Much like death and taxes, presbyopia is one of life’s unfortunate certainties. An estimated 2 billion individuals worldwide have presbyopia.1 The management of presbyopia is therefore an exciting challenge for refractive surgeons because of the growing demand for both invasive and noninvasive treatments.
Many options are available for the treatment of lens dysfunction, including spectacles, multifocal contact lenses, topical presbyopia drops, laser vision correction, corneal inlays, and refractive lens exchange (RLE). Additionally, more presbyopia drops are coming to market. The success of any presbyopia treatment, however, depends heavily on managing patient expectations and choosing the safest procedure with the least amount of compromise for each individual. When selecting a procedure, it is important to consider the patient’s occupation, hobbies, driving habits, and visual expectations.
Ideally, surgeons should be well versed in a variety of procedures and customize their selection based on the patient’s needs and lifestyle.2
TREATMENT OPTIONS
People typically begin to experience the effects of presbyopia at 40 to 50 years of age. In the condition’s early stages, the lens is clear and has some accommodative amplitude. In our practice, a corneal approach to pseudoaccomodation is the most popular option for these patients.
Presbyopic laser vision correction. We have achieved favorable results with PresbyMax (Schwind eye-tech-solutions), which creates a multifocal ablation profile that incorporates predicted postoperative results for far and near vision. A bispheric ablation is mathematically optimized to allow adequate transmission of vision. We choose between one of three treatments: PresbyMax Monocular, which provides good distance vision with the least compromise; PresbyMax Hybrid, which provides rapid visual recovery and good vision at all distances; and PresbMax µ-Monovision, which optimizes near vision.
PresbyMax Monocular is the most popular ablation profile because it causes the least compromise in distance and intermediate vision, the latter of which is essential in our digital age. When a monovision profile is used, a common complaint that patients have is blurry intermediate or computer vision. Those who experience minimal interocular suppression of blur and those with large esophoric shifts are poor candidates for monovision. Contrast sensitivity is reduced with monovision, and patients who engage in fine near work may experience difficulty.3
THE THREE STAGES OF NEURAL ADAPTATION
Stage No. 1: Conflict. This stage lasts between 1 week and 1 month. The brain perceives a difference between the near and intermediate ranges of vision in one eye and the intermediate and distance ranges of vision in the fellow eye. Some patients experience blurry vision and are unhappy. Others do not experience this side effect. I advise patients that it is not unusual for them to think they have made the wrong decision 2 weeks after the procedure.
Stage No. 2: Neutrality. This stage can last between 1 week and 1 month. Patients may notice a difference in vision between their eyes but typically do not report blurring due to conflict (stage No. 1).
Stage No. 3: Blended vision. Binocular summation occurs by 3 months after surgery. At this stage, patients enjoy a full range of vision without perceiving differences between the vision of their right and left eyes. Both distance and near vision are clear.
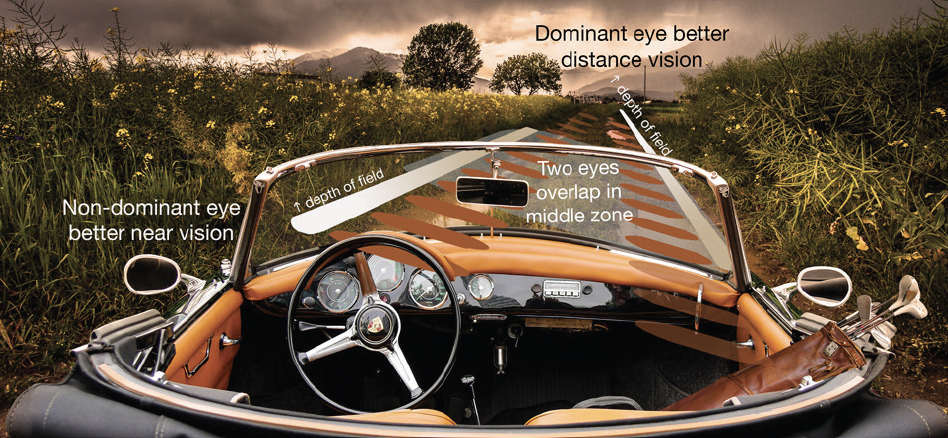
Figure. A visual aid can help patients understand presbyopic laser vision correction and neural adaptation.
We customize the ablation profile to the patient’s needs and age but warn them that an enhancement of the addition may be required in the future. Summation takes place when the difference in refraction between the eyes is no more than 1.50 D.4 The patient’s tolerance of the induced anisometropia should be evaluated with a cross blur or tolerance test using a 1.50 D retinoscopy lens within the phoroptor. A thorough explanation of the three stages of neural adaptation is crucial (Figure; also see The Three Stages of Neural Adaptation).
