Improved Astigmatism Management With the Catalys’ Laser Marking and Registration Modules
Shachar Tauber, MD

It has always been challenging to correct astigmatism accurately at the time of cataract surgery, but this is a major contributor to patients’ postoperative satsifaction.1 Success with a toric IOL requires identification of the correct axis and stable placement of the lens on the target axis. Just 5º to 10º of rotational misalignment of the IOL can reduce the toric effect by up to 30%.2 Limbal relaxing incisions, which in my practice have been replaced by femtosecond laser intrastromal arcuate incisions, provide an opportunity to address lower levels of astigmatism but also require exact placement.
The new cOS 6.0 software for the Catalys Precision Laser System (Johnson & Johnson Vision) facilitates both kinds of correction by enabling the direct importation of preoperative data from the Cassini (i-Optics), the biomorphometric intraoperative registration of iris features, and precise laser marking.
MORE PRECISE MARKING
I have been dissatisfied with manual ink marking when I am using a highly sophisticated femtosecond laser (Figure 1). Manual ink marking is imprecise; it accounts for up to 10º of axial misalignment3,4 due to the thickness of the ink mark and the inconsistencies introduced by the marker. In too many cases, the marks run or disappear or my view of them is blocked by the laser interface.
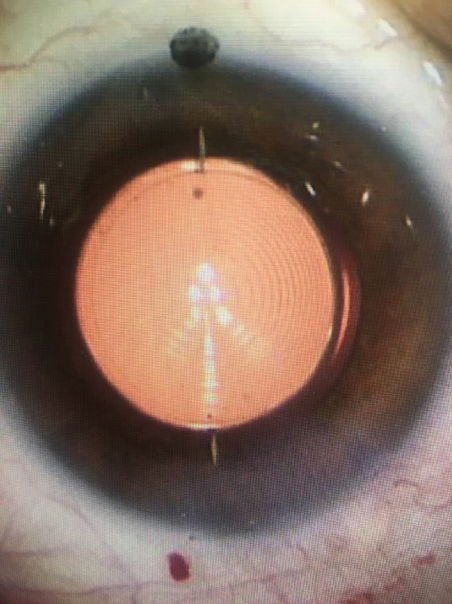
Figure 1. Intrastromal marks made by a Catalys laser are more precise than the adjacent scleral ink mark.
The latest Catalys software eliminates the need for manual marks. It compares the pre- and intraoperative iris anatomy data and compensates for tilt and rotation so that the laser marks are perfectly aligned to the steep meridian and the target axis. The radial intrastromal marks can be centered on the capsule, just like the capsulotomy, and easily aligned to the marks on the toric IOL. The laser marks have a mean accuracy of 0.6º, providing more than five times greater precision than a manual ink mark3 and giving me much greater confidence in my toric IOL results.
The alignment marks are easy to visualize under an operating microscope and remain visible for several months postoperatively, which is helpful for confirming alignment.
A MORE EFFICIENT WORKFLOW
Linking preoperative diagnostic information to the laser minimizes data entry and eliminates several steps in the planning process for toric IOLs and arcuate incisions (Figure 2). The examination, evaluation, and treatment planning are all done preoperatively with the Cassini, and these data are imported via a wireless connection or USB drive to the laser.
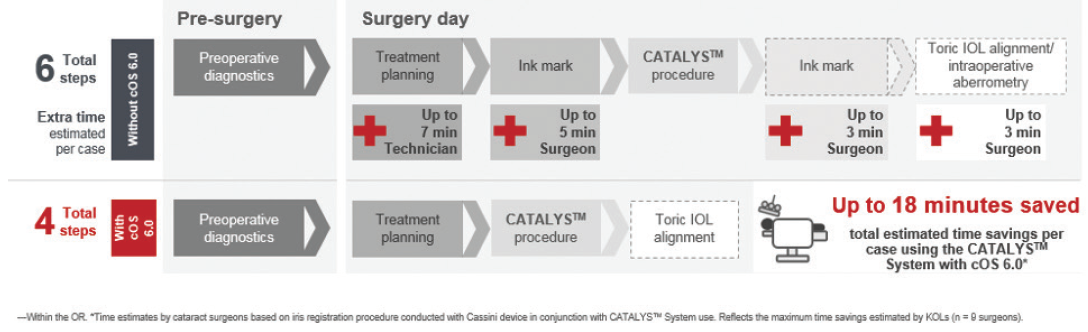
Figure 2. Improved toric IOL alignment workflow.
