Case Presentation
A 74-year-old man presents with increasing diplopia and decreasing vision in his left eye over the past several months. The patient underwent cataract surgery approximately 15 years ago. He reports no history of trauma.
On examination, the patient has 20/200 UCVA OS. The slit-lamp examination reveals an inferiorly displaced three-piece IOL with a dense Soemmering ring visible superiorly (Figure). The posterior capsule is open. The pupil does not dilate well. Optical coherence tomography of the retina is normal.
How would you approach this case? Would you try to work with the existing IOL, or would you plan to exchange it?
—Case prepared by Audrey R. Talley Rostov, MD, section editor.
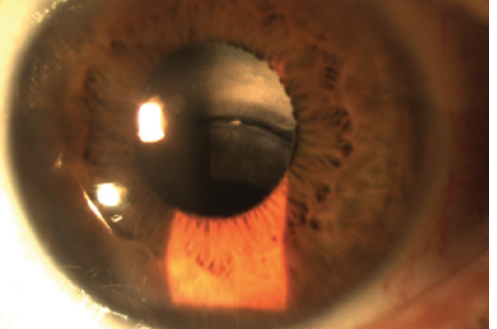
Figure. An inferiorly displaced three-piece IOL and a dense Soemmering ring superiorly.

ALAN S. CRANDALL, MD
With this presentation—late subluxation, capsular phimosis, poor pupillary dilation, and a Soemmering ring—the patient most likely has pseudoexfoliation (PXF) syndrome.1
I prefer to make the decision as to refixation of a decentered IOL versus explantation with exchange for a new IOL during the actual surgery based on a number of factors. I therefore come prepared with multiple options ready to go. If the lens were structurally fine (no defects from a YAG laser, scratches, etc.), then I would attempt to use that complex and fixate it to the sclera. In many of these eyes, a capsular tension ring (CTR) is in place, in which case I use a lasso technique described by Kirk and Condon that uses a 9–0 Prolene suture (Ethicon).2 I find this approach to be minimally invasive, time conserving, and relatively easy to perform. It can also be done without a CTR, in this case with a three-piece lens. There are several techniques to use the existing lens if the bag appears too weak for suturing. One could remove the bag and the Soemmering ring (which often is not easy and may require manual extraction), after which the lens could be iris fixated,3 glued to the sclera, or addressed with the Yamane technique that I now use.4
If I needed to explant the complex, then I would try to cut the implant to pass through a small incision and would sclerally fixate an Akreos Micro Incision Lens (Bausch + Lomb) with a CV-8 Gore-Tex suture (W.L. Gore & Associates; off label). One could also consider a standard anterior chamber lens if no glaucoma exists or an Artisan lens (Ophtec; FDA trial ongoing).

KENDALL DONALDSON, MD, MS
This appears to be a classic case of PXF syndrome with progressive zonular weakness, probable phacodonesis, and a subluxated three-piece IOL. In these cases, I am always pleased to see a three-piece IOL instead of a single-piece acrylic lens, because the former presents more options and simpler methods for repair. Given the potential for such sequelae, it is often best to place a three-piece IOL (either with or without a CTR) in PXF patients who exhibit limited pupillary dilation at the time of the original surgery. Not only do the Prolene haptics of a three-piece IOL add rigidity to the capsular bag complex, but they can later be used for iris suturing, scleral suturing, or gluing through a scleral tunnel if eventual subluxation occurs. In this case, I would preserve the original IOL, whereas if this were a single-piece lens, I would opt for an IOL exchange.
My preference here would be to perform a limited pars plana vitrectomy and prolapse the optic through the pupil. The haptics could then be sutured to the iris using a 10–0 Prolene suture and Siepser sliding knots. Once the haptics have been secured to the iris, the optic could then be returned to its position and centered behind the iris. Based on my experience, this would be the simplest approach, but other options include suturing the haptics to the sclera (with 10–0 Prolene or CV- 8 Gore-Tex) or passing the haptics through the sclera and tunneling them beneath a scleral flap to be glued in place through the technique popularized by Amar Agarwal, MS, FRCS, FRCOphth. As with any intervention, the surgeon’s comfort and familiarity with various techniques will dictate the best approach. All of these options are viable, and whichever the surgeon feels most comfortable with will likely yield the most favorable outcome. Overall, however, preserving the original IOL and securing it to surrounding structures would be the easiest and quickest method if at all possible.

