LASIK and PRK
Arjan Hura, MD

Advances in preoperative biometry, diagnostic imaging modalities, IOL calculation formulas, and surgical technique are improving the predictability of results and patient satisfaction after modern refractive cataract surgery. However, there is always the possibility of a suboptimal result. Surgeons should be ready to address issues as they arise.
SIX FACTORS
Six factors merit consideration before laser vision correction (LVC) is chosen as a method of enhancement.
No. 1: Is LVC the most efficacious method of enhancement? LVC might not be the most effective method of addressing residual postoperative refractive error if it is due to IOL tilt, rotation, decentration, or subluxation. In those situations, it may be best to consider repositioning or exchanging the IOL or implanting a secondary sutured IOL. If the residual refractive error is mild and the patient is not a good candidate for LVC, a piggyback IOL may be a simple and elegant solution (D. Brian Kim, MD, shares more about this method later in the article). If the patient’s complaint is related to contrast sensitivity, quality of vision, or dysphotopsias, consider exchanging the IOL for a monofocal lens.
No. 2: Have you addressed the unaddressed? Once refractive stability is achieved, four critical confounding variables must be assessed on examination and treated as needed to ensure a good result after a possible LVC enhancement.
- Carefully examine the eyelids, tear film, and cornea to assess if dry eye disease is influencing the patient’s refractive error. Also assess the cornea for signs of corneal edema, Fuchs endothelial dystrophy, epithelial basement membrane dystrophy, or Salzmann nodules/pterygia. Ocular surface disease is transient but common after ocular surgery and can affect a patient’s vision significantly.
- Check to see if the patient has a smoldering or rebound intraocular inflammation.
- Examine the posterior capsule for signs of significant opacification amenable to an Nd:YAG laser capsulotomy or capsular block syndrome causing a refractive shift.
- Examine the posterior segment for macular edema or other retinal pathology. In the presence of significant vitreous opacities that are likely the source of the patient’s symptoms, an Nd:YAG vitreolysis or a referral to a vitreoretinal specialist for vitrectomy should be considered.
No. 3: How did the patient respond to an enhancement trial? Demonstrate to the patient what they can reasonably expect from their vision after a potential second surgery. It can be helpful to show the patient at the phoropter or conduct a contact lens trial. If they are not satisfied with the trial or their BCVA does not improve significantly, do not proceed with the enhancement until the unaddressed variables are elucidated.
No. 4: Prepare for the enhancement. If you suspect a component of the capsule is contributing to the patient’s complaints, an Nd:YAG capsulotomy can be performed. Before the procedure, the patient should be advised that a future IOL exchange procedure will be more complex with an open capsule.
Most surgeons prefer to wait several months after lens implantation before performing an LVC enhancement to ensure refractive stability. This is a great time to address the factors listed in No. 2 (Have you addressed the unaddressed?). Review the patient’s medication list and history and decide on a plan for anesthesia. Finally, discuss the chosen LVC procedure with the patient and set reasonable expectations for their outcomes and time line for recovery.
No. 5: LASIK or PRK? Tailor the treatment to the patient and their optical system. Someone with a hyperopic refractive error or mixed astigmatism that has a spherical equivalent not close to plano may be better suited for LASIK versus PRK. LASIK may also be better for patients with a large refractive error to avoid the risk of haze that is associated with PRK. The epithelium can become looser with age, so care should be taken when lifting a LASIK flap in an elderly patient.
PRK may be a better option for a patient with epithelial dystrophy, a thin cornea, and keratoconus-spectrum disorders. Carefully evaluate topography, tomography, and epithelial maps to customize LVC enhancement.
No. 6: Know when to refer out. If you don’t feel comfortable performing LVC, refer the patient to a refractive surgeon in your community. The patient will appreciate a referral to a specialist who can help get them over the finish line.
Piggyback IOL
D. Brian Kim, MD

In 1993, Gayton and Sanders published the first case report of cataract extraction with simultaneous polypseudophakia for a patient with microphthalmos (axial length, 15.5 mm) who required 46.00 D of power.1 Two IOLs were placed in the capsular bag—the first published piggyback IOL procedure. It’s important to note that the risk for interlenticular opacification occurs due to the materials used in the IOLs and the placement of both lenses in the capsular bag. The risk for interlenticular opacification is eliminated when one IOL is placed in the bag and the other in the sulcus.
Placing a second IOL in the eye sounds like one of Dr. Frankenstein’s experiments, but it is a viable option in the right situation. The procedure is easy to perform (watch a piggyback IOL procedure below) and requires essentially no learning curve because every cataract surgeon has the requisite skills to place an IOL within the sulcus (Figure).
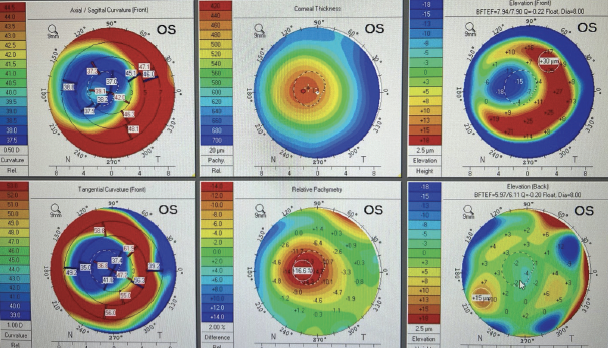
Figure. The piggyback IOL is implanted in the sulcus, and the haptic is dialed into place in the ciliary sulcus.