Figures 1 and 2 courtesy of Shachar Tauber, MD
Toric calculators and the Donnenfeld incisional nomogram are integrated into the system. I prefer to use the nomogram for intrastromal arcuate incisions described by Julian D. Stevens, MD,5 but I am looking forward to evaluating whether the advantages of having an automatically calculated nomogram outweigh the value of this intrastromal-specific nomogram. It’s also possible that additional nomograms may be programmed into the software in the future.
ENHANCED SAFETY AND ACCURACY
Iris detection is a major improvement in the precision with which the laser creates arcuate incisions of consistent length and depth. The intraoperative iris features are referenced and adjusted to those from preoperative Cassini tomography to identify precisely the target location for the incisions. This avoids problems that can arise from cyclorotation as well as docking-related tilt, which is otherwise impossible for the surgeon to identify and compensate for.
Finally, iris detection largely eliminates the potential to operate accidentally on the wrong eye or patient. These enhancements in precision and safety are steps in the right direction for surgeons who continually want to perfect their cataract surgery and astigmatism management outcomes.
1. Watanabe K, Negishi K, Kawai M, Torii H, Kaido M, Tsubota K. Effect of experimentally induced astigmatism on functional, conventional, and low-contrast visual acuity. J Refract Surg. 2013;29(1):19-24.
2. Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg. 2008;34(10):1631-1636.
3. Visser N, Berendschot TTJM, Bauer NJC, Jurich J, Kersting O, Nuijts RMMA. Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg. 2011;37(8):1394-1402.
4. Titiyal JS, Kaur M, Jose CP, Falera R, Kinkar A, Bageshwar LM. Comparative evaluation of toric intraocular lens alignment and visual quality with image-guided surgery and conventional three-step manual marking. Clin Ophthalmol. 2018;12:747-753.
5. Day AC, Lau NM, Stevens JD. Nonpenetrating femtosecond laser intrastromal astigmatic keratotomy in eyes having cataract surgery. J Cataract Refract Surg. 2016;42:102-109.
Femto LDV Z8: Strong Technical and Workflow Features
Neda Nikpoor, MD

The Femto LDV Z8 (Ziemer) is a state-of-the-art femtosecond laser. It is less well-known than its competitors, but technical and workflow features set the Z8 apart from the rest. I have used every major platform, and I have found the Z8 to be the most efficient and the easiest to use. In my experience, it also provides the best surgeon and patient experiences.
SURGEON EXPERIENCE
The Z8 has the lowest pulse energy, shortest pulse duration, and highest repetition rate of any femtosecond laser available in the United States. Why is this important? These specifications directly affect patient outcomes.
Studies of aqueous samples have demonstrated that higher energy can lead to prostaglandin release, which may result in greater inflammation and pupillary constriction.1 I find the use of intracameral Shugarcaine (epinephrine 0.025%/lidocaine 0.75%) to be necessary during laser cataract procedures performed with other systems but not with the Z8 because the pupil size does not change. I also notice far fewer bubbles during laser cataract surgery with the Z8, which facilitates visualization and hydrodissection. Additionally, I find cortical removal to be easier when I use the Z8 because the cortex is not as sticky as it is after treatment with other femtosecond lasers.
