The Symbiotic Relationships of the O’s
Optometry and ophthalmology can work side by side for the benefit of all.
By Casey Claypool, OD
Empire Eye Physicians became the first ophthalmology clinic in our region—Eastern Washington and Northern Idaho—to work closely and openly with local optometrists about 30 years ago. Long before I joined the practice in 2012, Mark Kontos, MD, and Christopher Sturbaum, MD, had already established a reputation for fostering OD/MD relationships for the good of both their own practice and those of their referring optometrists.
My job at Empire Eye is pretty simple and quite fun: building bridges and taking care of patients. When I was hired, Dr. Kontos told me that he and Dr. Sturbaum would treat me and train me to be like an ophthalmologist in the clinic. I would handle pre- and postoperative patients, emergencies, and referred patients, just as they would.
I was excited: This arrangement made me feel like an equal colleague. When I came on board, the staff members were trained to educate patients about why they were seeing an optometrist at this previously all-ophthalmic practice.
In addition to my duties in the office, I was given administrative time during which I could travel and visit local optometric offices. Many of our patients are referred from local offices, but others may travel from 150 miles away. As I developed relationships with the optometrists throughout the region, they and their staff members became comfortable approaching me with issues that arose. Although our office runs smoothly for the most part, it is inevitable that there will be hiccups along the comanaged pathway, and these require open communication between the referring office and our surgical center. Because I have established an open dialogue with the referring offices, many of these problems can be addressed and fixed before they become troublesome.
As our practice grew, we built another office location and brought on two new practitioners—a retina specialist, David Skale, MD, and another optometrist, Alisha Heaton, OD. Dr. Heaton and I work together as we coordinate referrals, manage pre- and postoperative patients, and maintain relationships with our referring practices. We hold small continuing education events several times a year and one large event that draws about 100 ODs from the surrounding area.
SYMBIOTIC RELATIONSHIP
In general, optometrists love to see patients in the chair and ophthalmologists love to operate. That’s usually why we have chosen our respective fields, and that is the symbiotic division of labor that our practice is built on. The more I see of the pre- and postoperative patients, emergency patients, glaucoma follow-ups, dry eye patients, and so on, the more the MDs are freed to do what they love. In this arrangement, the OD practices at the top of his or her level medically, and the MD practices at the top of his or her level surgically. This mutually benefits both parties and allows them to do what they find most rewarding.
From a financial perspective, this OD/MD relationship is mutually beneficial as well. The MD is free to see more cataract consults and operate more, and this generates greater revenue for the practice than, say, performing a diabetic eye exam or treating a corneal ulcer would. In 4 years, we doubled our cataract surgical volume, and it continues to increase.
BENEFITS TO THE PATIENT
We all know there is already a shortage of ophthalmologists nationally, and as the baby boomers age this will only continue. Optometrists are well trained to work hand-in-hand with ophthalmologists, caring for patients and ensuring that there is adequate access to ocular health care.
When I first joined the practice, Drs. Kontos and Sturbaum were both booked out more than a month in advance, making it difficult for patients to come in on an emergency basis. I immediately took all the triage calls of flashes, floaters, and red eyes. Patients were grateful to be seen sooner, and they also appreciated hearing a diagnosis confirmed by doctors who conferred together. Many times we consult each other regarding difficult cases, which helps tremendously with patient care. It goes without saying that patient care improves when doctors are able to easily consult on challenging cases.
Dr. Heaton and I love working with patients who have dry eye disease, whereas our surgeons do not concentrate in this area. When they refer patients to our specialty dry eye clinic, patients know they are getting the care they need and are extremely grateful.
The ODs also handle much of the chair time for patient education before and after premium IOL implantations. Many patients opting for these lenses require extra handholding, and we work closely with our surgeons to ensure that the patients get the help they need without taking up the surgeons’ chair time.
HIRE AN OD
Gone should be the days when ophthalmologists view optometrists as competitors, and vice versa. The symbiotic relationship in our practice, with ODs and MDs working together, is beneficial on all levels. It provides rewarding careers and financially sound growth for the practitioners and ensures that we can focus on providing much-needed patient care.
If you are an ophthalmologist thinking about hiring an optometrist, go for it! Treat him or her like an equal colleague. The optometrists in the area will know about your symbiotic relationship, your surgical volume will increase, and you will soon see why this arrangement can be such a benefit for all involved.

