Accessibility for Blind Patients
Alex Cohen, PhD
United States

Cataracts create difficulties for a wide range of people, including those with vision loss due to degenerative retinal disease. Most patients with low vision understand that cataract surgery will not cure their disease or reverse its progression. Not unlike those contending with cataracts as a singular malady, however, patients with low vision hope that cataract surgery will improve their vision, even if only slightly, until their disease progresses.
Cataract surgery in patients with low vision requires special considerations that begin well before surgical preparations. Is your website and scheduling tool accessible to patients who are unable to use a mouse or those who rely on assistive technologies such as software and apps that read online content out loud to users? Do you have educational resources available that patients with low vision can review easily by themselves? Videos and comprehensive materials provided by ophthalmologic societies or produced by your marketing department may not be useful to these patients. A more appropriate resource for this population is PDFs that are compatible with screen-reading software programs and apps.
Postoperatively, patients with low vision may need assistance understanding and filling their prescriptions. The Accessible Pharmacy app (Accessible Pharmacy Services) is HIPPA-compliant, ultrasimplified optical character recognition software that reads the contents of prescription medication packages out loud to the user.
CONCLUSION
Removing barriers and challenges for patients with low vision through better awareness, staff training, and accessibility can help alleviate many of the fears and anxieties of these patients (see Four Additional Considerations for Low Vision Patients). Solutions and resources are available to help these patients live more independently while reducing the stress involved with cataract surgery.
Four Additional Considerations for Low Vision Patients
No. 1. Harsh fluorescent lighting in medical practices can create glare and contribute to mobility issues when patients navigate the waiting area or find the restroom. Is your staff trained as sighted guides or in offering specific directions without the value of sight to assist patients in comfortably navigating the space?
No. 2. COVID-19 restrictions may mean that a support person cannot accompany patients to their appointments. Completing and signing forms can be difficult for patients with low vision to finish on their own. Is your staff trained to assist these patients with these forms empathetically and discreetly?
No. 3. Scheduling preoperative laboratory testing, reviewing presurgical guidelines, and scheduling surgery can be daunting for patients with low vision. Does your routine explanation of all this information help patients with low vision, or does it demonstrate a lack of understanding and empathy while creating fear and stress for the patient?
No. 4. Patients with low vision often have difficult administering postoperative eye drops. Prescribing larger amounts of medication and supplying apparatuses to help minimize wasted drops are two ways to help alleviate this problem.
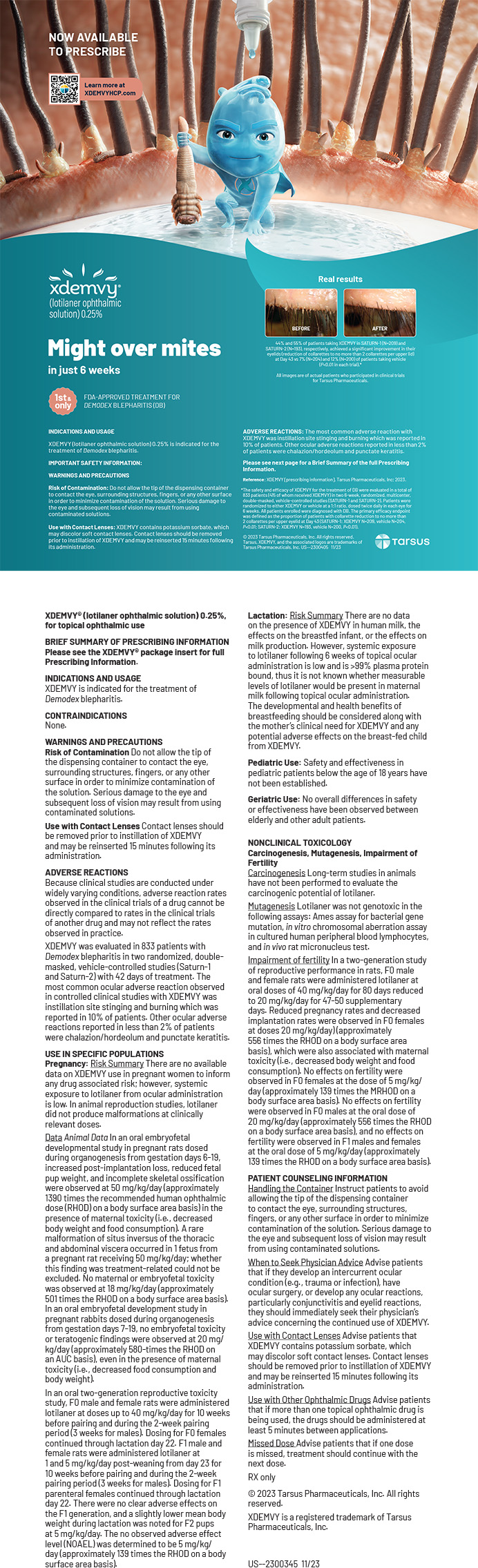
Four Practical Uses for Apps in Ophthalmology
Alexander Knezevic, MD
United States

Access to smartphones has changed many industries, and health care is no exception. Working in the technology- and device-heavy field of ophthalmology, I find that one of the handiest tools is already in my pocket.
