Conjunctivochalsis (CCh) is a common but frequently overlooked and poorly managed age-related condition that can cause degenerative changes in the Tenon capsule that can lead to decreased adhesion between the bulbar conjunctiva, Tenon capsule, and underlying sclera.1 CCh typically occurs bilaterally but can present asymmetrically. Patients with hypermetropia and blepharitis are at increased risk of developing CCh. This article describes a new option for treatment.
Diagnosing CCh
Symptoms of CCh include dry eye; ocular surface inflammation; foreign body sensation; subconjunctival bleeding; eye pain; blurry vision, especially on downward gaze; watering eyes; ocular fatigue and pain; frequent blinking; and decreased tear film break-up time. Unlike with aqueous-deficient dry eye disease, patients with CCh more often experience dryness in the morning.
Staining the ocular surface with fluorescein or lissamine green dye can help to detect the presence of redundant inferior conjunctival folds between the ocular surface and lid margin, which indicate CCh. I have also had success with a diluted solution of sterile gentian violet with topical anesthesia (Figure 1). Corneal staining associated with CCh occurs in an unexposed area of the conjunctiva rather than in the interpalpebral pattern associated with aqueous-deficient dry eye disease.

Figure 1. Lid-parallel conjunctival folds of CCh stained with diluted gentian violet.
Patient Selection
Dye-enhanced laser conjunctivoplasty is an option for patients with mild to moderate symptomatic CCh, especially those who are elderly and those who desire a minimally invasive and cost-effective treatment. The patient should also be informed of other available treatments, including surgical excision and thermocautery, and the possible complications associated with them such as scarring, shortening of the inferior conjunctival fornix, and lid margin entropion.
Treatment Protocol and Efficacy
Methodology. I analyzed the results of dye-enhanced laser conjunctivoplasty in 36 patients—21 men and 15 women—with CCh (unpublished data, 2020–2021). Patients with pterygium, eyelid abnormalities, autoimmune diseases, or a history of eye surgery were excluded.
The procedure. Topical anesthesia was administered to increase patient comfort during the procedure. Gentian violet dye was used to stain the conjunctiva to reveal the loose redundant conjunctival folds. (Stained areas have a stronger response to laser treatment than do unstained areas.2) After laser treatment, an additional amount of gentian violet was instilled.
Specifically, a topical anesthetic (3.5 mL of proparacaine HCl 5 mg/mL) was mixed with 1.5 mL of 0.5% (w/v) sterile gentian violet solution and applied to the target conjunctival surface. The dye was allowed to dry and stain the conjunctival surface for 60 seconds.
At the slit lamp, 10x magnification was used. The following settings were selected on a Viridis argon laser (Quantel Medical): power, 800 to 1,200 mW; spot size, 300 μm; duration, 0.1 milliseconds; and aiming beam intensity, 3. A base-up triangular laser pattern was used initially (Figure 2), followed by a base-down triangular laser pattern. Laser energy was directed at the inferior perilimbal conjunctiva 1 mm away from the limbus from the 4 to 8 clock positions.
Figure 2. A base-up triangular laser pattern.
Results. Three months after treatment, 35 of 36 patients (97%) exhibited a visible reduction of CCh. Complete relief of symptoms was experienced by 34 of 36 patients (89%). Two patients (11%) experienced moderate relief of symptoms and were offered retreatment, but both declined for personal reasons.
Figures 3 and 4 show the results of the study.
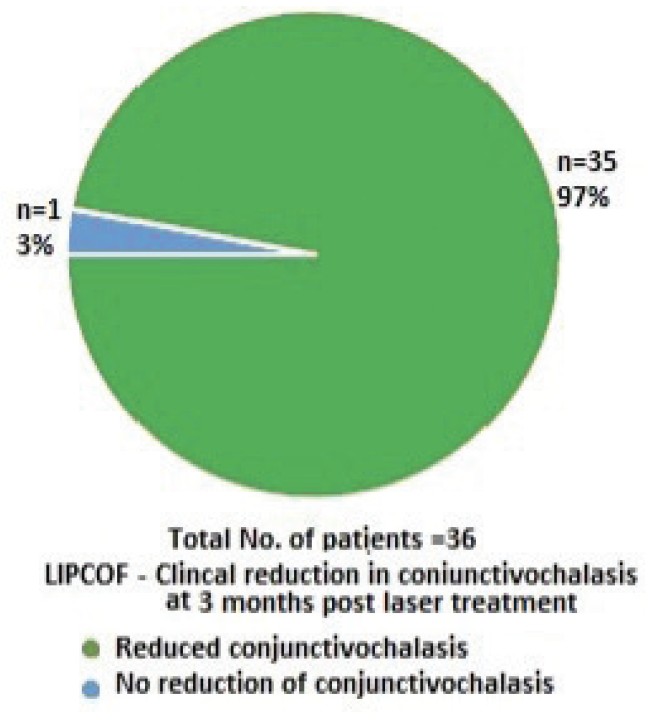
Figure 3. Visible reduction in CCh at 3 months after treatment.
