The congenital iris coloboma can be quite challenging to manage. To begin with, there may be an associated lens or zonular coloboma, which may permit vitreous prolapse and may require the use of a capsular tension ring for IOL centration. Even if the IOL is well centered, its edge may still be visible in an abnormal pupil, resulting in positive dysphotopsias or double vision. Simply closing the peripheral portion of the coloboma will not produce an acceptable outcome; when the pupil constricts, it will decenter towards the coloboma at the iris base, so the IOL’s edge will still cause unwanted symptoms. The etiology of this troubling problem is the anatomic anomaly. The iris sphincter tissue is connected to the iris base and chamber angle in the colobomatous eye. Thus, when the pupil constricts, it will also move peripherally towards the chamber angle. The key to managing the coloboma properly is therefore to separate the peripheral iris sphincter tissue from the more central tissue.
AT A GLANCE
• The congenital iris coloboma can be quite challenging to manage.
• Even if the IOL is well centered, its edge may still be visible in an abnormal pupil, resulting in positive dysphotopsias or double vision. Simply closing the peripheral portion of the coloboma will not produce an acceptable outcome.
• The key to managing the coloboma properly is to separate the peripheral iris sphincter tissue from the more central tissue. The author shares a refinement of a technique that he and his colleagues published in 2006.
SURGICAL TECHNIQUE
The technique described in this article and demonstrated in the companion video is a refinement of one my colleagues and I published in 2006.1
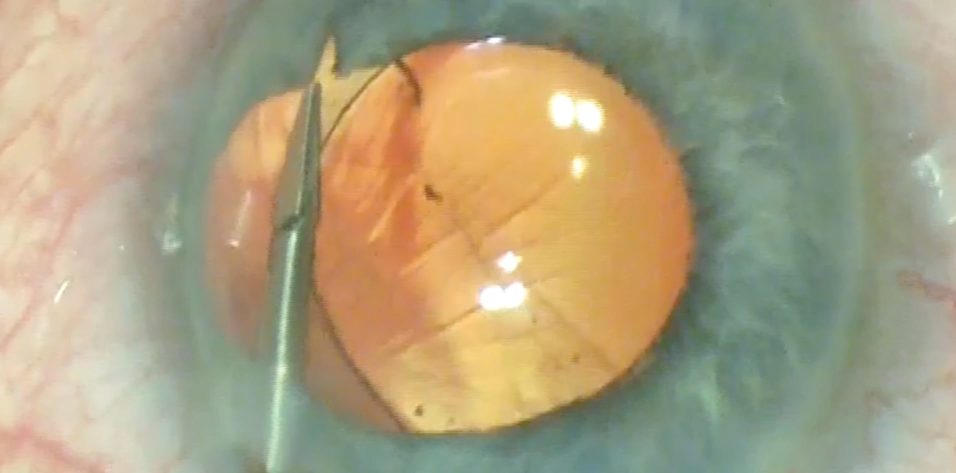
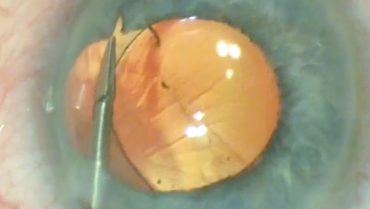
After removing the cataract and placing the IOL in a well-centered position (with or without support from a capsular tension ring as needed), I turn my attention to repairing the colobomatous iris. I instill acetylcholine chloride intraocular solution to constrict the pupil. Using intraocular scissors (MicroSurgical Technology [MST]), I cut the iris sphincter in the midperiphery under the protection of an ophthalmic viscosurgical device (Figures 1 and 2).
Figure 1. The surgeon uses MST intraocular scissors to incise the sphincter.
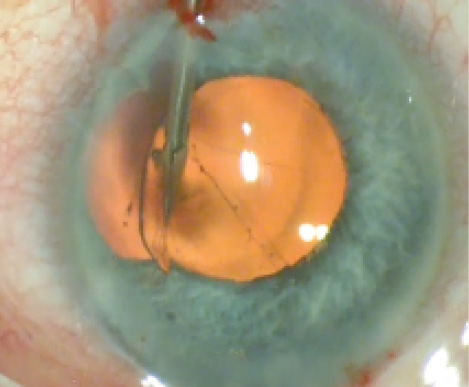
Figure 2. MST intraocular scissors incise the sphincter on the opposite side.
How close to the iris base the tissue is cut depends on how eccentric the pupil is and its size. In general, I gauge the incisions to permit enough remaining central iris sphincter tissue to form for a 3- to 4-mm pupil. The length of the incisions also depends on how eccentric the pupil is. Typically, I make the incisions about 1.5- to 2-mm long. Severe colobomata with very small and eccentric pupils require larger incisions. Severing the iris sphincter in this manner releases the pupil’s attachment to the iris base and chamber angle. Next, I suture the more central sphincter leaflets with 10–0 Prolene (Ethicon), using a modified Siepser knot, to provide a more central, round, and functional pupil (Figure 3).
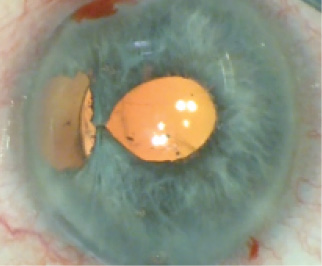
Figure 3. The surgeon uses a 10–0 nylon suture to bring the central iris leaflets together.

Figure 4. With MST Micro-Holding Forceps, the surgeon teases the peripheral iris tissue centrally.
These are just the first steps in the coloboma repair. The large peripheral defect must now be addressed. The next step is critical to maintaining a central pupil. Using a 23-gauge MST Micro-Holding Forceps, I grasp the peripheral iris remnants and tease them centrally (Figure 4). Some angle hemorrhage should be expected during this maneuver, but the bleeding is typically limited and simply aspirated to improve visualization before the placement of more sutures. Stretching this tissue creates small peripheral iris defects, but it also allows me to approximate the peripheral iris remnants to the more central iris tissue without causing the pupil to move towards the angle. The more maneuverable peripheral remnant can be approximated to the pupillary margin near where the central leaflets were brought together with a similar suturing technique (Figure 5). Next, I close the remaining slit-like peripheral iris defects with two additional Siepser-style suture passes (Figure 6).

Figure 5. The more maneuverable peripheral iris remnant is sutured with 10–0 nylon to where the central leaflets were approximated.


Figure 6. Using 10–0 nylon, the surgeon sutures the first (Above) and second (Below) slit-like defects.
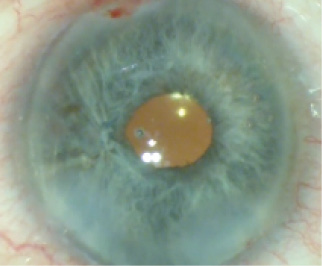
Figure 7. The final result is a centered, round, and functional pupil.
CONCLUSION
In my hands, this technique has been effective and reproducible. It results in a pupil that constricts in a normal circumferential manner without moving peripherally (Figure 7).
1. Cionni R, Karatza E, Osher R, Shah M. Surgical technique for iris coloboma repair. J Cataract Refract Surg. 2006;32(11):1913-1916.