MICHAEL D. GREENWOOD, MD
The figure shows a subluxated IOL. Given the poor pupillary dilation and presumed loss of zonules, this patient likely has a history of PXF. The worsening diplopia and decreasing vision in the setting of a normal retinal optical coherence tomography scan are likely due to the displaced IOL.
Because this patient has a three-piece IOL and a large Soemmering ring, I would fixate the existing IOL to the sclera. The haptic and Soemmering ring would support the suture. I would use iris hooks to give me a clear view of the haptics and to see if there were any vitreous prolapse. If so, I would perform a limited pars plana vitrectomy, while making sure to support the IOL. I would create a Hoffman pocket near the optic-haptic junction and a second pocket 180º away. Next, I would pass a 26-gauge hollow needle through the pocket, under the haptic, and through the capsular bag. I would then dock the long needle of a double-armed 9–0 Prolene suture and externalize the needle. I would repeat this maneuver, going above the haptic, to form a loop around the haptic. Then, I would repeat these steps on the other side. Alternatively, the surgeon could use a Gore-Tex suture (off label) in a handshake technique, but the dense Soemmering ring might make this approach difficult.
Regardless of technique, it would be important to avoid tilting or twisting the optic. I would therefore tie the sutures in a 3-1-1 fashion, while making sure not to overtighten them, and center the optic.

PRIYANKA SOOD, MD
Although cases like this one are challenging, they can also be very gratifying. In this situation, I prefer to keep the three-piece lens in the eye. Given the poorly dilating pupil, I would aim to iris fixate the IOL. Ophthalmologists have moved toward scleral fixation with newer techniques in recent years. I have had good results with iris-fixated IOLs in the past, however, and I think this particular patient would do well with this solution.
After gently filling the anterior chamber with viscoelastic, I would begin by anteriorly capturing the IOL through the poorly dilated pupil to temporarily hold the lens in place. If I felt the pupil was not small enough, I would first inject acetylcholine (Miochol-E; Bausch + Lomb) into the anterior chamber. Next, using a Sinskey hook, I would tilt the lens haptic forward to highlight the location of the haptic behind the iris. I would then use 9–0 polypropylene on a CIF-4 needle to fixate the haptic to the iris using a Siepser slipknot and modified McCannel technique through small corneal incisions.
Once the lens was secure, I would push the optic back through the pupil and gently remove the viscoelastic with a Simcoe cannula. This approach would likely yield great results with the smallest incisions and least manipulation. Scleral fixation could also be attempted, but I suspect it would be more challenging because of the small pupil.

DARCY H. WOLSEY, MD, MPH
I would attempt to keep the IOL in the eye if possible. Siegel and Condon described a noninvasive method of using the fibrosed capsular bag and a single iris suture for capsulorhexis fixation.5 Keeping the bag intact would avoid disrupting the Soemmering ring. In Siegel and Condon’s technique, the surgeon grasps the edge of the capsulorhexis with a microsurgical forceps to stabilize the IOL. He or she passes a 10–0 polypropylene suture on a long, curved needle (PC-7; Ethicon) through the midperipheral iris to engage the fibrotic edge of the capsule and then directs the needle back around the superior edge of the capsule, up through the midperipheral iris, and out a previously made paracentesis. The suture is then tied with the modified Siepser knot. Obviously, any vitreous present would need to be removed prior to fixation of the IOL.
If a significant amount of vitreous is present or the lens is significantly mobile, it may be easier for the surgeon to remove the entire complex, clean up the vitreous, and use his or her favorite technique for scleral fixation. The double-needle Yamane method of transconjunctival intrascleral IOL fixation is a noninvasive approach to scleral fixation that may be technically easier than suturing the IOL to the iris and capsule and may provide better stability in the future, less risk of uveitis-glaucoma-hyphema syndrome, and a lower risk of inflammation from disruption of the Soemmering ring.4

WHAT I DID: AUDREY R. TALLEY ROSTOV, MD
I made four incisions with a bimanual 1.3-mm diamond blade in anticipation of Otis suture fixation, and I used a dispersive ophthalmic viscosurgical device to examine/viscodissect the IOL and capsule. With microscissors and forceps (MicroSurgical Technology), I created some relaxing incisions on the anterior surface of the phimosed capsular bag, which relaxed the IOL into a more anatomic position. After performing a limited bimanual pars plans vitrectomy, I fixated the IOL to the iris with a 9–0 Prolene suture on a CIF-4 needle and Siepser sliding knots.
1. Jehan FS, Mamalis N, Crandall AS. Spontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology. 2001;108;1727-1731.
2. Kirk TW, Condon GP. Simplified ab externo scleral fixation for late in-the-bag intraocular lens dislocation. J Cataract Refract Surg. 2012;38(10):1711-1715.
3. Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33:1851-1854.
4. Yamane S, Inoue M, Arakawa A, Kadonosono K. Sutureless 27-gauge needle–guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmology. 2014;121(1):61-66.
5. Siegel MJ, Condon GP. Single suture iris-to-capsulorhexis fixation for in-the-bag intraocular lens subluxation. J Cataract Refract Surg. 2015;41(11):2347-2352.




