
In the past, when clinicians identified patients with keratoconus or post-LASIK ectasia, the doctor-patient discussion was very challenging. There was no effective treatment available to prevent patients with keratoconus from progressing to a stage at which a corneal transplant might be necessary. Similarly, prior to the availability of the cornea-strengthening procedure CXL, patients with post-LASIK ectasia had few options, and some ended up requiring a transplant as well.
Thankfully, with the development of CXL, patients who are diagnosed with keratoconus or post-LASIK ectasia now have a safe and effective therapy that can stop the condition from worsening in 97% to 99% of cases with a single treatment.1,2 Many patients who undergo CXL also experience a significant improvement in vision and corneal shape over time.3
With the availability of CXL, the main challenge is now to identify patients at risk for these ectatic conditions at the earliest stage possible. It is therefore helpful for clinicians to perform corneal mapping whenever there is a suspicion that keratoconus or post-LASIK ectasia may be present.
IDENTIFYING PATIENTS
One barrier to making an early diagnosis is that slit-lamp examinations in these patients at risk typically have normal findings. This is not the case with advanced keratoconus, when signs such as Vogt striae, apical scarring, and Fleischer ring can be seen at the slit lamp. But in advanced keratoconus, patients have generally already experienced visual loss. To identify the condition before visual loss occurs, therefore, clinicians must focus on other tools that can provide evidence.
Corneal topography and tomography are two such tools. In patients who present with increasing astigmatism and/or a loss of BCVA, corneal mapping can be used to evaluate for changes in corneal shape. Other red flags include a family history of keratoconus, the presence of significant ocular allergies associated with vigorous eye rubbing, and a history of sleep apnea.4 Clinicians should consider performing topography in any patient with these conditions associated with keratoconus.
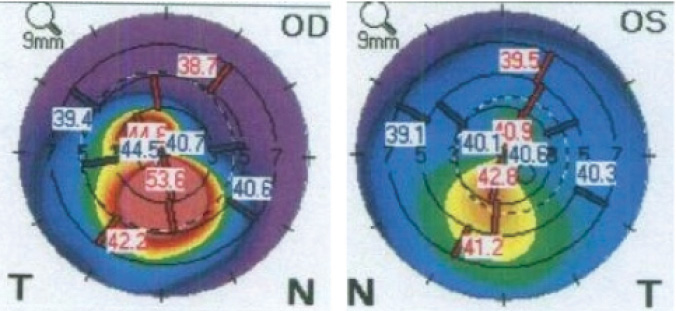
Figure 1. A patient with moderate keratoconus in his right eye (Left) and inferior steepening consistent with early keratoconus in his left eye (Right).
Another barrier to identifying patients at risk is that individuals with keratoconus or post-LASIK ectasia can present with very good vision—even 20/20 UCVA. Figure 1 shows topography maps of a 25-year-old man with moderate keratoconus in his right eye and BCVA of 20/40. The patient’s left eye has 20/20 UCVA but demonstrates inferior steepening consistent with early keratoconus. Figure 2 shows topography maps of a woman who underwent LASIK 15 years earlier, developed post-LASIK ectasia in her right eye, and underwent CXL to halt the progression and improve corneal shape and visual acuity. Over time, she developed inferior steepening in her left eye consistent with early post-LASIK ectasia despite maintaining 20/20 UCVA. She elected to undergo CXL in her left eye to prevent worsening of the ectasia (Figure 3).
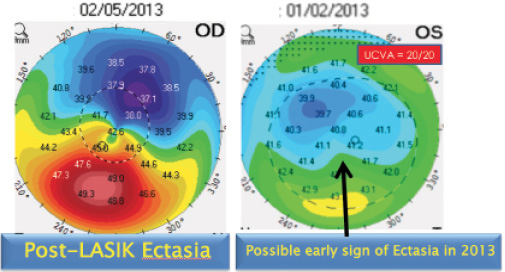
Figure 2. Topography maps of a patient with post-LASIK ectasia.
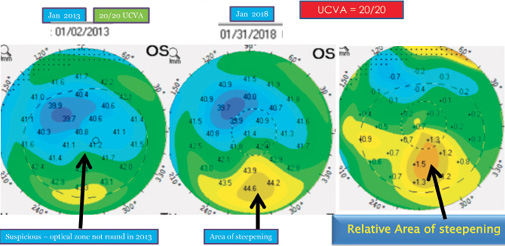
Figure 3. Inferior steepening consistent with early post-LASIK ectasia.
