Posterior capsular opacification (PCO) is the most common complication of cataract surgery, developing in approximately 50% of eyes by 5 years after cataract surgery.1,2 Nd:YAG laser posterior capsulotomy is the standard treatment for symptomatic PCO and is the second most frequently performed procedure, after cataract extraction, in Medicare beneficiaries.3 One long-term, all-age, US population-based study found that the cumulative probability of Nd:YAG laser posterior capsulotomy after cataract extraction was 38% at 9 years after the initial procedure.4 Although it is generally accepted that laser discission of the capsule improves visual acuity, glare disability, and contrast sensitivity, the incidence of postlaser complications and their relationship to capsulotomy size and total laser energy application are unclear.5
One of the most potentially serious complications of posterior capsulotomy is retinal detachment (RD). One report noted an incidence of RD of 1.4% after laser capsulotomy.6 Another found that RD occurred in eyes after laser capsulotomy with 3.8 times greater frequency than in eyes that had not undergone capsulotomy.7
Data comparing the risk of RD with capsulotomy size are limited. The literature contains claims that larger capsulotomy size and greater total laser energy increase the risk of IOL movement, iritis, rise of IOP, cystoid macular edema (CME), and RD, and authors have advised performing smaller capsulotomies to minimize the energy used to create the capsulotomy, thereby presumably minimizing the associated risk.8,9
One study recommended a capsulotomy size of approximately 2 to 3 mm diameter,10 as did another that reported that a capsulotomy of at least 1.5 mm in diameter provided satisfactory visual performance.11 Yet another study concluded that a cruciate-shaped capsulotomy with an opening of 3.5 mm or less provided the greatest improvement in visual function with minimal complications.2 This retrospective study specified neither the nature of the complications nor the duration of any associated symptoms.
We have seen several patients with symptoms of glare that developed after Nd:YAG capsulotomy with openings of 2 to 3 mm diameter; their symptoms were eliminated by enlargement of the capsulotomy to approximately 5 mm, and we have routinely performed Nd:YAG laser posterior capsulotomies of approximately 5 mm for more than 20 years (Figure 1).
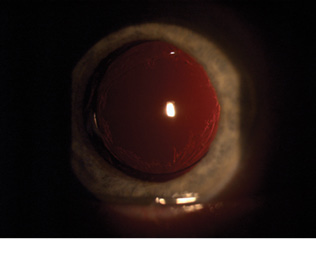
Figure 1. Capsulotomy with a diameter of 5 mm.
RECORD REVIEW
We performed a retrospective analysis of the medical records of patients in whom we performed cataract surgery and subsequent Nd:YAG posterior capsulotomy, with the latter procedure done between January 2013 and December 2015 (unpublished data). Of 180 records reviewed, 108 eyes (87 patients) had a least 1 year (mean, 21.9 months) follow-up after capsulotomy. These patients were included in the study, and their medical records were further reviewed.
In all eyes included in the study, a one-piece acrylic IOL had been implanted into an intact capsular sac. One patient was excluded due to preexisting RD at the time of capsulotomy.
All capsulotomies were approximately 5 mm, thereby leaving 0.5 mm of intact posterior capsule beneath the periphery of the 6-mm IOL optic in all eyes. Patients were not given postoperative medications, and routine IOP measurements were not performed on the day of the Nd:YAG procedure.
The patients’ medical records were reviewed to determine the incidences of RD, CME, iritis, IOL dislocation, floaters (transient or persistent), glare, and flashing lights (ie, flashes). Axial lengths of each eye were also noted. Transient floaters were defined as those that began within 24 hours after the procedure and resolved within 1 year. Persistent floaters were defined as those that began within 24 hours after the procedure and remained after 1 year. The incidence of glare symptoms before and after the procedure was compared.
