Case Presentation
A 68-year-old woman chose a legal-to-drive vision option, with laser cataract surgery performed on her right eye on September 22, 2016. In March 2000, the patient had undergone bilateral myopic LASIK in which the surgeon had used a microkeratome to create the flaps.
A Haigis L IOL power calculation formula was used for postmyopic LASIK, and the ORA System (Alcon) was consulted intraoperatively. During cataract surgery, the posterior capsule tore, but an anterior vitrectomy was not required. The surgeon implanted a three-piece LI61AO posterior chamber lens (Bausch + Lomb) via an optic capture technique.
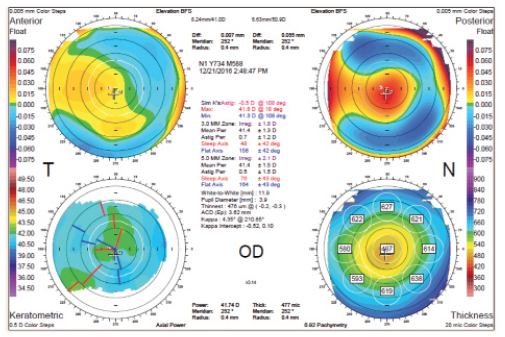
Three months postoperatively, the patient is unhappy with her result. She has a distance UCVA of 20/80 but refracts to 20/20 with a correction of -2.00 +1.00 × 30. Corneal topography is normal (Figure), as is an optical coherence tomography scan of the macula.
The patient will not undergo cataract surgery on her left eye until the issue with her right eye is resolved. How would you approach an enhancement?
—Case prepared by Karl G. Stonecipher, MD.

WILLIAM F. WILEY, MD
My preference would be to perform low myopic PRK with intraoperative mitomycin C (MMC). I find that the technique works well in patients with low myopic errors, and I would favor this approach over another intraoperative maneuver after a complex cataract surgery. Radial keratotomy (RK) is another option, but few surgeons are trained for this procedure.
If this patient had postoperative hyperopia or hyperopia with astigmatism, I might recommend a lens-based approach (IOL exchange or piggyback IOL) instead. In my hands, the results of laser surface ablation for hyperopic correction are variable, and the epithelial healing response often trumps predictability/accuracy. The one exception when I comfortably perform hyperopic surface ablation is for a post-RK patient with early or nonexistent presbyopia. Because the last RK procedures were performed more than 20 years ago in this country, however, these patients are becoming less common, and IOL approaches seem to be the best course of action for their refractive errors.

DENISE M. VISCO, MD
I would perform laser surface ablation. With this level of residual refractive error, the treatment would only remove approximately 24 µm of tissue. The full treatment would be within the flap itself. I am not a fan of piggyback lenses in patients like this one, and I would be concerned about refractive IOL stability. In addition, it would be necessary to treat the cornea with an astigmatic intervention such as astigmatic keratotomy with a femtosecond laser or a blade. In my hands, these procedures are less predictable in eyes with thin corneas compared with a myopic astigmatic excimer laser treatment.
It would be essential to treat the patient’s ocular surface disease prior to diagnostic testing and surgery.

CATHLEEN M. McCABE, MD
I would not object to a piggyback lens in this case. My preference, however, would be to perform PRK over the LASIK flap after confirming its thickness, and I would use MMC. I believe PRK would be the easier and safer option here.
Because this 68-year-old woman has a history of LASIK, I would definitely recommend an ocular surface workup. After optimizing the ocular surface, I would recheck the refraction and then proceed with surface laser vision correction.

QUENTIN ALLEN, MD
The patient’s residual refractive error might allow crisp near UCVA. I would discuss with her the potential of relying on her first eye for near vision and use a near card to demonstrate. The diopter of residual astigmatism may induce enough blur to be visually significant, however, and thus may not be tolerable. If the patient is willing to consider using her right eye for near vision, and the acuity is satisfactory for most near tasks, I would proceed with a distance target for the second eye using a femtosecond laser and the ORA System for verification. This procedure might be curative and provide significant spectacle independence.
If the patient is unhappy with the quality of her near vision because of residual astigmatism but is not opposed to using her right eye for a monovision near approach, an enhancement using limbal relaxing incisions may be possible. A contact lens trial with a toric lens could simulate either a full distance correction or improved near vision with astigmatic correction alone. In my experience, however, corneal arcuate incisions can be less predictable after LASIK.
If the patient insists on correcting the myopic overshoot prior to cataract surgery on her second eye, I would recommend surface ablation with MMC over the prior LASIK flap. I would try to convince her to wait several months (in hopes of performing surgery on her second eye for distance in the meantime) to allow for possible monovision adaptation and to ensure corneal stability prior to any laser vision correction. Based on the Orbscan measurements, her topography is appropriate for this intervention, and her pachymetry appears to be within the limits of this treatment.

DAVID A. GOLDMAN, MD
My choice in this case would be surface PRK with MMC. Before proceeding, however, I would perform a contact lens trial to show the patient what will happen postoperatively to her near vision. The last thing I would want in this case is for her to be unhappy after laser vision correction because she had lost her near vision.