I have used various apps to study for boards, review for a case, and examine patients. Apple’s App Store and Google Play provide access to many ophthalmology-specific apps. The following are what I consider to be some of the best apps in four categories.
Category no. 1: EDUCATION
AAO Ophthalmic Education (American Academy of Ophthalmology). This app is a true one-stop shop for eye education. Users can double-check eye conditions and management protocols through access to both The Wills Eye Manual (7th edition) and EyeWiki. The app also includes a series of “Dx This” mystery cases to help users prepare for the Ophthalmic Knowledge Assessment Program test and medical boards. The app includes current surgical videos and articles published by some of ophthalmology’s most prominent surgeons.
YouTube (Google) and Eyetube (Bryn Mawr Communications). Surgical videos are a must-have for the ophthalmic surgeon. I am constantly reviewing and fine-tuning my technique by watching videos from other surgeons. In addition to the YouTube and Eyetube apps, I rely on the online Eyetube video library to view surgical videos. All three are perfect resources for reviewing a video before cases or prepping for a new technique or procedure. These growing libraries of videos are available on demand at no cost.
OphthoQuestions (Ophtho Questions). Like the popular question banks of medical school, this app is a comprehensive question bank specifically for ophthalmology. Questions are created and reviewed both by board-certified ophthalmologists and trainees and specifically designed for the Ophthalmic Knowledge Assessment Program test and medical boards.
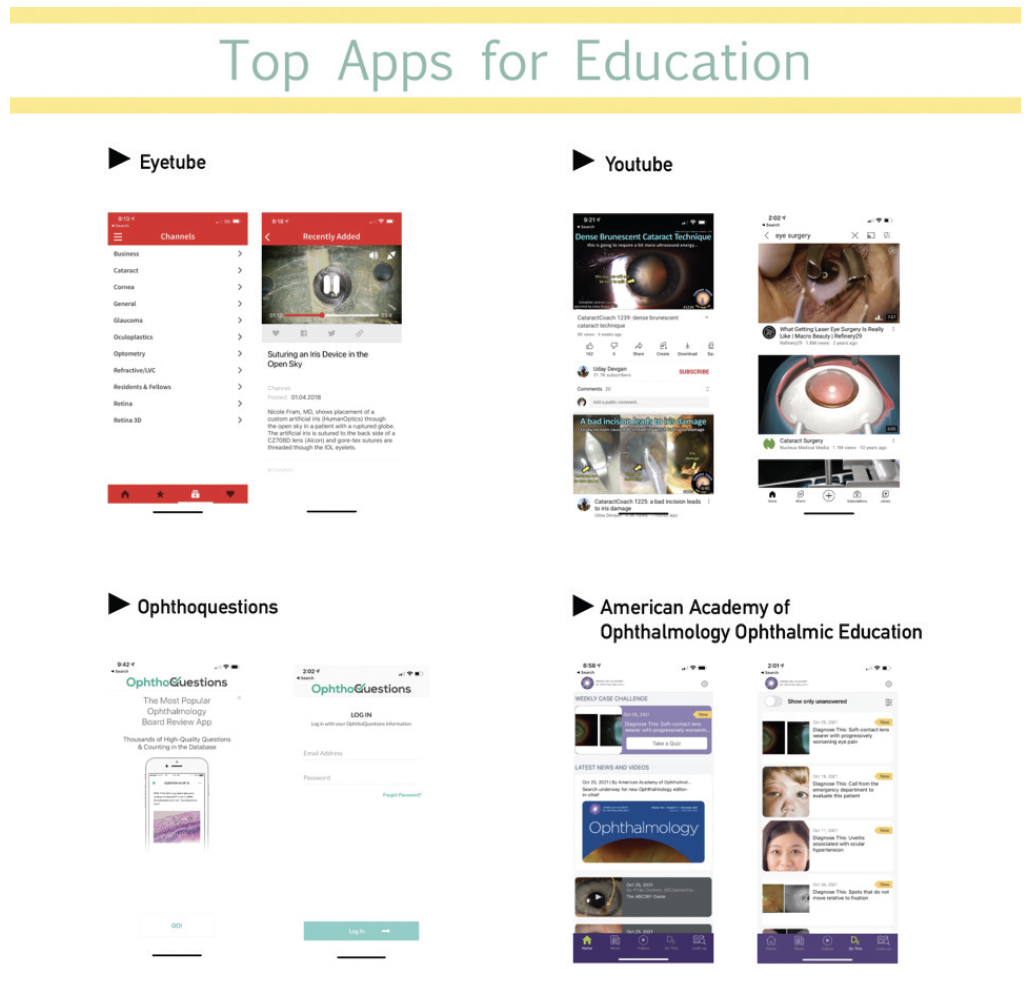
Category no. 2: CLINIC USE
PocketEyeExam (Nomad). It may be a no-frills app, but PocketEyeExam has been on my home screen for years. Can’t find a vision card? Use the app’s intermediate vision checks. Possible neuro-ophthalmologic problem? Use its Ishihara plates. Not sure what a patient’s visual potential is? Click on the app’s optokinetic nystagmus strip function. Registration and sign-up are not required.