Of the 108 eyes included in the study, follow-up ranged from 12 to 52 months (mean, 21.9 months). Nd:YAG capsulotomy followed cataract surgery by an average of 39.9 months (range, 1–99 months). Analysis of the complications our study revealed is overviewed in Positive Findings.
DISCUSSION
After undergoing Nd:YAG laser posterior capsulotomies of 5 mm diameter, the patients included in our study did not experience an increased incidence of RD, CME, or iritis when compared with rates reported in previous studies, including those in which smaller capsulotomies were created.
RD developed in two of 108 eyes (1.85%); this is comparable to the rates (1.4% and 3.8%) reported in previous studies.6,7 Ambler et al found that 38% of detachments developed in the first 2 months and 69% within the first 6 months after capsulotomy.6 Tielsch et al reported an RD incidence of 3.8%; they used Medicare records and conditional logistic regression models in determining this ratio.7
In two reports,12,13 the incidence of RD after cataract surgery ranged from 0.6% to 1.7% in postoperative year 1, compared with an annual rate of RD in the general population of 0.0065% to 0.0179%. A review by Haug and Bhisitkul13 assessed known risk factors for RD such as younger age, male sex, and greater axial length (AL) and found that an eye with an AL of 23 to 25 mm had an 8-year RD rate of 2.44% after cataract extraction, compared with an RD rate of 6.14% rate in eyes with an AL of 26 mm or greater. Another report found a greater risk of postoperative RD in eyes with a history of previous RD and AL greater than 24 mm.14
POSITIVE FINDINGS
Retinal Detachment
- Developed in two eyes, both occurring by 16 months after capsulotomy
- One of the patients had a history of previous retinal detachment and an axial length of 26.8 mm; the other had an axial length of 25.7 mm
Cystoid Macular Edema
- Developed in one patient 6 months after capsulotomy
Iritis
- No instances
IOL Displacement/Dislocation
- No instances were reported at any follow-up examination after Nd:YAG capsulotomy
Floaters
- Of the 87 patients included, 13 complained of floaters that developed within 24 hours after Nd:YAG laser capsulotomy
- Of these, 11 patients reported that floaters had disappeared by 1 year
- Floater symptoms persisted for at least 1 year in two patients
Glare Symptoms
- Of 27 patients with specific glare complaints before the procedure, 20 no longer complained of glare after the procedure
- Four reported improved glare symptoms
- Three continued to experience significant glare at 1 year after the procedure
Flashes
- No patient complaints at any post-YAG follow-up examination
study findings
In our study, average AL was 24.13 mm (range, 21–27.7 mm). Fifty eyes had an AL greater than 24 mm, 27 had an AL greater than 25 mm, and 18 had an AL greater than 26 mm. Of the two cases of RD seen in our study, both occurred 16 months after the capsulotomy, and one patient (one eye) had a previous history of RD. Both patients were men with an AL greater than 25 mm—factors known to increase the risk of RD after cataract extraction.13 Our RD rate of 1.85% was similar to that reported by Ambler6 and Tielsch7 and similar to that reported after cataract surgery without Nd:YAG laser capsulotomy.
One patient in our study developed CME, but this occurred 6 months after the capsulotomy, an indication that the number of pulses and energy delivered were not factors in this development. No patient developed postoperative iritis, despite the fact that no topical antiinflammatory medications were given.
Fifteen percent of study patients reported new floaters after capsulotomy; however, they persisted in only 2%. There is limited information in the literature concerning the incidence of floaters in relation to Nd:YAG capsulotomy. Some authors have stated that a particular shape, such as a cruciate or hinged capsulotomy, may result in a reduced incidence of floaters; however, the duration of floater symptoms was not mentioned in these reports.2,14
Twenty-three patients (27 eyes) in the study complained of glare before capsulotomy, and, of these, three patients reported persistent glare after the procedure. These results are consistent with a previous report indicating that wider capsulotomies are necessary to improve forward light scatter.15
It appears likely that larger capsulotomies reduce the possibility of postlaser glare symptoms because there is less diffraction of light at the margins of the capsulotomy. Another likely benefit of larger capsulotomies is improved peripheral retinal visualization.11
CONCLUSION
In comparison with previous studies, including those using small (2–3 mm) Nd:YAG laser posterior capsulotomies,6,7,8,9,11,13 large (5-mm) capsulotomies were not associated with increased risk of RD, CME, IOL displacement, iritis, or symptoms such as flashes or persistent floaters.
