When patients come to my practice for premium cataract surgery, we aim to do whatever it takes to make them happy. Happy patients help build your personal brand and premium cataract practice through word-of-mouth referrals, optometric referrals, and awesome five-star reviews. Building rapport and ensuring patient satisfaction and happiness start during the preoperative counseling process by outlining the pros and cons of each surgical option. The goal is to undersell and overdeliver.
When patients expect their surgical procedure to help them achieve freedom from glasses and/or contact lenses, the ability to make postoperative refractive tweaks is crucial. Depending on the practice setting, enhancement rates after cataract surgery range from 3% to 15%. When a premium cataract surgery patient is unhappy, you and your practice must do everything you can to make them happy.
ADDRESS THE PROBLEM
The greatest cost to any practice is an unhappy patient who feels they are not being taken care of. These patients pose a risk of spreading negative marketing about your practice, including how dissatisfied they are with their vision after you did their cataract surgery. Such messaging could negatively impact both word-of-mouth and optometric referrals to your practice and result in a dreaded one-star review on Google.
In my experience, being able to help an unhappy cataract patient can do a lot in terms of building your personal brand and reputation in your community. Identifying the cause of the patient’s dissatisfaction will help you determine the path forward to making them happy. This might require doing nothing, assessing and optimizing the ocular surface, resetting realistic expectations, or performing a LASIK enhancement or an IOL exchange (see Case Presentation).
CASE PRESENTATION
I recently performed cataract surgery for a patient with a history of LASIK surgery with a decentered myopic ablation (Figure). A 15.50 D monofocal toric IOL (Tecnis II Toric ZCU225, Johnson & Johnson Vision) was implanted in the patient’s left eye. At the 1-month postoperative visit, UCVA was 20/70 OS correctable to 20/20 with a +3.00 D refraction. The patient was unhappy with his final uncorrected visual acuity. We discussed the options for management, and he opted for an IOL exchange.
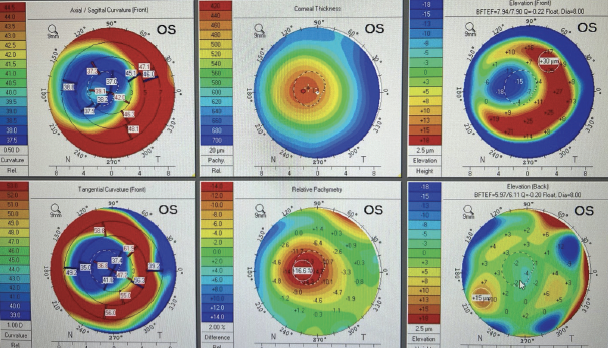
Figure. A decentered myopic LASIK ablation.
The IOL calculation suggested a 19.50 D ZCU225 IOL. Surgery was successful. At the 1-week visit, the patient’s UCVA was 20/20.
Even though the patient required an additional trip to the OR, he was happy with his final vision and overall experience. I did not bill insurance for the IOL exchange given that the reason for the surgery was for a refractive result.
LASIK enhancement. In my practice, the process for a LASIK enhancement after cataract surgery is seamless. We offer the procedure at no additional cost to the patient once refractive stability is achieved, which is typically around 3 months.
IOL exchange or removal. This process is more complex than an enhancement procedure because it involves a return to the OR and an anesthesiologist. For surgeons who do not practice in a setting with an in-office surgical suite, it also involves an ambulatory surgery center (ASC).
The use of Current Procedural Terminology (CPT) code 66986 (exchange of IOL) requires that the return to the OR be medically necessary. Documentation of patient complaints and/or mechanical failure of the IOL is required to support medical necessity claims under CPT code 66986. When IOL exchange is performed during the global period for cataract surgery (ie, 90 days), a CPT modifier 78 is required, indicating an unplanned return to the OR.
An IOL exchange performed for a refractive result is not a medical necessity, and insurance should not be billed. The devised payment strategy for these situations should work for you, the ASC (if one is used), and the anesthesiologist. This can be simpler to determine if your practice owns an ASC. If it does not, work with your ASC to establish how much you will be charged for the procedure.
CONCLUSION
Refractive cataract surgery is one of the most rewarding procedures we can offer our patients. In the rare instance that the refractive target is missed, an IOL exchange is one way to get your patients the outcomes they desire and promote the overall success of your practice. It is crucial to have a plan with your practice, ASC, and anesthesiologist for how enhancements are covered, especially when they are not covered under CPT code 66986.
Most patients are happy with their outcomes after cataract surgery. Show those who are not that you care, and provide them with the treatment they need to achieve their goals. In my experience, this can turn them from unhappy patients to some of your strongest advocates and biggest fans.