Ullman Indirect (Michael Ullman, PhD). It takes some time to get used to, but Ullman Indirect with your condensing lens can obtain fundus photos right on your smartphone. The app allows you to adjust light and take either photos or videos of the retina. It’s a handy tool, particularly if looking to get an opinion from a retina colleague.
Category no. 3: PATIENT uSe
EyeDropAlarm (Kayur Shah, MD). This app schedules eye drop reminders for patients. Users select the eye drop type from a list and set how many times a day they want the alarm to go off.
Uber (Uber Technologies) and Lyft (Lyft). Getting to doctor’s appointments can be challenging for some patients, especially those with visual impairment. These apps allow the user to call a car immediately or schedule ahead of time.
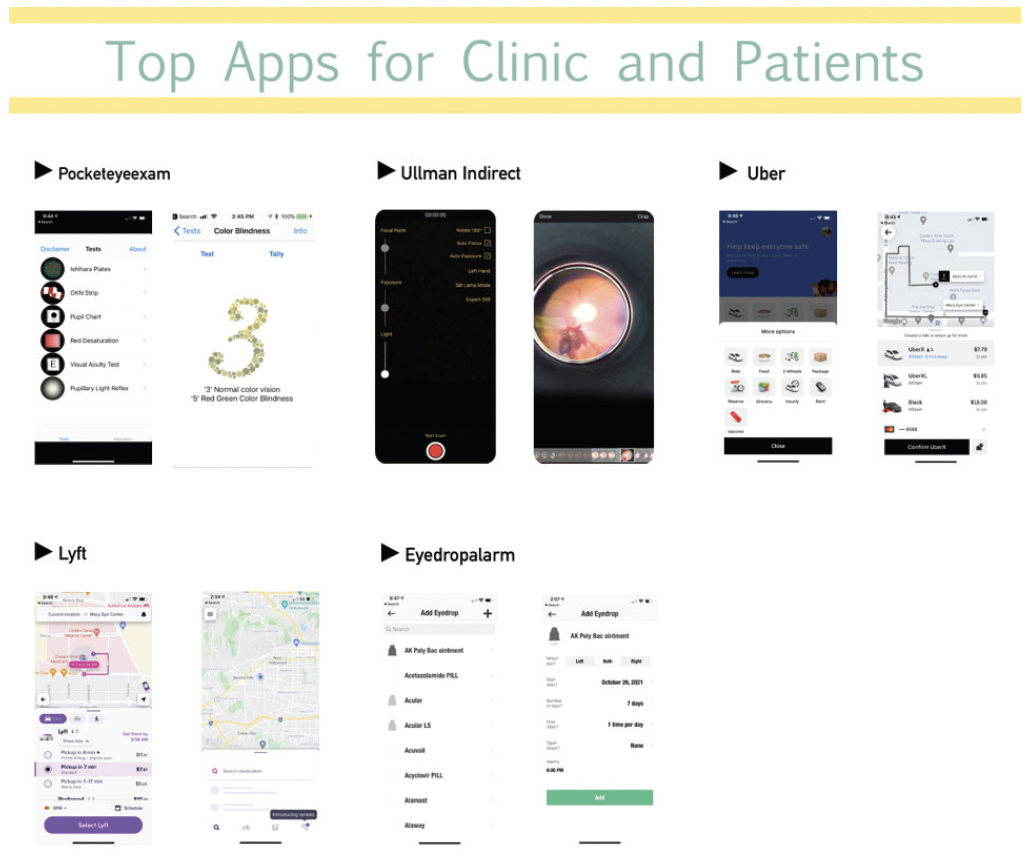
Category no. 4: NETWORKING
Instagram (Meta)/TikTok (Tik Tok)/Facebook (Meta)/Twitter (Twitter). Digital marketing and social media in medicine have entered the mainstream. Fortunately, you don’t have to do a TikTok dance to benefit (although I won’t stop you). Depending on their age, your patients are likely on at least one of these four social media platforms. Use of these apps is an opportunity to connect with patients. The platforms can be used to promote your practice, connect with current and prospective patients, advertise a residency program, and provide educational content. Social media is a high-impact and low-expense marketing tool.
