Finding Opportunity After Crisis
By Francesco Carones, MD; and Amanda Cardwell Carones, MPH

Advantages of an Overnight Change
When we traveled to Marrakech, Morocco in February for the Winter ESCRS meeting, we had no idea how much our world would change before we even returned home to Milan, Italy. At the time of this writing, there have been 13 weeks since Italy’s first confirmed case of COVID-19 and 11 weeks of lockdown. Only now can we finally leave our home—but only for essential work, to buy essential items, and to walk our dogs a maximum of 200 meters from our doorstep. A self-declaration form is required every time we go outside. Grocery shopping must be done at the nearest shop. Traveling outside of the town limits is not permitted. Masks are mandatory at all times. Children are not allowed outside at all.
For many of us, our habits changed literally overnight. Before COVID-19, this 42-year-old mom of two was accustomed to frequent travel and daily face-to-face interactions with clients, colleagues, and friends. Thanks to the pandemic, I have suddenly found myself smart-working from home, staring at a computer screen for hours on end with breaks only to feed and care for my kids.
In the beginning, I tried to enjoy virtual happy hours with friends, but those grew old quickly. Webinar fatigue is bad enough, but add to it the complications of eyestrain, misplaced glasses, dry eye, and a tiny bit of uncorrected hyperopia, and suddenly I became an irritable 42-year-old, stay-at-home-while-smart-working-and-homeschooling, presbyopic mom of two.
FINDING THE SILVER LINING
About 2 weeks into our new normal, I told my husband, Francesco Carones, MD, that there could be blessings at the end of this disaster. I was sure that other 40-to-55-year-olds had developed a sudden attachment to reading glasses and detestation for their computers. There were certainly also active people in their early 70s, now occupying their quarantine time with more near-vision activities, who would be noticing early symptoms of cataracts. Then there are the contact lens users who can’t run out to buy new lenses and solutions and who have been repeatedly warned of their increased risk for viral contamination.
The bottom line is that, during this crisis, many individuals now have an increased awareness of the importance of vision. This newfound appreciation for good vision could potentially drive stronger demand for vision correction and preventive therapies.
It is possible that, after an initial societal reopening phase, consumers may choose to spend money on health-minded purchases that can provide long-term benefit1 rather than buying the newest designer handbag or shoes. In April, the Boston Consulting Group predicted that a pent-up demand for medically necessary procedures will make preventive health an “explicit winner” in the post–COVID-19 period.2
This confirmation was the motivation we needed to radically reassess how we connect with our patients, especially in those conversations that eventually lead to patients booking surgical procedures. What if we gently informed patients that their blurry computer vision, headaches, dry eyes, and tiredness could potentially be addressed? What if there were a way to eliminate the glasses that fog every time they put on a mask? What if they could address it now and have one less thing to worry about during future quarantines?

Putting Theory Into Practice
We never completely shut our doors to patients during the lockdown period, but we did use a rotating, bare-minimum staff, and we focused primarily on urgent patient visits. In mid-April, we opened our surgery schedule again and almost immediately noticed a renewed level of interest in surgical (cornea- and lens-based) consultation visits.
Since most of our lens-based procedures are at least partially covered by private insurance, we expect to see a quick return to pre–COVID-19 levels in the 55-plus age group, probably by early summer. As cornea-based procedures are mostly paid out-of-pocket, we initially expected case volume to resume to near-normal in early fall. However, based on phone call trends, it seems laser refractive procedures may bounce back to higher-than-normal levels even before summer. At present, our main goal is to drive interest and to reassure patients that we are here for them when they are ready.
NEW PRACTICE, NEW PROCEDURES
Fortunately, when we built our new office (which opened only in late January), the layout was designed specifically to minimize wait times, optimize patient flow, and provide more space per patient. This has obvious advantages now because it avoids the need for major structural or scheduling changes to facilitate social distancing.
In early April, we implemented a formal protocol for the safety and well-being of our staff and patients.
Staff guidelines. Staff members are required to wear surgical gowns, N95 or FFP2 masks, shoe covers, hair covers, goggles or face shields, and gloves. Movement of staff within the clinic is limited; those in administrative roles are not allowed in patient care areas. Before the COVID-19 crisis, we had switched to using disposable surgical instruments, which is one further way we can minimize exposure to our staff.