Low pulse energy reduces postoperative inflammation. This combined with an overlapping cut pattern and a high repetition rate produces highly precise corneal incisions with few tissue bridges and a capsulotomy edge that is indistinguishable from that of a manual capsulorhexis on electron microscopy (Figure 3).2 I have found the smooth edge of this capsulotomy is stronger than the capsulotomy edges created with other femtosecond lasers, likely because higher pulse energy creates weaker capsulotomies.3 I have encountered many more anterior capsular tags and tears during laser cataract procedures that I have performed with other platforms.
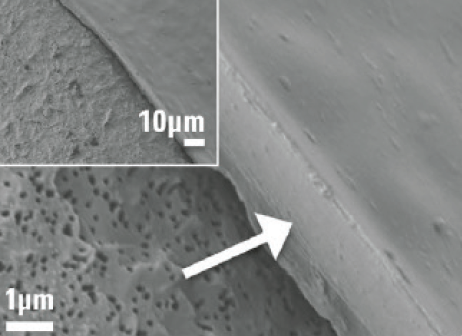
Figure 3. Capsulotomy edge cut with a Femto LDV Z8 using low pulse energy in a human eye.
Figure 3 courtesy of Ziemer
The Z8 may be used for cataract surgery and corneal procedures. It has a small footprint and is mobile. Because the Z8 is easily moved between multiple surgery centers, the acquisition cost of the unit can be shared.
PATIENT EXPERIENCE
Because laser cataract surgery performed with the Z8 can be performed sterile in the OR, it is one continuous procedure for the patient and the surgeon. Patients are prepped, draped, and anesthetized in the OR. I find that they are much more comfortable with this arrangement than when the laser procedure must be performed in a separate room without sedation. This single-surgery approach improves patient flow with less time in surgery, less overall time in the ambulatory surgery center, and less contact with staff.4
Low suction and a liquid patient interface offer excellent patient comfort (Figure 4). In my experience, the low suction also minimizes or eliminates the incidence of subconjunctival hemorrhage. A smooth build in vacuum also facilitates a comfortable patient experience.

Figure 4. The liquid patient interface of the Femto LDV Z8 is docked to the eye.
Figure 4 courtesy of Neda Nikpoor, MD
1. Liu YC, Setiawan M, Ang M, Yam GHF, Mehta JS. Changes in aqueous oxidative stress, prostaglandins, and cytokines: comparisons of low-energy femtosecond laser-assisted cataract surgery versus conventional phacoemulsification. J Cataract Refract Surg. 2019;45(2):196-203.
2. Williams GP, George BL, Wong YR, et al. The effects of a low-energy, high frequency liquid optic interface femtosecond laser system on lens capsulotomy. Scientific Reports. 2016;6:24352.
3. Pisciotta A, De Maria M, Verdina T, Fornasari E, de Pol A, Cavallini GM. Anterior capsule of the lens: comparison of morphological properties and apoptosis induction following FLACS and standard phacoemulsification surgery. Biomed Res Int. 2018;2018:7242837.
4. Vasquez-Perez A, Simpson A, Nanavaty MA. Femtosecond laser-assisted cataract surgery in a public teaching hospital setting. BMC Ophthalmol. 2018;18(1):26.
Improvements to the Lensar Enhance Surgical Adaptability
Robert J. Weinstock, MD

One of the many lessons I learned this past year is that adaptability is important. I discovered that I could change the way I practice in order to remain successful but that changing my capital equipment was not so easy. I have therefore never felt more confident about my decision 7 years ago to acquire a Lensar Laser System (Lensar) because the company is committed to innovation. Lensar has continually improved its system to adapt to surgeons’ changing needs and to meet patients’ rising expectations, with six upgrades since the product’s initial launch.
CATARACT DENSITY IMAGING
Cataract density imaging (CDI) is a great example of Lensar’s innovations. This feature has taken laser cataract surgery to a whole new level. Thanks to augmented reality that uses Scheimpflug imaging, ray tracing, and 3D modeling software, CDI can grade the cataract 1 through 5 and identify the location and density of the nucleus to optimize fragmentation. After imaging and grading the cataract, the CDI software automatically adapts and recommends the most efficient fragmentation pattern based on my preferences.