Doximity (Doximity). This app has become a popular platform for health care providers. Doximity hosts job listings, current literature, and personal updates from medical colleagues. It’s like LinkedIn for medicine. Additionally, Dialer is built into the app; health care providers can place calls to patients from their cell phone while displaying their preferred callback number on caller ID.
CONCLUSION
The use of smartphone apps is a necessity for eye care professionals. The apps highlighted in my contribution to this article are valuable resources that can help improve efficiency and provide the best quality of eye care in the technology age.
dropAdrop Eye Drop Reminder
Ali Mearza, MBBS, FRCOphth
United Kingdom

The dropAdrop app (OCL Vision; Figure 1) was developed over the past 5 years and inspired by a patient’s comment that the drop regimen after their procedure was hard to follow. This patient wondered if the process could be made easier with an app. My colleagues and I jumped on the idea.
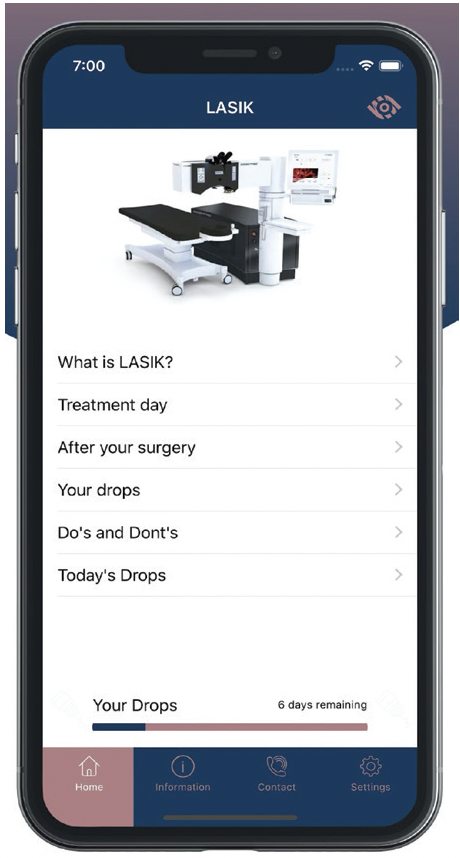
Figure 1. The user interface from the dropAdrop app.
DEVELOPING THE APP
Once we had researched feasibility, we planned the app’s functionality, look, and feel. We then enlisted the help of an app developer. Our collaboration involved beta testing to ensure that the app worked as promised and was easy to use and navigate.
Significant costs are associated with app development, and a developer’s time must be factored into the budget. An app must be designed for both the Apple App Store and Google Play to work with all platforms. It is important to prepare a design and functionality brief at the outset so that all parties understand the outputs required.
FEATURES
We decided from the start to make the app free to all patients, even those undergoing surgery at a facility other than OCL Vision.
Drugs and dosing schedules depend on the type of treatment. The app is programmed with this information specific to OCL Vision and sends push notifications to remind our patients to take their eye drops. If users are undergoing surgery at another facility, they are prompted to enter the prescribed drugs, their dosing frequency, and the duration of treatment; the app stores this information and sends reminders. The app also provides dos, don’ts, and specific information on how to administer eye drops correctly.
Updates. Given the problems with patient compliance, we broadened the use of the app to cater to patients with chronic eye conditions such as glaucoma that require long-term medical therapy. Patients can enter each drug, its dosing frequency, and the duration of treatment. The app then sends reminders to improve adherence.
The app can now be used to send a questionnaire on quality of vision to patients after surgery. Responses can be collated and analyzed to help practitioners evaluate various technologies and procedures.
Future direction. We are currently taking steps to allow other clinics to use the dropAdrop app for their patients via a licensing arrangement that will retain the app’s functionality but permit rebranding and customization to suit practice-specific requirements. This functionality should become available in early 2022.