Patient guidelines. Patients are requested to attend visits alone, except when a caregiver is required, and are permitted to enter the clinic no more than 10 minutes ahead of their appointment times. When they enter, they receive a branded patient wellness kit that includes a disposable gown, shoe covers, hair cover, and face mask (Figure 1). No-touch hand sanitizer stations are positioned throughout the clinic and in each patient room.

Figure 1. Customized masks, included in patient wellness kits, are provided at check-in.
When patients call to schedule appointments, they are triaged by answering questions about recent fever or potential exposures. These questions are repeated during the appointment reminder call.
We installed an infrared camera so that we can monitor the temperature of anyone who enters the building. We do mandatory rapid immunoglobulin M and immunoglobulin G testing on surgery day for surgical patients and offer it as an at-cost option for clinic patients. These initiatives, especially the antibody testing, have garnered extremely positive feedback from patients.
PATIENT COMFORT AND OUTREACH
Implementing our new safety protocols was relatively easy, but helping patients to feel comfortable scheduling an appointment was more challenging. We found that implementing three new educational and service offerings was helpful.
Webinars. We host a patient outreach webinar series, led by Luca Vigo, MD, and me from our respective homes, to help convey to our patients that we are all in this together (Figure 2). During each webinar, we discuss our safety protocols and review ocular health issues related to COVID-19. After more than 150 participants attended the first webinar, we decided to introduce small group webinars so that participants can interact directly with the surgeons and with other patients. It is essentially an informal chat where all vision-related questions are welcome.

Figure 2. Small group webinars hosted by Carones Vision are used to discuss safety protocols and review COVID-19–related ocular health issues.
Figures 1 and 2 courtesy of Francesco Carones, MD
Web consultations. Our appointment times are now spaced further apart, giving the surgeons about 10 to 15 minutes between patients. In that time, we also offer patients 10-minute web consultations at no charge to speak directly with their ophthalmologist before coming in to the clinic. The web consult enables us to establish rapport, it helps patients feel confident in their decision to schedule the appointment, and it also provides an opportunity for the ophthalmologist to better understand each patient’s personal vision requirements and to reduce chair time in the clinic. Family members can be present and participate in the web consultation, which we have always advocated for in the decision-making process.
Home visits. The third service that we have introduced for patients living in Milan is home visits for basic vision examinations. During the home visit, autorefractometry and visual testing, slit-lamp examination of the anterior and posterior segments, evaluation of the tear film, and tonometry are performed with handheld portable devices.
CONCLUSION
In our practice, the focus right now is not solely to recoup financial losses; we feel it’s just as important to provide patients with services that build trust and confidence and fill gaps in the services currently available in our market. We truly believe that surgical volume will follow.
1. Murillo-Vargas D. How the COVID-19 pandemic is influencing consumer behavior. Contentserv Group. March 26, 2020. https://www.contentserv.com/en/blog/how-covid-19-pandemic-is-influencing-consumer-behavior. Accessed May 8, 2020.
2. Koslow L, Lee J, Bharadwaj A, Sanghi K, Barrios G. COVID consumer sentiment snapshot #5: a story for the ages. Boston Consulting Group. April 13, 2020. https://www.bcg.com/publications/2020/covid-consumer-sentiment-survey-snapshot-4-13-20.aspx. Accessed May 8, 2020.
COVID-19 in Hong Kong
By John S.M. Chang, MD

In late December 2019, the outbreak of COVID-19 started in mainland China. Immediately after the first confirmed case in Hong Kong was reported on January 24, everyone started stockpiling surgical masks and disinfectants, and the government rapidly took measures to combat the virus and prevent a massive outbreak. The quick actions of our residents and our government were mostly because of the lessons learned from our painful experience with the severe acute respiratory syndrome (SARS) outbreak in 2002 and 2003.
In Hong Kong, the spread of COVID-19 was contained early on, and the number of infected individuals fell into the single digits until a mass return of students from overseas occurred in mid-March. These students went out to bars and restaurants without wearing masks and started a second wave of community outbreak.
WHY ARE MASKS IMPORTANT?
In 2003, if a patient became infected with SARS, symptoms would manifest after 3 to 7 days, but they became contagious only after the symptoms appeared. Importantly, the symptoms were generally quite severe and distinguishable from common upper respiratory diseases such as the common cold or flu.
COVID-19 is far more infectious than SARS. The incubation period is suggested to be 1 to 14 days (median, 5.1 days),1 but in rare cases this period can be up to 27 days.2 And in an important distinction from the 2003 SARS illness, individuals infected with this coronavirus (SARS-CoV-2) can be contagious during the entire incubation period and be completely asymptomatic.