Meeting the Demands of Surgical Patients
As volume increases, the collaborative model is the way to go.
By Bobby Saenz, OD, MS, FAAO
Despite the increasing number of patients in need of medical eye care and ophthalmic surgery, the number of eye surgeons remains constant.1,2 A 2014 report by the humanitarian organization Prevent Blindness predicted that 45.6 million Americans will need cataract surgery in the year 2050.3 At the same time, there is increasing demand for refractive surgery and refractive cataract surgery, which is leading more ophthalmologists to focus on this burgeoning subspecialty. (This, perhaps surprisingly, is in alignment with modern optometry, and later I will explain how.)
At Parkhurst-Nuvision, where I practice in San Antonio, Texas, we believe that a collaborative care model in which optometrists and ophthalmologists partner together can solve many problems, including meeting the increasing demand for eye care services. It also renders obsolete the old-school turf war that used to rage between ophthalmologists and optometrists.
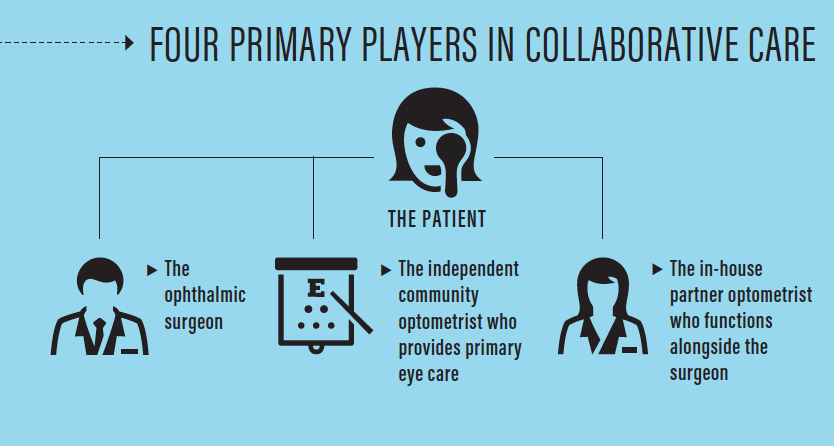
In the collaborative care model, there are four primary players whose roles I should define up front: the ophthalmic surgeon; the independent community optometrist who provides primary eye care; the in-house partner optometrist who functions alongside the surgeon; and, most important, the patient (see infographic below). In the collaborative eye care model, the community optometrist focuses on primary eye care, including routine eye exams, glaucoma surveillance, and diabetic eye disease screening, and on comanagement of refractive and cataract surgery patients. Meanwhile, the surgical practice team—the MD and in-house OD, working together—focuses on surgical solutions and the treatment of advanced ocular disease.
HOW IT WORKS
As a partner optometrist in the surgical practice at Parkhurst NuVision, my role as Clinic Director is not to perform routine eye care or to maintain an optical business; rather, it is centered on collaborative care with independent optometrists in our community. I help to manage the patients that they refer to us for advanced medical and surgical care. This primarily involves interpreting higher-level diagnostic scans and in-depth questionnaires for the surgical patients, but it also includes helping to set appropriate expectations for patients needing cataract, refractive, keratoconus, and microinvasive glaucoma surgeries.
We have great success setting patient expectations, and this is in large part thanks to the primary care optometrists in our community who have enjoyed long-term doctor-patient relationships with the patients they refer to us. Because of these deep relationships, they are able to communicate effectively to us the patients’ visual needs, expectations, and likes and dislikes about their vision. There is no substitute for the time it takes to develop this level of understanding between doctor and patient, and this is a crucial part of our process. It’s not uncommon for me to call one of our primary care optometrists, even while his or her patient is still in our chair, to ensure that we are choosing the appropriate technology for the patient. Great patient care requires extraordinary communication!
NO PRIMARY CARE
It is important to note that the most successful ophthalmic practices using the collaborative care model typically do not maintain an optical shop, nor do they perform primary eye care themselves. This creates an environment where both practices—the surgical practice and the community optometrist—are in alignment to create the best medical and surgical results for their patients without any competition.
In this model, everyone wins. The community optometrists win because they maintain their role as the primary eye care provider before and after their patients’ surgical events. The in-house partner optometrists—who like me have sought out residencies in anterior segment and ocular disease—win because we are passionate about caring for patients through their surgical planning and early or challenging postoperative care. And the surgeons win because their skill sets are maximized where they can deliver the biggest impact: doing surgery. Most important, patients win because they get an experienced, well-practiced surgeon and a team of doctors who collaborate to ensure that their outcomes exceed their expectations.
DELEGATION, TRAINING ARE KEY
The partnership between optometrists and ophthalmologists in the surgical practice, specifically the delegation of surgical planning and early postoperative care to the optometrists, allows more time for the surgeon to do more surgery and see more patients. This works only if the surgical practice optometrist has a deep understanding of the surgical technologies used by the surgeon he or she partners with. These are topics that are beginning to be taught in optometry schools with regularity today. After graduation, optometrists who want to thrive in this role should seek additional training, for example through a residency in refractive surgery and ocular disease.
We recognize the need for more refractive surgery–oriented optometrists. Thus, another responsibility of mine is to work to provide updates on the latest surgical advances to community optometrists who are interested in being involved in our model through continuing education events.
I also help to teach the students who rotate through our clinic on a monthly basis. One of the unique features of our practice is that we are located adjacent to the Rosenberg School of Optometry, and it is a mandatory part of their curriculum that every student rotate through our clinic for full-time immersion in clinical care involving refractive surgery patients. The school has embraced the goal of being the leading optometry institution for surgical comanagement, and its leaders understand that we must train more optometrists in the comanagement of cataract and refractive surgery to meet current and future patient needs and demands.4 (This was what I meant when I said that modern optometry is in harmony with the current trend among ophthalmologists toward performing more refractive and refractive cataract surgery.)
MEETING DEMAND
The collaborative care model will be increasingly necessary if we are going to maintain a high degree of patient satisfaction while meeting the demands of patients who need cataract or refractive surgery. We are already seeing how this is paying dividends for our patients in Texas. Optometrists who now feel comfortable and knowledgeable with surgical comanagement are sending us patients who are already well educated about all the options they have at the time of cataract surgery. Because of the commitment and knowledge of these primary care optometrists, their patients have access to skilled surgeons and the latest technologies. And they benefit from a team of doctors who together are communicating, collaborating, and seamlessly delivering unparalleled quality of care.

