materials to read through, our staff helping to educate them, an optometrist seeing them and educating them in our office, and then finally I continue the process. All cataract patients deserve to know all of the options for postoperative vision. Their choices will determine the way they can use their vision for the rest of their lives.
Educating and presenting the options in simple and understandable terms, setting up preoperative expectations with care and precision, reading patients’ levels of understanding to cater to the way they learn, answering their questions in a patient and caring way, and then delivering the vision they desire has helped our total practice grow in many ways. Patients value a practice that cares deeply about educating them in a comprehensive manner.
All along the patient education process, I am thinking: “What type of cataract surgery would this patient want if he or she knew what I know?” It is our responsibility to get to know the patients and their life activities in order to give a recommendation of what we would do if it were our eyes in their situation. This means we need to get to know their situations.
THE INACCURACY OF CATARACT SURGERY AND THE ACCURACY OF FINE-TUNING
There are many reasons that cataract surgery is not as accurate as we would like. Factors include incisional healing that changes astigmatism, posterior corneal astigmatism that is difficult to precisely quantify in preoperative biometric measurements, and the difficulty of estimating final effective lens position. Each of these limits our ability to hit plano, or whatever the refractive goal is.
After patient education is complete, my patients understand that the lens implant calculation is both a calculation and an estimation—and they know why. They may forget the details, but when I remind them during the postoperative period, it helps a lot that we talked about it beforehand.
It also helps for patients to understand that all cataract surgery typically needs fine-tuning. If they choose traditional cataract surgery, the fine-tuner is glasses. If they choose refractive cataract surgery, the fine-tuner is either corneal laser surgery or a light-adjustable implant.
It also helps for patients to understand why fine-tuning is so accurate. They learn during patient education in my practice about the factors I mentioned previously: incisional healing changing astigmatism, posterior corneal astigmatism that is difficult to precisely quantify, and the final effective lens position. Once healing is complete, I explain that these factors are no longer an issue, and, because of this, fine-tuning will be much more accurate than the initial cataract removal and implant surgery.
I tell all patients, whether I plan to use a corneal adjustment (laser) or an implant adjustment (light), that they should expect to need a fine-tuning. Then, if they don’t need it, they consider it a pleasant surprise.
SOMETIMES 20/20 IS NOT ENOUGH
Because fine-tuning is so important to achieve maximum patient satisfaction, this is a good time to say that sometimes the most confusing part of refractive cataract surgery is the surgeon’s reliance on the Snellen chart. Let me explain.
Just because the patient can see the 20/20 line does not mean that he or she should be happy. As a matter of fact, it is not a good idea for us to think, or say, that the patient should be happy until we have completed our testing. The best thing to do is to perform a high-quality manifest refraction. Even if only a small level of correction is needed, if it makes the patient see crisply, there is a very good chance it will help take the football in for a touchdown.
This is why I love the phrases best corrected image quality (BCIQ) instead of BCVA and uncorrected image quality (UCIQ) instead of UCVA. If a low correction improves that patient’s UCIQ, it is a good idea to do that enhancement. UCIQ is the main driver of patient satisfaction in refractive cataract surgery (Figure).
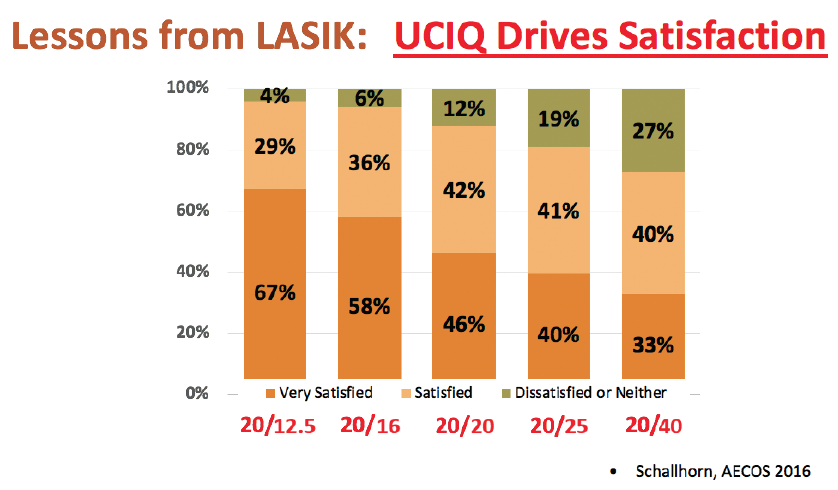
Figure. Uncorrected image quality (UCIQ) is the main driver of patient satisfaction in any refractive surgery procedure, including refractive cataract surgery.