In this regard, wearing surgical masks is crucial, as we never know who is infected and contagious. If individuals wear surgical masks only after they develop related symptoms, they may have already spread the virus to many of their colleagues, friends, and relatives during an asymptomatic incubation period.
Mask wearing slows the infection rate, allowing time to track cases and prevent a massive outbreak. It does not completely prevent us from infection, but it does lower the dosage if we get infected, allowing time for antibodies to develop to fight the virus.
POLICIES AND MEASURES IN OUR HOSPITAL
New policies and measures for infection control have been adopted by our hospital for both visitors and staff.
Masks. All visitors entering the hospital must wear their own masks; we do not provide them. Patients are required to wear a mask at all times during their clinic visits. The exception is during refractive surgery such as LASIK and SMILE. Patients must leave their masks in the waiting area before they enter the OR because the masks may have been contaminated elsewhere. Masks are removed when povidone-iodine is applied to the patient’s face and eyelids. Our ORs are positively pressured. Patients are required to put on the masks again when they return to their recovery cubicle after the completion of surgery.
Entering the facility. Before entering the main entrance of our hospital, all visitors must use alcohol hand rubs provided by the facility. They are also required to have their body temperature measured at the main entrance. Staff members ask health-related questions about patients’ infection risk when they arrive at the front door and again when they sign in at the registration counter. The same questions were also asked when they initially called to schedule their appointment. (For a list of these questions, see Questions to Ask Patients.)
Also at the registration counter, patients must fill out an epidemiologic surveillance and triage form. Questions include whether they have been symptomatic, have traveled, or have been in close contact with confirmed cases or clusters within the past 14 days.
It may seem obsessive and compulsive asking patients these questions over and over again, but it helps to demonstrate to patients that we are very cautious, and it imparts to them a sense of security.
Staff safety measures. Staff members working at the hospital’s main entrance have on full personal protective equipment (PPE). Doctors wear surgical masks and scrubs and a white coat during patient consultations and examinations. Doctors also have the option to wear full PPE during consultations. In our clinic, staff members take separate lunch hours to avoid group gatherings. In our staff canteens, makeshift clear acrylic partitions have been installed and tables separated.
GOVERNMENT POLICIES
A number of safety policies have been set by the Hong Kong government.
Inbound travelers. All non–Hong Kong residents coming from overseas are denied entry to Hong Kong. Non–Hong Kong residents coming from Mainland China, Macao, and Taiwan are denied entry if they have been to any overseas countries and regions in the past 14 days.
For all asymptomatic inbound travelers, compulsory quarantine is required at designated places (ie, home or other accommodation) for 14 days. Asymptomatic inbound travelers arriving at the Hong Kong airport are subject to the compulsory Enhanced Laboratory Surveillance Programme, which mandates that they undergo COVID-19 testing and wait for test results at a designated location. Asymptomatic inbound travelers who need to wait for test results overnight are temporarily accommodated in a designated hotel. Symptomatic inbound travelers are sent to the accident and emergency department of a hospital for further COVID-19 tests.
All quarantined new arrivals must wear a wristband that is connected to a tracking app on their cell phone. The app will inform authorities automatically if they leave their isolation location. Surprise phone calls and visits to their place of quarantine by government officials are performed to make sure that they stay at their quarantine location.
Public gatherings. From late March to early April, game centers, bathhouses, fitness centers, public entertainment facilities, party rooms, beauty parlors, golf clubs, bars, and karaoke clubs were closed. Also prohibited were any public group gatherings of more than four people. Restaurants were required to distance their dining tables at least 1.5 meters apart or to install acrylic partitions between seats and to limit seating to four people per table.
As of May 8, we have had no local COVID-19 cases for the past 17 consecutive days, and some of these measures have been relaxed. Group gatherings of eight or fewer individuals are now permitted in public places. Cinemas, fitness centers, beauty parlors, and bars have reopened. High schools will resume in the coming weeks. The city is considered free of local transmission after two 14-day periods (ie, 28 days) of zero local cases.
CURRENT STATUS
Our hospital. Our ophthalmology department has two centers. The main hospital, which houses the eye surgery center and clinics, is situated in a residential district; the other center is a refractive surgery center and ophthalmology clinic situated in a commercial building in the city’s business district. During the worst period of the outbreak, our patient volume decreased by approximately 90% at the main hospital and 50% at the business district surgery center. Surgeries were scheduled in the late mornings and early afternoons to reduce manpower and, therefore, the risk of staff infection.