Coordinate Your Messages for Collaborative Care
The optometrist and ophthalmologist must be on the same page in their dealings with comanaged patients.
By Justin Schweitzer, OD, FAAO
At Vance Thompson Vision, I play multiple roles. I am a clinician, an educator, and a liaison to our optometric referral network.
I manage and run a daily clinic for a fellowship-trained anterior segment and glaucoma surgeon. My daily activities include pre- and postoperative evaluations and management of anterior segment disease and glaucoma. A lot of my day is spent preparing patients for cataract, glaucoma, cornea, and refractive surgery. I also work closely in an educational capacity with our ophthalmology fellow, optometry resident, and optometric interns. Finally, an important role I play is taking time out of my clinic schedule to meet with optometrists who place their trust in our practice to perform surgery on their patients. I listen, discuss, and work with them to improve the ways we communicate and provide services for their patients.
ADVANTAGES OF THE MD/OD RELATIONSHIP
The population of the United States is getting larger and older. Unfortunately, along with those trends comes more disease and, for our discussion here, more eye disease. The number of patients who need ocular surgery is increasing with the growth of the population’s age and size, and it will become more difficult for surgeons to meet the demand. In this scenario, there are many advantages to collaborative care between optometrists and ophthalmologists, including the four I discuss here.

No. 1: Patient care is better. With collaborative care, I am able to use my talents taking care of patients in the clinical setting, and the surgeon I work with is able to use his talents in the OR. Many times, two heads are better than one. When we are dealing with a complicated patient, both the OD and the ophthalmologist can contribute ideas and thoughts, and together we can provide a better solution than if only one of us was thinking through it.