Refractive lens exchange. The goal of this procedure is to restore clear vision while maintaining spectacle independence. RLE is usually reserved for young individuals who have clear lenses but are poor candidates for laser vision correction. Patients with corneal pathologies such as narrow angles or early lenticular changes may not be suitable candidates for laser vision correction. Other unsuitable patients include those whose ametropia is beyond the capability of the laser. We use the HD Analyzer (Visiometrics) to assess ocular scatter and the modular transfer function to determine the presence of lenticular changes. The Vivior Monitor (Vivior) assists with IOL selection. This technology is worn by patients for about 48 hours and combines data on the user’s visual behavior (ie, preferable viewing distances and light intensities during daily activities) and matches them with objective lens data and IOL defocus curves.
Nondiffractive extended depth of focus IOLs such as the AcrySof IQ Vivity (Alcon) and Acunex Vario (Teleon Surgical) provide a near add of around 1.50 D and can be used for blended vision. When we use a mix-and-match approach, we like to implant the Acunex Vario in the dominant eye and the Acunex Vario Max in the nondominant eye. Alternatively, a trifocal IOL can be selected to match to the patient’s unique defocus curve.
Patients typically experience a wow phase during the first week after surgery. They then enter a critical phase, during which they focus on the shortcomings of the IOL and visual sacrifices, before progressing to the final adaptation and acceptance phase.
Corneal inlays. There are three types of corneal inlays: reshaping, refractive, and small aperture. The Raindrop Near Vision Inlay, a reshaping transparent hydrogel implant, was recalled in 2018 owing to an increased risk of corneal haze. The Kamra small-aperture inlay (CorneaGen) was found to be safe and effective. Unlike monovision, corneal inlays do not adversely affect distance visual acuity, but they may reduce night vision and contrast sensitivity. Any foreign material inside the cornea can lead to haze formation, which has implications for the use of synthetic corneal inlays. The development of an allogenic inlay (Allotex) may therefore make inlays a more attractive option for presbyopia correction.
Pharmacologic treatment. The use of presbyopia drops to induce temporary miosis is gaining momentum. Vuity (pilocarpine HCl ophthalmic solution 1.25%, Allergan) is the first FDA-approved eye drop for the treatment of presbyopia. The drop is instilled once a day binocularly or monocularly (to mimic monovision) to induce pupillary constriction and provide up to 5 hours of near vision improvement. The onset of action is 15 minutes. Side effects include headache, conjunctival hyperemia, and dim night vision. Fixed combinations of pilocarpine and NSAIDs5 and 0.2% brimonidine and carbachol6 are being studied, as are lens-softening topical agents such as a lipoic acid, an antioxidant that chemically reduces the disulphide bonds in the lens improving the dynamic refractive power.7
Pharmacologic treatment can allow patients to avoid wearing spectacles and contact lenses or undergoing surgery. The duration of effect of these agents, however, is temporary, and long-term application can be costly. There is also a risk of systemic and ophthalmic adverse events. Areas of interest include increasing the duration of effect and decreasing the drugs’ effects on distance vision, night vision, and the ocular surface.
Phakic IOLs. Patients with hyperopia, myopia, astigmatism, keratoconus, and a history of corneal transplantation can be good candidates for phakic IOLs,3 as can individuals who are poor candidates for laser vision correction. Correcting presbyopia with phakic IOLs avoids the potential vitreoretinal alterations associated with conventional RLE. Postoperative visual recovery is quick, and the procedure can be reversed should the patient not tolerate their visual outcome.
CONCLUSION
Many options are available for the treatment of presbyopia, and matching the technology to a patient’s particular visual needs can be challenging. Identifying the most effective treatment requires listening to their needs and managing their expectations. A thorough assessment of eye health and patient lifestyle is crucial.8
Applying a personalized approach to presbyopia correction has never been more important than it is today, as we all continue to navigate the COVID-19 world in front of our computers and cell phones.
1. Reinstein D, G Carp, T Archer, M Gobbe. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg. 2012;28(8):531-541.
2. Azar D. Monovision. In: Azar D, Gatinel D, Ghanem R, Taneri S, eds. Refractive Surgery. Elsevier; 2020.
3. Schmid R, Luedtke H. A novel concept of correcting presbyopia: first clinical results with a phakic diffractive intraocular lens. Clin Ophthalmol. 2020;14:2011-2019.
4. Azen SP, R Varma, S Preston-Martin, M Ying Lai, D Globe, S Hahn. Binocular visual acuity summation and inhibition in an ocular epidemiological study: the Los Angeles Latino Eye Study. Invest Ophthtalmol Vis Sci. 2002;43(6):1742-1748.
5. Benozzi G, Perez C, Leiro J, Facal S, Orman B. Presbyopia treatment with eye drops: an eight year retrospective study. Trans Vis Sci Tech. 2020;9(7):25.
6. Abdelkader A. Influence of different concentrations of carbachol drops on the outcome of presbyopia treatment – a randomized study. Int J Ophthalmic Res. 2019;5(1):317-320.
7. Korenfeld MS, Robertson SM, Stein JM, et al. Topical lipoic acid choline ester eye drop for improvement of near visual acuity in subjects with presbyopia: a safety and preliminary efficacy trial. Eye. 2021;35:3292-3301.
8. Mercer RN, Milliken CM, Waring GO IV, Rocha KM. Future trends in presbyopia correction. J Refract Surg. 2021;37(S1):S28-S30.