Once the outbreak began to improve, our cataract volume returned to around 60% of normal. As of April 27, our LASIK and SMILE volume has returned to 100%. In fact, some centers in Korea have reported that their refractive surgical volume has increased to 120%. This may be due to two main reasons:
No. 1: Younger patients are not as concerned about the virus because they are less prone to death; and
No. 2: Most patients are working from home right now, so they are able to have surgery without needing to take official time off.
The general public. Hong Kong was never on lockdown. Citizens could go to work, although working from home was and still is encouraged. Nearly all citizens wear face masks in public, and awareness of hygiene has improved, with more frequent handwashing and use of portable alcohol hand rubs. Handshakes, hugs, and kissing are strongly discouraged.
Most people have stayed at home after work and on weekends, and a governmental geodata website provides updates on the latest confirmed COVID-19 cases in Hong Kong and alerts citizens to avoid the places where they are occurring.3 There are also daily news reports of new confirmed cases. When a new case is confirmed, all of that person’s close contacts are quickly traced, and those individuals are quarantined. If the infected person was reporting to an office building, the whole office/apartment building is sterilized.
As of April 27, Hong Kong has performed a total of 154,898 COVID-19 viral tests (20,665 per million population). This is a higher rate than has been performed in the United States, France, or Italy.
CONCLUSION
It is important to create a safe environment in your clinic. When the staff feels comfortable, your patients will also feel comfortable.
At the time of this writing, April 19 was the last reported local transmission of COVID-19 in Hong Kong. Because of the new governmental regulations, over the past 3 weeks the daily number of confirmed cases has dropped significantly to single digits. As of May 7, there are 1,041 confirmed cases but there have been only four deaths. Further, 932 patients have recovered and only 105 are now hospitalized. We have had no new local cases for 17 days.
Surgeons should pay more attention to earlier reopening of their refractive surgery center rather than their cataract surgery center.
Although there is light at the end of the tunnel, we must not let our guard down. This virus is very infectious. We may need to wear masks for a long time—at least until there is an effective vaccine.
Questions to Ask Patients
In the past 14 days, have you:
- Experienced any symptoms such as fever/coughing/sore throat/shortness of breath/breathing difficulties?
- Traveled outside Hong Kong?
- Had any family members travel to countries or areas outside Hong Kong?
- Been in close contact with confirmed cases under medical surveillance?
- Or your family members attended any events with confirmed case clusters, such as a wedding banquet or other large gathering?
1. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med. 2020;172(9):577-582.
2. Coronavirus incubation period could be 27 days, shows data. February 23, 2020. Pharmaceutical Technology. https://www.pharmaceutical-technology.com/news/coronavirus-incubation-period-27-days/. Accessed May 8, 2020.
3. Coronavirus disease (COVID-19) in HK. https://chp-dashboard.geodata.gov.hk/covid-19/en.html. Accessed May 8, 2020.
Practice Restart
By Oliver Findl, MD, MBA

Austria is a relatively small country with fewer than 9 million inhabitants. At the time of this writing, the nation’s Federal Ministry for Social Affairs, Health, Care, and Consumer Protection is meeting to develop a uniform approach to the slow resumption of surgical care across the country. The ministry is and will continue monitoring statistics on COVID-19 cases. An increase in infections may prompt a halt or reversal of the reopening of health care practices and possibly other businesses.
At this juncture, it is worth looking at how the pandemic has affected eye care in Austria thus far and what the immediate future holds.
THE SHUTDOWN
At the time of this writing, Austria is emerging from an approximately 5-week shutdown. All elective surgery was cancelled. Intravitreal injections were halted for 1 week; when they recommenced, at the usual rate, we began administering the injections at a satellite clinic to reserve the hospital setting for COVID-19 patients.
To minimize the risk of infection, hospital staff were split into three teams that rotated in service so that each reported every third day with no overlap.
Austria already had a secure telemedicine service, and health care practitioners have used it quite a lot during the shutdown. At my hospital, one doctor was dedicated to providing this form of care for the entire day.
RAMPING BACK UP
Prioritizing patients. As we entered the slow resumption of eye care services, our hospital staff was consolidated into two teams for the first 2 weeks; now, the entire staff is back to work. Patients whose surgical procedures or visits to the outpatient clinic were cancelled during the shutdown have been divided into four categories of urgency, and their resumption of care is being prioritized according to need. Lid surgery and refractive surgery, for example, will not resume for a long time. Initially, we are limiting cataract surgery to patients who have pronounced lens opacities and poor visual acuity, patients with anisometropia, and those who can no longer legally drive.