No. 2: The patient experience is better. Wait times for cataract surgery and other ocular surgeries in certain parts of the United States are far longer than they need to be. If ODs can handle the pre- and postoperative care and ophthalmologists are in the OR doing what they do best, a decrease in wait times occurs, and this improves the patient experience.

No. 3: Pathology can be treated preoperatively. With the increasing number of patients needing surgery, a burden is placed on eye care providers to treat any existing ocular disease before surgery. An excellent example of this is ocular surface disease. In a collaborative care arrangement, the OD can relieve this burden by managing the patient’s ocular surface disease before surgery, allowing the surgeon to continue to be in the OR performing surgery.

No. 4: Referrals increase. One of my roles is to communicate with community optometrists and generate referrals for our practice. With me taking on this role for the practice, we are able to keep our surgery schedule moving along. The ophthalmologist does not need to be out of the OR, and I am able to deepen relationships with my OD colleagues in our region and improve our services and communication for their patients.
MAKING COLLABORATIVE CARE WORK
Trust between the OD and MD in a comanagement arrangement is the single most important factor to achieving successful collaborative care. The ophthalmologist must trust that the OD is always going to do what is in the best interest of the patient, and the reverse is also true for the OD who is sending his or her patient for surgical care. He or she must trust that the ophthalmologist will always do what is in the best interest of the patient.
The OD and MD also must have similar sets of values when it comes to patient care. If the ophthalmologist believes in investing in the world’s best technology, it is imperative that the OD believe in that technology as well. In order to provide a great patient experience, the OD and MD need to have similar discussions with patients about the technology, or it could leave doubt in the patients’ mind regarding the surgery or perioperative care they are going to receive.

Integrated Eye Care: A Winning Combination
A team approach helps to provide continuity of care.
By Walter O. Whitley, OD, MBA, FAAO
Virginia Eye Consultants (VEC) is a tertiary referral practice whose mission is to provide world-class specialty eye care. Our integrated practice model provides medically necessary and elective eye services in a patient-first, practice-efficient model.
I serve as the director of optometric services at VEC, and my role is to oversee all aspects of MD/OD integration within our practice. The practice consists of 19 providers, including nine subspecialists, two comprehensive ophthalmologists, five full-time medical optometrists, one physician assistant, two optometric residents, and three optometric externs. I work closely with our surgeons and optometrists—no matter their specialty, subspecialty, or discipline—to ensure everyone is on the same page and working to maximize patient care and enhance the patient experience.
CARE TEAMS
In our practice, the optometrists help the surgeons and referring providers manage patients for various conditions. Optometrists handle perioperative care, dry eye disease, glaucoma and retinal surgery management, and emergency eye care visits. We have developed what we call provider care teams by specialty, and these teams help to comfort patients and ensure they trust that they will be well taken care of.
These dedicated teams include a cornea team consisting of one MD and one or two ODs, a glaucoma team consisting of two MDs and one OD, and others. The care team approach helps to ensure that practitioners are available for patient appointments and serves to reassure patients and address their needs. The care team concept allows the surgeon or other subspecialist to seamlessly transfer care to the team’s optometrist after surgery is successfully completed. For example, the specialist informs the postoperative patient that his or her eye is improving or stable and that he or she will see someone else on the team at the next visit. Because this information is coming directly from the surgeon, patients are compliant with and accepting of the team concept.
REFERRAL NETWORK
Most of our patients are referred to our practice from more than 250 community optometrists and health care providers. Crucial to the success of our practice are our working relationships with this referral network. We believe in a collaborative care model with a focus on patient-centered, cost-effective, and efficient delivery of care.
Our referring optometrists provide all of the primary eye care needs for their patients, and many are actively involved in providing medical eye care. When one of their patients develops a complex condition or needs surgery, a consultation, or a referral for medical eye care due to insurance reasons, the community OD refers that patient to our practice for a problem-focused exam.
Most new patients to our practice are seen by a surgeon for the initial evaluation and for the procedure, if one is deemed medically necessary. After the surgery, our surgeon and optometrists work together to see the patient postoperatively or, if the patient chooses, to refer him or her back to the comanaging optometrist for postoperative care.
WORDS OF WISDOM

Casey Claypool, OD
“It is inevitable that there will be hiccups along the comanaged pathway, and these require open communication between the referring office and our surgical center. Because I have established an open dialogue with the referring offices, many of these problems can be addressed and fixed before they become troublesome.”