FEEDBACK
The response to the dropAdrop app from our patients has been excellent. One recent review in the App Store read, “It’s so simple but so useful. A great reminder, especially when you’re out and about or occupied with other things during the day. It’s a brilliant app.”
The dropAdrop app is an example of how technology can be used for the benefit of patients.
What Gets Us From A to See?
Marcus Pedersen, MAT, FHEA, and Radhika Rampat, MBBS, BSc (Hons), FRCOphth
United Kingdom


During the COVID-19 pandemic, many patients have missed medical appointments or had those appointments delayed. The health care field has responded by turning increasingly to mobile health (mHealth) and telehealth to facilitate patient care.1 The World Health Organization’s Global Observatory for eHealth uses the term mHealth to refer to medical and public health practices supported by mobile wireless devices such as phones, patient monitoring devices, and personal digital assistants.2 This digital renaissance has included the development of mobile applications to educate patients in the comfort of their own homes, allow them to monitor their medical conditions from home, and help nonclinical and clinical staff members assess patient health.2,3
Our contribution to this article describes eight apps (Figure 2) designed to support the ophthalmic health care system. Not all of them have been clinically validated.

Figure 2. The apps on this home screen are designed to support the ophthalmic health care system.
HOSPITAL CARE
MicroGuide (Horizon Strategic Partners). This app is used for all specialties across many National Health Service trusts in the United Kingdom. Users recently gained access to useful treatment algorithms on the Moorfields Emergency Guidelines app, otherwise known as MEGA, via this platform. This information is not a replacement for established local protocols.
EyeLogbook (Royal College of Ophthalmologists). This is the official app endorsed by the Royal College of Ophthalmologists to document procedures and facilitate the completion of trainees’ yearly reviews. Not only does this app keep track of procedural numbers, but it also provides a space where users can record comorbidities and complications to learn from them.
ToriCAM (Graham Barrett). Damien Gatinel, MD, PhD, designed the first smartphone-enabled noncontact solution for marking the eye. Unfortunately, his Toreasy and Toraxis apps are no longer available. The ToriCAM app by Graham D. Barrett, MB BCh SAf, FRACO, FRACS, however, is based on similar principles. ToriCAM offers a user-friendly method of determining the correct alignment of a toric IOL at the time of the cataract procedure and verifying the axis postoperatively.
EDUCATION
Complete anatomy ’22 (Elsevier). It can be difficult to view ocular anatomy. This app uses 3D objects to allow users to navigate the eye and learn about its specific anatomical features. There are in-app purchases.
AR Eye (Yetzer Studio). Experiencing another person’s vision loss could foster empathy and a better understanding of the difficulties that person faces. Users of this app can experience how five different diseases affect vision. This could be helpful for both eye care providers who must educate patients and for patients’ family, friends, and caregivers. Hospital staff could benefit from using this app as well.
Be My Eyes (Be My Eyes). What if a blind person could ask 5 million people for help by pressing a button? This may sound like science fiction, but it’s reality. Users of this app can connect to one of 5.4 million people who have volunteered to answer users’ questions or guide them through what the back camera of the user’s phone is seeing.
VISION MONITORING AT HOME
Patients who can detect changes in their visual acuity may feel more empowered in their own care. With quick and easy testing, two apps help patients to detect reductions in vision so that they can schedule a visit with their optometrist or ophthalmologist if necessary.
EyeHandbook (Cloud 9 Development). This app allows ophthalmologists, optometrists, and patients to measure visual acuity on a Snellen chart. The patient can also take the Ishihara test to detect color blindness. Numerous other tests and educational resources such as forums, medication information, and videos are available through this app.
dropAdrop (Ophthalmic Consultants of London). Poor adherence to prescribed medical therapy costs the United States $100 to $300 billion per year.4 This app is free to download and reminds users when it is time to take their drops. Unlike with a calendar app, users can specify the condition they have or the surgical procedure they are undergoing or underwent, any of which may require the administration of more than one type of medication. Additional drop regimens can be added.
1. Tarricone R, Petracca F, Ciani O, Cucciniello M. Distinguishing features in the assessment of mHealth apps. Expert Rev Pharmacoecon Outcomes Res. 2021;21(4):521-526.
2. Marcolino MS, Oliveira JAQ, D’Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6(1):e23.
3. Choe EK, Abdullah S, Rabbi M, et al. Semi-automated tracking: a balanced approach for self-monitoring applications. IEEE Pervasive Computing. 2017;16:74-84.
4. Benjamin RM. Medication adherence: helping patients take their medicines as directed. Public Health Rep. 2012;127(1):2-3.