We have changed to performing nearly all cataract surgeries as immediate sequential bilateral procedures in order to avoid an additional hospital visit for second eye surgery. We have a strict protocol that all materials used for the second eye surgery must be from a different lot in order to avoid the very small risk of bilateral toxic anterior segment syndrome. The logistics of this are quite cumbersome but doable. (Editor’s note: for more on immediate sequential bilateral cataract surgery, see the article on pg 72.)
Ideally, patients undergoing ophthalmic surgery in this time of uncertainty will be 70 years or younger because they seem to be at lower risk of serious complications or death from COVID-19. We will not recommence providing strabismus surgery for quite a while because it typically requires general anesthesia, which can depress the immune system and make patients more vulnerable if they contract the virus.
Before their preoperative assessments, patients complete a checklist of questions about coronavirus symptoms via telephone. They undergo a swab test for the virus 2 days before their scheduled procedure, and they are asked to stay at home during that time. We receive the result of the test 12 to 24 hours after it is submitted to the laboratory. If the result is positive, we advise the patient to remain at home and call the state for instructions.
Safety measures. Visits to our outpatient clinic began about 2 weeks after we reopened two ORs. Before reopening my practice, we instituted several safety precautions, including addition of plexiglass shields to all slit lamps and at the front counter. All staff members and patients wear masks.
We send patients information prior to their visit that instructs them to return home immediately after their appointment and to call a state telephone number to be tested for COVID-19 if they have any of the following symptoms: fever, cough, or loss of the ability to taste or smell. Before entering the practice, patients must disinfect their hands with the disinfecting agent that is available just outside the office. A staff member takes their temperature with a noncontact thermometer before they are permitted to sit down in the waiting room, where chairs have been spaced at least 1.5 meters apart.
All reading material and the coffee bar were removed from the waiting area, but bottled beverages are available. Disinfecting agents have been distributed throughout the office, and surfaces are regularly disinfected. The interval between visits has been extended so that I see only three patients per hour; my usual rate before the COVID-19 outbreak was four or five patients per hour.
CONCLUSION
Returning to practice has required a great deal of additional work, and it is more difficult to comfort patients. But they will adapt, just as we have. They are seeing plexiglass walls at bakeries and other shops, and everyone is wearing masks in public.
Epidemiologists and virologists suggest that changes to ophthalmic practice and beyond will last for many months. We physicians must gear ourselves to a slower pace of fewer patients per hour, which may mean we decide to extend practice hours in order to increase the volume of patients we can see in a day. We must also be selective about which patients to see and probably postpone yearly checkups to accommodate more time for those patients with a greater need for care.
Pandemic Response at the Singapore National Eye Centre
By Jodhbir S. Mehta, BSc (Hons), MBBS, PhD, FRCOphth, FRCS(Ed), FAMS; and Marcus Ang, MBBS, PhD, FRCS(Ed)

The COVID-19 pandemic has undoubtedly been the most challenging situation that many of us have faced during our ophthalmic careers. As of May 29, more than 5.9 million individuals have been infected worldwide, and more than 364,000 have died.1 We both work in Singapore in a tertiary care referral hospital, and our response continues to evolve even at the time of this writing.
Singapore National Eye Centre (SNEC) is located within the Singhealth academic campus, which includes the Duke-NUS Medical School, Singapore General Hospital, and several national specialist and research institutes. SNEC also has five satellite units around the country. We see a mixture of public and private patients, and we run 14 ORs.
The first case of COVID-19 in Singapore was reported in late January. Most of the cases in the first wave in Singapore were traced to individuals traveling from Wuhan, China, or their close contacts. These cases were monitored, but there was little effect on our working schedule. By the end of January, however, Singapore experienced a second wave of the outbreak, caused mainly by community spread.
PRECAUTION IN PLACE
SNEC had many precautions already in place as result of the SARS outbreak in 2002 and 2003. We immediately implemented single entry through the main entrance of our facility and performed a temperature check on everyone who entered the building (Figure 3). Further, all patients had to answer a questionnaire about travel history, especially to China and Korea, and known contact with people who had traveled there.

Figure 3. A temperature screening and triage area is set up at the main entrance of SNEC.
A COVID-19 task force comprising department heads and senior doctors was established. All doctors were stationed on a single site run by SNEC, and no travel was allowed between sites. We deferred all elective surgery bookings for 2 months but continued operating to clear our waiting lists. All SNEC staff had twice-daily temperature checks that were recorded online.