Bobby Saenz, OD, MS, FAAO
“It is important to note that the most successful ophthalmic practices using the collaborative care model typically do not maintain an optical shop, nor do they perform primary eye care themselves. This creates an environment where both practices—the surgical practice and the community optometrist—are in alignment to create the best medical and surgical results for their patients without any competition.”

Justin Schweitzer, OD, FAAO
“The OD and MD also must have similar sets of values when it comes to patient care. If the ophthalmologist believes in investing in the world’s best technology, it is imperative that the OD believe in that technology as well. In order to provide a great patient experience, the OD and MD need to have similar discussions with patients about the technology, or it could leave doubt in the patient’s mind regarding the surgery or perioperative care they are going to receive.”

Walter O. Whitley, OD, MBA, FAAO
“By maintaining consistent communication with members of our referral network, we are able to keep them up to date on what’s happening in the practice. Our practice uses several means of communication with the network, from weekly email blasts and quarterly newsletters to lunch-and-learns and educational seminars. The more interactions we have with our referring providers, the stronger our relationships become. Most of them have all of our personal contact details and can get hold of us at any time in regard to patient questions or concerns.”
OUTREACH TEAM
As our practice grows, so do the needs of our optometric community. We must continually make sure that we are supplying our referring providers with up-to-date patient education materials, support, and updates on our practice’s offerings. In order to meet those needs, we have invested in a provider relations and community outreach team to improve communication and integration with our referral network.
This team includes an OD who helps serve as an additional practice liaison, a practice development manager who assists in calling and visiting referring providers, a practice development coordinator who responds to emails or phone calls from providers, and a leader who oversees the team—that’s me. We hold weekly meetings to review our referral numbers, go over upcoming events, brainstorm opportunities, and discuss any issues within the network. These regular meetings allow the team to continually evaluate our opportunities and potential issues or threats that may arise within the network.
CONSTANT COMMUNICATION
The key to our practice and our referral network is continuous communication. By maintaining consistent communication with members of our referral network, we are able to keep them up to date on what’s happening in the practice. Our practice uses several means of communication with the network, from weekly email blasts and quarterly newsletters to lunch-and-learns and educational seminars. The more interactions we have with our referring providers, the stronger our relationships become. Most of them have all of our personal contact details and can get hold of us at any time in regard to patient questions or concerns. Whether through personal calls, secure emails or texts, or in-person visits to discuss patient care, these interactions help to strengthen the bonds between providers and to maximize patient care.
Patients benefit the most from our integrated eye care model, with a team of providers to address their vision and medical eye care needs. Optometrists provide more than 70% of all eye care visits in this country and see patients of all ages to address their primary eye care needs. Many optometrists have developed strong relationships with their patients over their lifetimes and understand their vision needs, how they use their eyes at work and at leisure, their ocular and systemic histories, and their individual personalities.
Patients have the comfort of seeing a provider they are familiar with. Many patients prefer to see their optometrist for postoperative care due to convenience because they live or work closer to the referring optometrist’s practice than to our center. Our practice and our referring providers always put patient care as our top priority. As a team, we continuously work together to provide optimal patient care.
1. Resnikoff S, Felch W, Gauthier T, et al. The number of ophthalmologists in practice and training worldwide: A growing gap despite more than 200,000 practitioners. Br J Ophthalmol. 2012;96:783-787.
2. Association of American Medical Colleges website. The complexities of physician supply and demand: Projections from 2014 to 2025: 2016 update. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Accessed June 14, 2018.
3. The Future of Vision. Prevent Blindness. June 11, 2014. https://www.preventblindness.org/future-vision. Accessed June 14, 2018.
4. Sandberg KA. How students learn perioperative care. http://www.optometrytimes.com/optometry/how-students-learn-perioperative-care. Accessed June 14, 2018.