The risk of postoperative glare symptoms may be reduced and peripheral retinal visualization may be improved when larger rather than smaller capsulotomies are performed.
1. Wormstone IM. Posterior capsule opacification: a cell biological perspective. Exp Eye Res. 2002;74(3):337-347.
2. Cetinkaya S, Cetinkaya YF, Yener HI, Dadaci Z, Ozcimen M, Acir NO. The influence of size and shape of Nd:YAG capsulotomy on visual acuity and refraction. Arq Bras Oftalmol. 2015;78(4):220-223.
3. Schein OD, Katz J, Bass EB, et al. The value of routine preoperative medical testing before cataract surgery. N Engl J Med. 2000;342(3):168-175.
4. Baratz KH, Cook BE, Hodge DO. Probability of Nd:YAG laser capsulotomy after cataract surgery in Olmsted County, Minnesota. Am J Ophthalmol. 2001;131:161-166.
5. Magno BV, Datiles MB, Lasa MSM, Fajardo MRQ, Caruso RC. Kaiser-Kupfer evaluation of visual function following Neodymium:YAG laser posterior capsulotomy. Ophthalmology. 1997;104:1287-1293.
6. Ambler JS, Constable IJ. Retinal detachment following capsulotomy. Aust N Z J Ophthalmol. 1988;16(4):337-341.
7. Tielsch JM, Legro MW, Cassard SD, et al. Risk factors for retinal detachment after cataract surgery: a population-based case-control study. Ophthalmology. 1996;103(10):1537-1545.
8. Javitt JC, Toelsch JM, Canner JK, Kolb MM, Sommer A, Steinberg EP. National outcomes of cataract extraction. Increased risk of retinal complications associated with Nd:YAG laser capsulotomy. Ophthalmology. 1992;99:1487-1498.
9. Karahan E, Er D, Kaynak S. An overview of YAG capsulotomy. Med Hypothesis Discov Innov Ophthalmol. 2014;3(2):45-50.
10. Charles S. Vitreoretinal complications of YAG laser capsulotomy. Ophthalmol Clin North Am. 2001;14(4):705-710.
11. Patton N, Aslam TM, Bennett HG, Dhillon B. Does a small central Nd:YAG posterior capsulotomy improve peripheral fundal visualization for the vitreoretinal surgeon? BMC Ophthalmology. 2004;4(8).
12. Aslam T, Dhillon B. Neodymium:YAG capsulotomy: a clinical morphological analysis. Graefes Arch Clin Exp Ophthalmol. 2002;240(12):972-976.
13. Haug SJ, Bhisitkul RB. Risk factors for retinal detachment following cataract surgery. Curr Opin Ophthalmol. 2012;23:7-11.
14. Lewis H, Singer TR, Hanscom TA, Straatsma BR. A prospective study of cystoid macular edema after neodymium:YAG laser posterior capsulotomy. Ophthalmology. 1987;94(5):478-482.
15. Alipour F, Jabbaryand M, Hasemian H, Hosseini S, Khodaparast M. Hinged capsulotomy – Does it decrease floaters after yttrium aluminum garnet laser capsulotomy? Middle East Afr J Ophthalmol. 2015;22(3):352-344.
16. Goble RR, O’Brart DP, Lohmann CP, Fitzke F, Marshall J. The role of light scatter in the degradation of visual performance before and after Nd:YAG capsulotomy. Eye. 1994;8(5):530-534.