In February, our clinic numbers dropped by 20% to 40%. General clinics were affected more so than speciality clinics. Patients were informed that there were delayed times in the hospital due to the increased health checks we had put in place.
CHANGING PRIORITIES
Between February and March, there was a slow but steady rise of COVID-19 cases in the community. By mid-March, the rise was exponential enough to indicate our third wave. This time, the source was mainly people coming back to Singapore from overseas—particularly from the United States and Europe. At this point, our priorities changed to protecting our staff and patients, educating the public, providing emergency eye care services, and contributing to the national effort to curb the outbreak.
Protecting the staff. Under our current protocols, all SNEC medical and nonmedical staff wear masks at all times, and N95 masks are worn any time that full PPE is required. Breath shields and disinfectants are placed at all slit lamps (Figure 4), and we try to avoid long consultations with patients near the slit lamp. We are trying to avoid direct ophthalmoscopy and portable slit-lamp examination, but when either must be performed we wear full PPE.
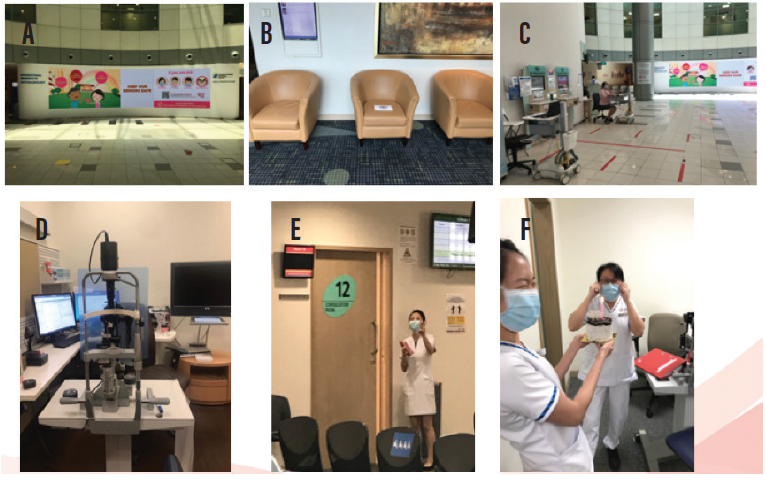
Figure 4. New safety measures at SNEC include: signage in the main foyer alerting patients to COVID-19 guidelines (A), thinning out chairs in the waiting room (B), patient triage area in the foyer (C), installation of slit-lamp shields (D), color-coded examination rooms (E), and staff wearing masks at all times (F).
For surgery, we pool lists so that all general anesthesia cases are done in one OR because these have a higher risk of COVID-19 transmission. The anesthetist and all assisting nursing staff must wear full PPE during intubation and extubation. Due to the air circulation, we wait 15 to 20 minutes after intubation before entering the OR (Figure 4). Patients suspected of being COVID-19–positive are seen in a separate isolation area.
Protecting patients. Text messages describing our safety measures and handwashing etiquette are sent to patients ahead of their appointments. We also communicate that our patients’ eye care will not be compromised during this time, even if they have seen another doctor.
Strict social distancing measures are followed within the hospital. We advise patients either to come by themselves or to bring only one caregiver in order to limit the number of people in the hospital. A mobile clinic reception check-in station is used to avoid queues and overcrowding. A large information screen in the foyer explains the safe distancing measures we are taking with respect to clinic seating. Half of the chairs have been removed from our waiting rooms to increase social distancing.
Patients’ prescriptions are sent to their homes to avoid building up pharmacy queues (Figure 5). We have stopped all clinical research to reduce the number of patients coming to the hospital.