This is important for two reasons. First, it expedites lens fragmentation by using appropriate laser energy targeted to the densest part of the lens, which varies depending on what grade of cataract is present. Second, it significantly limits or eliminates phaco energy, which improves visual outcomes on postoperative day 1 and speeds up recovery. Other femtosecond laser platforms that use OCT imaging do not have the resolution or imaging capable of grading cataract density and nucleus size.
INTELLIAXIS REFRACTIVE CAPSULORHEXIS
Preoperative information is imported wirelessly into the laser, which avoids the potential for transcription errors. The IntelliAxis Refractive Capsulorhexis marks the capsule and the cornea on the steep axis. I find this feature indispensable for cataract surgery on patients receiving a toric IOL and those receiving arcuate incisions to correct their astigmatism.
The system uses iris registration to eliminate cyclotorsion errors. Once docking of the laser is complete, iris registration is accomplished in less than 3 seconds. I no longer need to mark the cornea preoperatively or use other alignment tools during the cataract procedure. This is a huge time-saver.
FUTURE INNOVATION
Lensar plans to launch Ally, the market’s first cataract system that combines a femtosecond laser and phaco device, early next year. This will eliminate the need to roll patients between machines, and I am eager to evaluate the system’s impact on surgical efficiency and practice economics.
Digital Marking and Planning With the LenSx
O. Bennett Walton, MD, MBA

The use of a femtosecond laser for certain steps of the cataract procedure can enhance the surgical experience. When used in combination with other advanced technologies, femtosecond lasers can produce more predictable postoperative outcomes1 and offer additional value in the clinic for other ophthalmology procedures.
The increased predictability of spherical equivalent after laser cataract surgery is likely due to the standardized centration and sizing of the capsulotomy. Systems such as the LenSx (Alcon) deliver reproducible circumferential optic coverage, reduce lens tilt, and ensure a consistent effective lens position.1
In addition to cataract functionality, users who have upgraded to the latest LenSx software can use the laser to create flaps, sidecuts, tunnels, and pockets. The laser-assisted creation of tunnels and pockets is useful for the implantation of intrastromal corneal ring segments and presbyopia-correcting inlays.
Integration of the LenSx with the Verion Image Guided System (Alcon) increases accuracy and efficiency during surgical planning and execution. The company’s recent acquisition of the Argos biometer should facilitate digital marking and planning of astigmatic correction with toric IOLs and laser arcuate astigmatism correction.
1. Yeu E. Retrospective comparison of clinical outcomes associated with manual and femtosecond laser-assisted cataract surgery. Paper presented at the: 2018 ASCRS/AOA Annual Meeting; Washington, DC; April 13-17, 2018.
Centration, Comfort, and Versatility With the Victus
Mitchell Shultz, MD, and Abraham Chorbajian


It is hard to believe that nearly 10 years have passed since I (M.S.) first wrote about femtosecond lasers for cataract surgery. This technology had just debuted at the ASCRS Annual Meeting in San Diego and sparked my curiosity, and I was determined to learn everything I could about the various platforms. I spent the better part of the next 2 years doing research, watching other surgeons operate, meeting with industry executives, and visiting with the engineers who worked on all of the platforms available at the time. After completing my due diligence, I decided that the best platform for our center was the Victus femtosecond laser (Bausch + Lomb). It offered versatility for optimizing the accuracy and precision of corneal incisions and cataract surgery.
Nearly 8 years later, our practice has benefited greatly from this platform’s versatility for making consistent LASIK flaps, creating precise arcuate and corneal incisions, performing accurate capsulotomies, and presoftening cataracts with various fragmentation patterns (Figure 5).