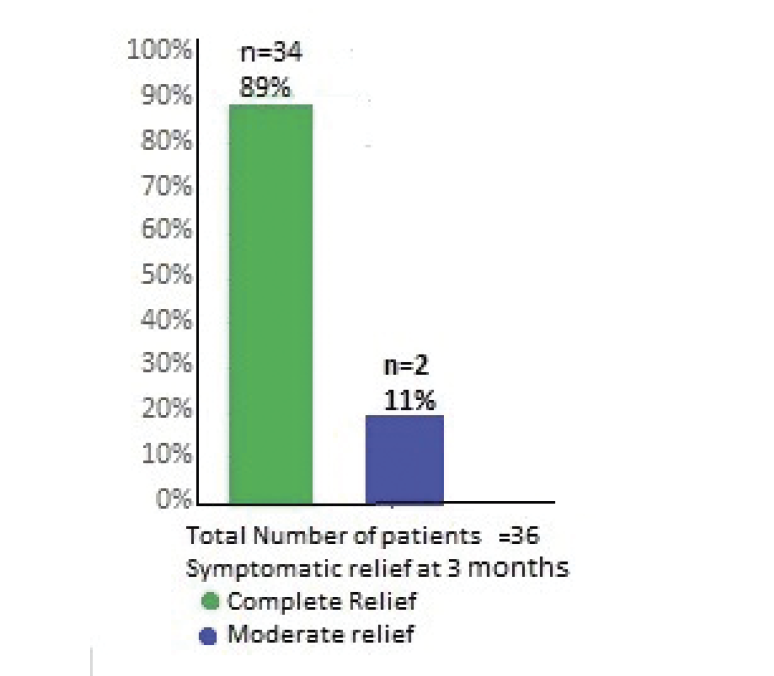
Figure 4. Symptomatic relief after dye-enhanced laser conjunctivoplasty.
Management and Follow-up
After dye-enhanced laser conjunctivoplasty, patients may experience mild irritation, conjunctival congestion or swelling, and foreign body sensation. They should avoid exposure to dust, smoke, and fumes for 4 weeks to prevent contamination of the laser-treated conjunctival surface.
I recommend a postoperative regimen that typically includes four agents.
No. 1. A steroid eye drop (fluorometholone ophthalmic suspension 0.1% [FML, Allergan]) instilled every 8 hours for 2 weeks to reduce inflammation and the associated discomfort and pain.
No. 2. Lubricating eye drops (Systane, Alcon) administered every 6 hours for 4 weeks to alleviate any gritty sensation and lubricate the ocular surface.
No. 3. Decongestant eye drops (phenylephrine hydrochloride 1.2 mg/mL [Prefrin, Allergan]) instilled every 8 hours for 2 weeks to minimize conjunctival congestion.
No. 4. Moxifloxacin ophthalmic solution 5 mg/mL (Vigamox, Alcon) administered every 6 hours for 2 weeks to prevent infection of the raw, laser-treated conjunctival surface.
Patients return for a follow-up appointment at 2 weeks and a final consultation at 6 weeks to assess their clinical and symptomatic improvement.
Advantages of Laser Conjunctivoplasty
Dye-enhanced laser conjunctivoplasty can be performed under topical anesthesia as an office-based procedure. Compared with alternatives such as surgical resection and repair of the redundant conjunctiva, laser conjunctivoplasty appears, in my experience, to provide better adhesion between the loose conjunctiva and the underlying Tenon capsule.
The equipment and materials for the procedure are available in most eye care facilities. Treatment can be repeated. It is also cost effective.
Conclusion
Dye-enhanced argon laser conjunctivoplasty can reinforce the conjunctival adhesion to the sub-Tenon capsule and sclera and reduce or eliminate conjunctival laxity. This procedure appears to be safe and effective for the treatment of mild to moderate symptomatic CCh.3-7
1. Balci O. Clinical characteristics of patients with conjunctivochalasis. Clin Ophthalmol. 2014;8:1655-1660.
2. Parul S, Kumar H, Neelam P. Treatment of overhanging blebs with frequency-doubled Nd:YAG laser. Ophthalmic Surg Lasers Imaging. 2004;35(5):429-432.
3. Yang HS, Choi S. New approach for conjunctivochalasis using an argon green laser. Cornea. 2013;32(5):574-578.
4. Shin KH, Hwang JH, Kwon JW. Argon laser photoablation of superficial conjunctival nevus: results of a 3-year study. Am J Ophthalmol. 2013;155:823-828.
5. Shin KH, Hwang JH, Kwon JW. New approach for conjunctivochalasis with argon laser photocoagulation. Can J Ophthalmol. 2012;47:380-382.
6. Kashima T, Akiyama H, Miura F, Kishi S. Improved subjective symptoms of conjunctivochalasis using bipolar diathermy method for conjunctival shrinkage. Clin Ophthalmol. 2011;5:1391-1396.
7. Kwon JW, Jeoung JW, Kim Tl, Lee JH, Wee WR. Argon laser photoablation of conjunctival pigmented nevus. Am J Ophthalmol. 2006;141:383-386.