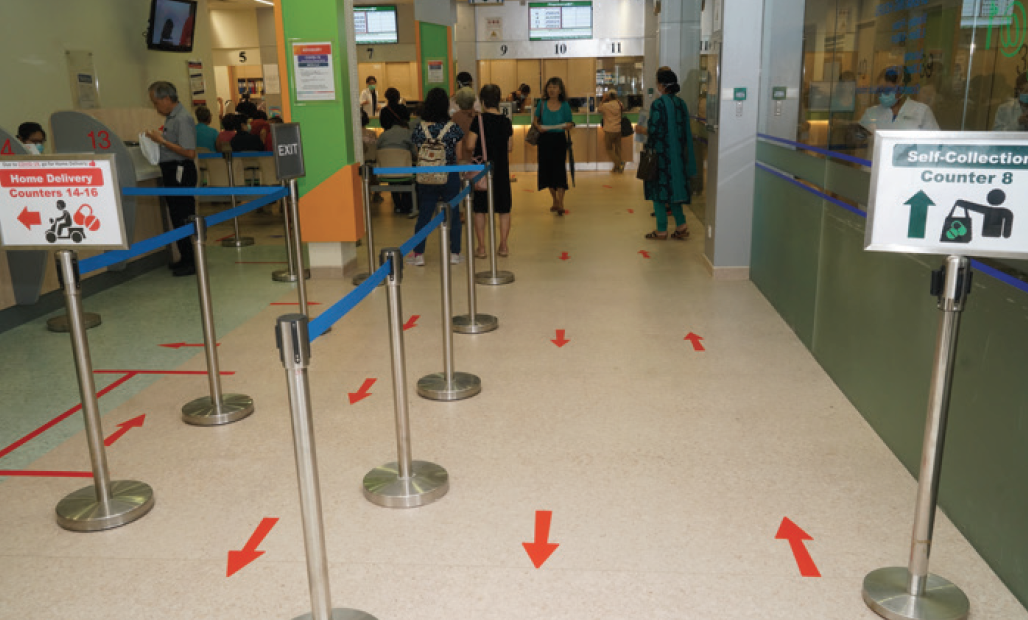
Figure 5. Home delivery of prescriptions to thousands of patients has drastically reduced the numbers of patients waiting in the SNEC pharmacy.
Contributing to national efforts. Many SNEC nurses, researchers, and doctors have been deployed to other hospitals or care facilities or to work in the fever-screening area. In this area, patients suspected to have COVID-19 are examined, a nasopharyngeal swab is taken, and a chest x-ray is performed. Depending on their medical conditions, patients are sent to one of three areas for further follow-up.
WHAT NOW?
We recently entered our fourth wave of the COVID-19 outbreak (Figure 6). At this time, most cases come from the foreign workers in Singapore. We now have more than 5,000 confirmed cases, and the country is enforcing a lockdown or circuit-breaker to control the escalating situation.
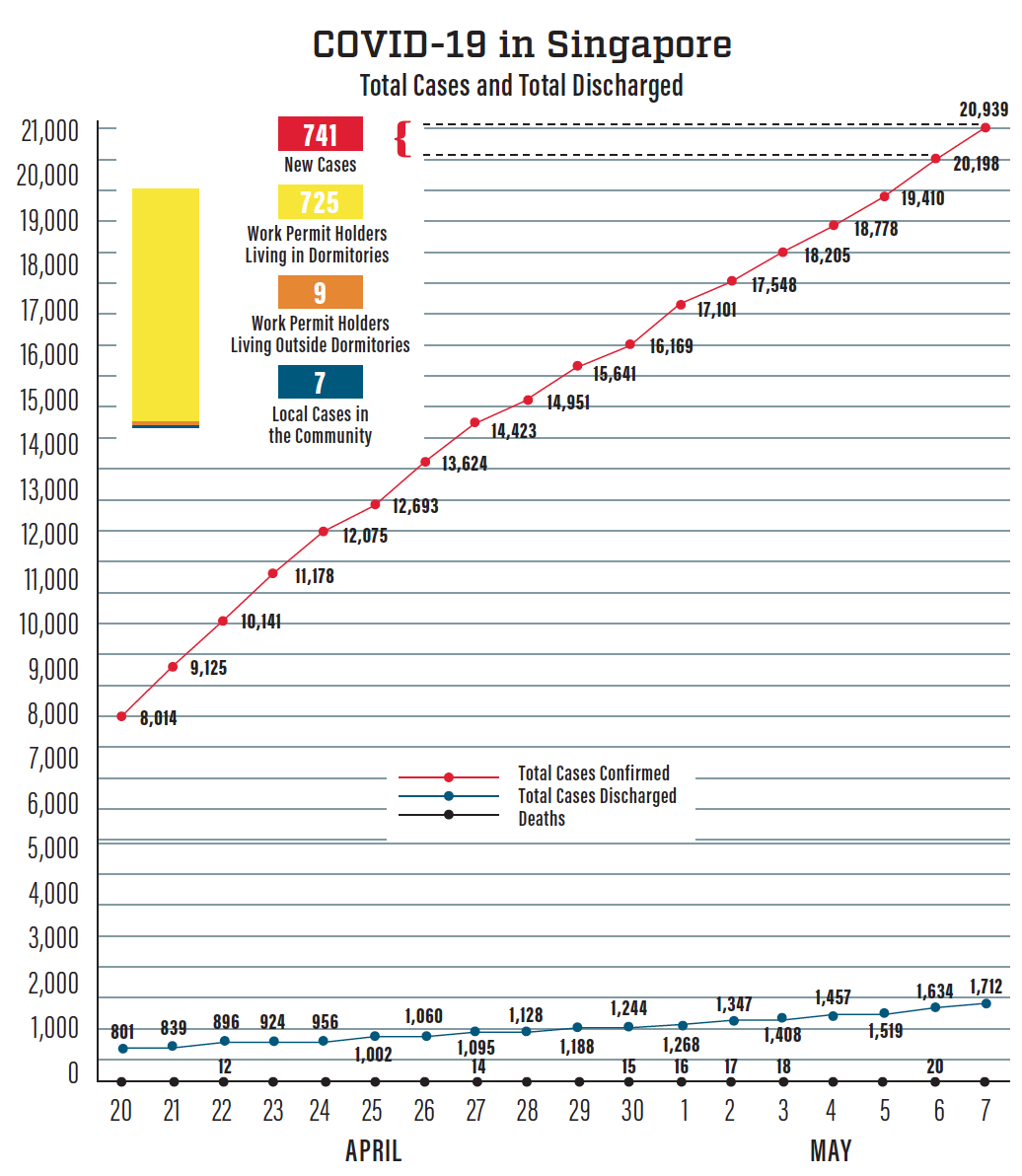
Figure 6. Total number of COVID-19 cases in Singapore. Source: Ministry of Health. May 7, 2020.
Figures 3-6 courtesy of Jodhbir S. Mehta, BSc (Hons), MBBS, PhD, FRCOphth, FRCS(Ed), FAMS
In our hospital, we immediately cut the workload to 10% of our normal clinic volume. Each doctor assesses the urgency of his or her appointments. Most patient appointments are delayed by up to a month or longer if possible. Staff members call patients to notify them of changes in appointments, to ensure that they have adequate medication, and to provide reassurance that a doctor reviewed their file to make the delay decision.
A convention center has been converted to a hospital to house medically stable COVID-19 patients, and again SNEC staff members were deployed to help battle the infection. At SNEC, we are working on a split-team system to reduce the risk of spreading the infection to other speciality teams.
We are still in lockdown, but restrictions on some services should be lifted in the coming weeks. For now, we are treating only emergent and urgent cases. We spend 1 week at SNEC and the next at the makeshift hospital in the convention center.