FOLLOWING UP
Corneal topography and tomography are effective tools to screen patients for signs of early keratoconus. Following CXL, these technologies are also effective for determining whether the procedure has stabilized the cornea and whether there has been improvement in corneal shape over time. The corneal topography maps in Figure 4 are from a patient enrolled in a clinical trial for epi-on CXL who demonstrated significant improvement in corneal shape over a 5-year period. At 6 years, the corneal shape improved even further. The maximum keratometry (Kmax) value decreased from 53.60 D preoperatively to 49.20 D at 5 years and to 47.90 D at 6 years.
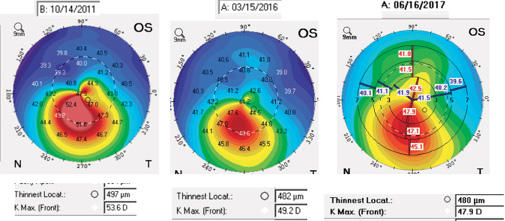
Figure 4. Topography maps of a patient enrolled in a clinical trial for epi-on CXL demonstrate significant improvement in corneal shape over a 5-year period.
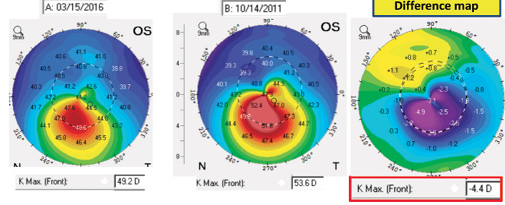
Figure 5. Improvement in corneal shape over 5 years. Flattening is indicated by the blue/ purple shading, and superior steepening is indicated by yellow.
Topographic or tomographic difference maps can help clinicians to monitor change in corneal shape over time (Figure 5). In many cases, keratoconus remains stable when it develops in older patients; however, there are exceptions, and some older patients can show progression. Figure 6 shows the change in corneal shape over a 10-year span in a 70-year-old patient with a history of LASIK. The difference map shows that Kmax increased by 4.90 D over this period.
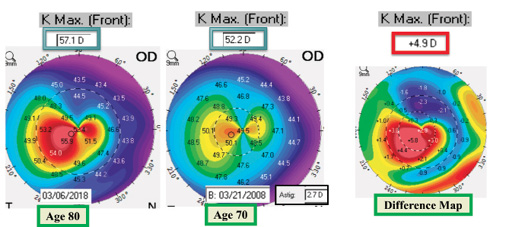
Figure 6. Change in corneal shape over a 10-year span in a 70-year-old patient with a history of LASIK.
NEW MEASURES
Several promising technologies to assist in the identification of patients with early keratoconus have recently emerged. These include epithelial mapping and the measurement of corneal biomechanics. Both technologies are commercially available but not yet widely used.
At least two available devices can perform epithelial mapping. Cornea Advance (Optovue) anterior segment OCT can map epithelial, stromal, and total corneal thickness and help to identify thinning in eyes with early keratoconus. The Artemis 2 high-frequency ultrasound system (ArcScan) provides a detailed image of epithelial thickness across the cornea and can be used to identify apical thinning.
To measure corneal biomechanics, clinicians can use the »ORA ocular response analyzer (Reichert), with recently introduced software designed to detect keratoconus. The »Corvis ST (Oculus Optikgeräte) also measures corneal biomechanics, using a high-definition video camera to record the reaction of the cornea to an air pulse. The system is designed to differentiate a normal corneal biomechanical response from one that indicates keratoconus.
CONCLUSION
The availability of CXL allows eye care providers to offer a safe and effective therapy for strengthening the cornea to their patients with keratoconus or post-LASIK ectasia. The challenge remains identifying patients at an early enough stage that CXL can be implemented to prevent loss of BCVA.
Because patients with early keratoconus present normally at the slit lamp, it is up to clinicians to use topography, tomography, or the newer tools of epithelial mapping and corneal biomechanics to identify patients at increased risk for keratoconus. With greater awareness of these conditions and the availability of new and advanced diagnostic testing, one can hope that clinicians can identify most patients before they experience significant vision loss from these treatable conditions.
1. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620-627.
2. Antoun J, Slim E, El Hachem R, et al. Rate of corneal collagen crosslinking redo in private practice: risk factors and safety. J Ophthalmol. 2015;2015:690961.
3. Hersh PS, Greenstein SA, Fry KL. Corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37:149-160.
4. Gupta PK, Stinnett SS, Carlson AN. Prevalence of sleep apnea in patients with keratoconus. Cornea. 2012;31(6):595-599.




