In its Medicare Physician Fee Schedule Final Rule for 2023, CMS rejected a proposal to make facility payments for office-based ophthalmic surgeries. The following is a summary of this and other key points in the ruling.
Office-based payments. In response to requests to create an office-based payment for cataract surgery, MIGS, vitrectomy, and other ocular surgery procedures, CMS stated it heard concerns about the services’ being furnished in nonfacility settings. The CMS Final Rule stated, “We appreciate commenters’ perspectives regarding their experience and concerns for Cataract and Retinal Surgeries being furnished as office-based surgery (OBS). As we continue to consider how and where these services are furnished, and whether they are typically furnished in different settings, information such as the comments provided by these and other commenters are [sic] helpful. Based upon commenters’ feedback, we have concerns about these services being furnished in nonfacility settings. It is also unclear whether these services are routinely being furnished outside of facility settings. CMS will continue to evaluate whether these services are being furnished in nonfacility settings and will consider establishing nonfacility values for these services at that time.”1
The Outpatient Ophthalmic Surgery Society (OOSS) submitted comments to CMS objecting to office-based cataract surgery reimbursement and expressed support for the CMS Final Rule. OOSS called it a “victory for our patients and our [ambulatory surgery centers (ASCs)].”
In a separate news release, iOR Partners, a developer and manager of office-based suites, stated that it remains hopeful CMS will consider establishing nonfacility codes in the future: “The OBS movement achieved a key milestone as CMS recognized OBS as an alternative option for cataract, glaucoma, and retinal eye surgeries with its inclusion in the 2023 proposed rule. Most importantly, the agency stated in the final rule that they will continue to evaluate these procedures in the nonfacility setting and consider establishing nonfacility codes in the future. … Changes in health care take time. The movement toward OBS may be long and arduous, but it is in motion and accelerating. The magnitude of supportive comments collected by CMS indicates that change is happening.”
iOR Partners operates more than 80 office-based suites in the United States and said it will continue to advocate for CMS to develop a consensus-driven plan to provide payment for ophthalmic OBS procedures with key stakeholders.
Conversion factor. CMS’ Physician Fee Schedule Final Rule also calls for the conversion factor—used to determine provider reimbursement in traditional Medicare—to drop to $33.06, or 4.47% from the $34.61 factor for 2022. In a news release, CMS said the conversion factor decrease accounts for budget neutrality adjustments required by law, which will be 0% next year, and the expiration of the 3% supplemental increase to physician fee schedule payments.
Payment rate regulation. CMS also issued its final 2023 payment rate regulation for hospital outpatient departments and ASCs. Under the final rule, ASC payment rates will be updated by 3.8% in 2023 based on the projected hospital market basket percentage increase of 4.1%. This is reduced by 0.3% for productivity adjustment.
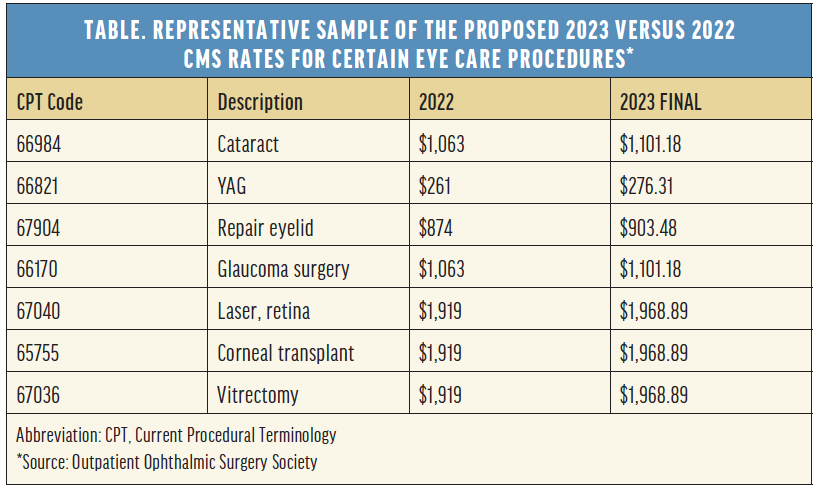
According to OOSS, CMS previously agreed that, for the period of 2019 to 2023, it would update ASC payment rates by the Hospital Market Basket rather than the Consumer Price Index-Urban. Under the policy, ASCs have received the same updates as hospitals, subject to certain adjustments. OOSS, which lobbied for the change to the Hospital Market Basket method, provided a representative sample of the proposed rates for various eye care procedures and how they compare to 2022 (see Table). Overall, the CMS payment rate policies will affect approximately 3,500 hospitals and 6,000 ASCs. According to OOSS, other parts of the CMS Final ASC Payment Rule include the following:
- The mandatory adoption of ASC-11, Cataracts: Improvement in Patient’s Visual Function within 90 Days Following Cataract Surgery will be suspended;
- Omidria (phenylephrine and ketorolac intraocular solution 1%/0.3%, Rayner) and Dextenza (dexamethasone ophthalmic insert 0.4 mg, Ocular Therapeutix) will continue to be paid for separately in the ASC under the agency’s nonopioid pain management program; and
- ASCs that implant lenses that have secured new technology IOL status will receive an additional $50 in facility reimbursement.
1. Department of Health and Human Services, CMS. Accessed November 4, 2022. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.cms.gov/files/