We continue to hold weekly journal clubs and lab meeting updates via Zoom (Zoom Video Communications). There are now high numbers of Zoom meetings, sometimes five per day. We also have weekly SNEC task force meetings, but our weekly speciality faculty online courses are temporarily paused during the lockdown. Many new models for dissemination are being explored, as we hope to come out of this period soon. Nevertheless, security of online information sharing is paramount, especially when patient data are discussed.
Only one SNEC staff member contracted COVID-19, and luckily that person has recovered.
We have had a lot of contact with colleagues in other countries, especially Italy, where we sent some PPE to help with that country’s shortage. We also authored an editorial published in Ophthalmology on preparedness among ophthalmologists.2 A particularly useful part of the editorial was a table showing what measures are being taken by ophthalmologists themselves and also for patients from nine centers around the world.
CONCLUSION
After lockdown, we plan to further change the way we practice. We are exploring more ways to reduce patients’ time in the hospital. We will be transitioning to video consultations for certain visits. And we are fast-tracking and expanding some ongoing initiatives such as virtual clinics, especially in our glaucoma and retina services.
We hope to resume elective cataract surgery at the end of lockdown because the risk of aerosol transmission of the virus with this procedure is small. Some higher-risk procedures such as oculoplastic surgery and general anesthesia cases will undergo more stringent assessments.
At the time of this writing, there have been more than 20,000 confirmed COVID-19 cases in Singapore. Fortunately, there have been only 20 deaths. One thing is for sure: The way we practice medicine will change as a result of this experience, and we are hopeful that some of the changes will be for the better for our specialty.
1. Corona Help. https://corona.help. Accessed May 29, 2020.
2. Olivia Li JP, Shantha J, Wong TY, et al. Preparedness among ophthalmologists: During and beyond the COVID-19 pandemic. Ophthalmology. 2020;127(5):569-572.