A LOT OF INFORMATION, SO KEEP IN TOUCH
Patience is the name of the game when dealing with refractive cataract surgery patients. You can do a great job of communicating the journey and repeating it multiple times, but they may still need reassurance and a review of the journey. This is why, at 1-month postoperative, we call all of our refractive cataract surgery patients who are being comanaged and not seen by us.
During that call, we can see how they are doing, reassure them, remind them of the three-step plus 1-year journey (which I address later in this article), and answer any of their questions. This has been helpful for our patients’ joy. We also see all refractive cataract patients, including those who are comanaged, at 3 months postoperative to see if they need a fine-tuning, tear-film optimization, or attention to the posterior capsule.
A MULTIPLE-STEP JOURNEY
For all the reasons I have described, and more, refractive cataract surgery can be a multiple-step process that takes more than 1 year to complete for optimal vision. Yes, sometimes it happens fast, just like with traditional cataract surgery, but I want patients to consider it a pleasant surprise when that happens.
I tell all my patients that it is important to be patient in this process, and, if they cannot be because of their personality, lifestyle, or occupation, then they should do traditional cataract surgery, get their new glasses 4 weeks later, and be done. Telling a patient that he or she may not have the personality for a presbyopia-correcting implant can be delicate, but it is far easier than taking care of a patient who is unhappy with his or her vision.
If I suspect that someone is impatient or has a perfectionist tendency, that is the time to delve deeper and ask him or her questions that will help me understand his or her personality well. I am open with the patient; I explain that we cannot change who we are, and I respect that those perfectionist tendencies can lead to success in other areas in life (a compliment helps). However, these personality traits make for a challenging patient in refractive cataract surgery because the final result usually does not happen fast. These patients appreciate this straightforward approach, and they may even still choose to have refractive cataract surgery—but now their expectations are more appropriate.
THREE TAKE-HOME MESSAGES
Here are three pillars that have helped me tremendously in educating patients and selecting appropriate patients for refractive cataract surgery. Making sure that patients understand these three educational pillars has been a game-changer in our cataract program.
Pillar No. 1: How do you want to use your vision for the rest of your life? Do you want to do a lot with glasses after cataract surgery or a lot without them? This is the most impactful question I ask during a cataract evaluation, as I try to figure out which road to go down with the patient in front of me. This one question separates patients into two groups, and patients in both groups appreciate that they are given a choice.
Patients who do not mind wearing glasses can sometimes be confused by all the options and wonder whether they are making a mistake by not having a premium implant. I tell these patients: “The single-vision implant, what we call monofocal, that I use has some of the world’s most advanced optics for image quality, and you are going to love it as long as you don’t mind wearing glasses.” And you can see a sense of peace come over them.
Pillar No. 2: The human lens serves two functions, and one or both can be replaced in this surgery. After figuring out whether the patient minds wearing glasses, I like to make sure they understand that our lens has two functions—reading range and clarity—and that it eventually loses the ability to perform both of those functions. I explain that some implants replace clarity only and some replace both the reading range and the clarity they have lost.
Pillar No. 3: Three steps plus 1 year. This may be the most impactful patient education piece that I deliver in refractive cataract surgery. For those who choose the advanced implant journey, I tell them that this is not a choice for impatient people. I tell them that, over a 4- to 6-month period, they will go through three steps:
Step No. 1: They will get the fancy implant that helps restore clarity and reading range.
Step No. 2: Incisional healing can increase or decrease astigmatism, and effective lens position variability can cause a healing blur that we will need to fine-tune with the laser at 3 months.
Step No. 3: They may also need an Nd:YAG laser capsulotomy within the first few months.
But I then go on to tell them that, after the one to three steps needed to get them to 20/20 vision without glasses, there is 1 year of neural adaptation, as their brain adapts to their new optical system.
CONCLUSION
Becoming comfortable delivering refractive cataract surgery has a lot to do with communication. Your patient must communicate what he or she truly wants, and you and your staff must communicate to set the appropriate expectations for refractive cataract surgery preoperatively, to manage irregularities in patient healing or expectations, and to handle the unhappy patient. Once the surgeon masters an understanding and comfort level in communicating the refractive cataract surgery journey, he or she will see patient and staff satisfaction levels that make delivering advanced cataract surgery a true joy.