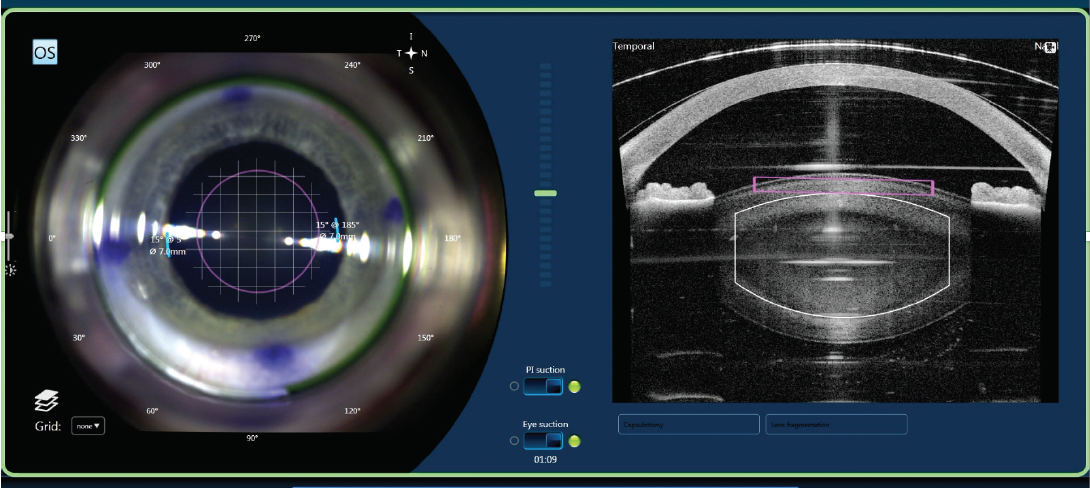
Figure 5. A treatment management screen of the Victus femtosecond laser.
Courtesy of Mitchell Shultz, MD
IMAGING AND GUIDANCE
The Victus is the only laser platform in its class to offer high-resolution, real-time OCT imaging and guidance. This makes it easier to plan and customize a grid fragmentation pattern. Coupling the Victus with the Stellaris Elite (Bausch + Lomb) for phacoemulsification has greatly reduced our total and effective phaco times by as much as 75% compared with traditional phacoemulsification without a femtosecond laser.
The live OCT imaging and state-of-the-art capsule scan allow us to optimize the position and effectiveness of capsulotomies and to customize the pattern of lens fragmentation to best suit each eye. A growing number of patients are choosing toric, accommodating, extended depth of focus, trifocal, and adjustable IOLs. Pairing these technologies with the Victus laser helps us to achieve the best possible refractive results for our patients.
CENTRATION AND COMFORT
The Victus can automatically center the procedure on the pupil, limbus, apex, or other positions, which facilitates the creation of well-centered corneal flaps and capsulotomies. With the soft silicone rim of the Victus Verafit patient interface, our patients do not complain about pain when their eyes are coupled to the laser. A recent redesign includes a curved liquid interface, which increases patient comfort and permits more flexible parameters for performing multiple procedures.
The combination of real-time live visualization, real-time OCT imaging, and the curved liquid interface help to minimize the risk of complications such as suction loss and conjunctival hemorrhage. The patient interface also provides optimal stability during creation of the LASIK flap, and it avoids posterior corneal folds, which can affect the anterior capsulotomy secondary to translation artifacts.
VERSATILITY
The integrated bed of the Victus allows cataract and corneal procedures to be executed under one workstation, and it can be used in conjunction with the Technolas Teneo excimer laser (Bausch + Lomb) to round out a complete refractive suite. This cost-effective versatility can enhance workflow and provide a high-quality surgical experience.
I (M.S.) typically spend less than 4 minutes total in the laser suite because most treatments take less than 2 minutes from start to finish. When I am operating, I generally perform a case with the Victus, go to the OR to perform phaco cataract surgery, and then return to perform another case with the Victus. This means I do not spend time waiting for the OR to be turned over.