
A patient presented to my clinic for a fourth opinion who had a longstanding history of difficulty since cataract surgery on her right eye. Her past medical history was significant for severe anxiety and depression, which were both related to her eye condition. She carried a past medical history of a rare hypercoaguable state, resulting in multiple blood clots that required long-term anticoagulation. The patient had a history of head trauma from a motor vehicle accident a few years earlier, and glass remained embedded in her periorbital area.
AT A GLANCE
• A patient presented for a fourth opinion who had a longstanding history of difficulty with recurrent hemorrhages, inflammation and glaucoma since cataract surgery on her right eye.
• On examination, the temporal haptic was found to be dislocated into the sulcus, with overlying transillumination defects of the iris. Subtle IOL tilt was observed. The author diagnosed uveitis-glaucoma-hyphema syndrome and decided to pursue an IOL exchange.
• Aside from a fibrosed nasal haptic, the procedure went as planned, and the patient had an uneventful postoperative course, with full resolution of inflammation and intraocular hemorrhages as well as stable IOP. She recovered excellent corrected visual acuity.
The patient’s past ocular history in her affected right eye was significant for an eight-cut radial keratotomy (RK), cataract extraction with toric IOL placement 6 years prior, YAG capsulotomy, and multiple episodes of spontaneous hyphemas and vitreous hemorrhages resulting in a vitrectomy since cataract surgery. Since her phacoemulsification, she experienced recalcitrant glaucoma and inflammation requiring a Baerveldt glaucoma implant (Johnson & Johnson Vision) in the right eye.
Gonioscopy revealed that the IOL’s temporal haptic had dislocated into the sulcus, with overlying transillumination defects of the iris (Figure 1). I observed subtle IOL tilt in the horizontal meridian on dilated Scheimpflug imaging (Figure 2).

6" class="Basic-Text-Frame">
Figure 1. Overlying transillumination defects of the iris.
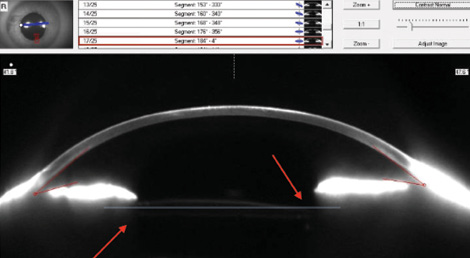
Figure 2. Subtle IOL tilt in the horizontal meridian is observed with dilated Scheimpflug imaging.
TREATMENT PLAN
I diagnosed uveitis-glaucoma-hyphema syndrome and decided to perform an IOL exchange. I felt that adequate anterior capsular support was available for a sulcus IOL. Given the patient’s history of RK, both from an incisional and optical standpoint, and a superior-temporally placed valve, I planned a nasal scleral tunnel approach with IOL exchange, anterior vitrectomy, and sulcus-fixated single-piece CZ70BD PMMA IOL (Alcon) with optic capture. Typically, I would approach phacoemulsification in eight-cut RK with a clear corneal incision. Given the potential complexity of this case and therefore increased risk of RK incision gape combined with the decision to place a large- optic PMMA IOL requiring a larger incision, I decided to use a scleral tunnel. I had a backup plan of scleral fixation in the event of poor capsular support.
As surgery progressed, I found that the nasal haptic was fibrosed into the capsule. Multiple attempts to free the adhesions with a second instrument were unsuccessful. In order to leave the zonular-capsular complex intact, I amputated the distal bulb and removed the IOL. Cutting the optic was not necessary due to the larger incision for the PMMA IOL. The superonasal surgical approach in the right eye was awkward, requiring me to perform surgery with my nondominant left hand for the majority of the case.
George O. Waring IV, MD, performs an IOL exchange in a patient with uveitis-glaucoma-hyphema syndrome.
Otherwise, the procedure went as planned, and the patient has had an uneventful postoperative course, with full resolution of inflammation and intraocular hemorrhages as well as stable IOP. She recovered excellent corrected visual acuity (see video above).