Courtesy of D. Brian Kim, MD
WHEN AND WHY
A piggyback IOL is used mainly to treat residual refractive error or negative dysphotopsia. An IOL exchange is another reasonable option for a refractive miss but is best performed during the early postoperative period before the IOL becomes fibrosed to the capsular bag. LVC (LASIK or PRK) can treat myopic errors effectively but is prone to regression when used to address high hyperopia.2 Reverse optic capture is arguably a more effective alternative than a piggyback IOL for negative dysphotopsia.3 In light of these considerations, I view piggyback IOLs as a useful tool with a narrow application.
IMPORTANT CONSIDERATIONS
The sulcus. As for any surgical procedure, proper patient selection is crucial. The piggyback IOL is placed within the ciliary sulcus, so adequate space is required. A wide sulcus is ideal to prevent IOL-iris chafing, pigment dispersion, transillumination defects, uveitis-glaucoma-hyphema syndrome,4 and cystoid macular edema.5 A peripheral iridotomy should be considered, especially when the sulcus is crowded, to reduce the risk of pigmentary6 or pupillary block glaucoma.7
Support. Strong zonular and capsular bag support is required for a stable piggyback IOL. Zonulopathy and zonular defects are a contraindication and can lead to late decentration or posterior dislocation of the IOL.8
Optic material. The rate of interlenticular opacification is high when the optics of the IOL placed in the bag and the piggyback IOL are both made of acrylic or PMMA.9,10 Acrylic-silicone or silicone-silicone combinations should be used because they tend to avoid interlenticular opacification.11
IOL design. Three-piece IOLs with a rounded anterior optic edge are preferable to IOLs with a square optic edge because the latter are more likely to cause iris thinning and atrophy, synechiae, and pigment dispersion.12 As an aside, one-piece IOLs have thick square-edged haptics that are even more likely to cause IOL-iris chafing; these lenses should never be placed in the ciliary sulcus.13 (See Power Calculation, for a tip on IOL calculations for IOL exchange procedures.)
POWER CALCULATION
Power calculations for a piggyback lens are simple and based on the patient’s pseudophakic refractive error. For a hyperopic refractive error,1 the spherical equivalent is multiplied by 1.5. For a hyperopic refractive error, the spherical equivalent is multiplied by -1.2. (For more on power calculations, see “IOL Exchange Calculations and Considerations.")
1. Gayton J, Raanan M. Reducing refractive error in high hyperopes with double implants. In: Gayton JL, ed. Maximizing Results: Strategies in Refractive, Corneal, Cataract and Glaucoma Surgery. Slack; 1996:139-148.
Surgical strategy. Patients who are poor candidates for LVC, such as patients with irregular corneas due to keratoconus or corneal scarring, are better suited to noncorneal intervention such as a piggyback IOL. Sometimes, a staged approach is beneficial. For instance, an eye with an existing corneal transplant can undergo cataract extraction and IOL implantation and later, after the keratometry readings stabilize, receive a piggyback IOL to address a residual refractive error.
WHICH IOL?
A few sulcus-specific IOL options are available outside the United States, including the Sulcoflex (Rayner), Add-on (HumanOptics), and 1st Add-on (1st Q GmbH). Toric and multifocal alternatives are also available.
In the United States, the only IOL approved for placement in the ciliary sulcus is the silicone SofPort (models LI61AO and LI61SE, Bausch + Lomb). The AO model has zero spherical aberration and is more tolerant of misalignment or decentration. Unfortunately, the SofPort line of lenses is available exclusively in plus powers and can therefore address only hyperopic refractive errors. The hydrophobic acrylic Sensar AR40 and Tecnis ZA9003 IOLs (both from Johnson & Johnson Vision) feature the proprietary anterior rounded OptiEdge design and are available in positive and negative powers, but the implantation of either lens in the sulcus is off label. The MA series of AcrySof IOLs (Alcon) is another off-label option, but these lenses have a square-edged anterior optic design and are therefore less favored for placement in the sulcus.12
LVC should be considered as a less invasive strategy to address low myopic refractive errors.
The Visian ICL (STAAR Surgical) is a sulcus IOL designed to correct high refractive errors in young phakic patients. The ICL may be used as a piggyback lens, but practically speaking, the cost would be prohibitive in most instances.14
CONCLUSION
The best candidate for a piggyback IOL has a primary IOL that is in the bag, stable zonules, a deep anterior chamber and ciliary sulcus, and a healthy corneal endothelium and macula. The indications for a piggyback IOL are limited, but it can be an excellent choice for specific scenarios given the straightforward surgical technique and immediate postoperative visual recovery.
1. Gayton JL, Sanders VN. Implanting two posterior chamber intraocular lenses in a case of microphthalmos. J Cataract Refract Surg. 1993;19(6):776-777.
2. Jaycock PD, O’Brart DP, Rajan MS, Marshall J. 5-year follow-up of LASIK for hyperopia. Ophthalmology. 2005;112(2):191-199.
3. Masket S, Fram NR, Cho A, Park I, Pham D. Surgical management of negative dysphotopsia. J Cataract Refract Surg. 2018;44(1):6-16.
4. Chang SH, Lim G. Secondary pigmentary glaucoma associated with piggyback intraocular lens implantation. J Cataract Refract Surg. 2004 Oct;30(10):2219-2222.
5. Davies EC, Pineda R 2nd. Intraocular lens exchange surgery at a tertiary referral center: indications, complications, and visual outcomes. J Cataract Refract Surg. 2016;42(9):1262-1267.
6. Iwase T, Tanaka N. Elevated intraocular pressure in secondary piggyback intraocular lens implantation. J Cataract Refract Surg. 2005;31(9):1821-1823.
7. Kim SK, Lanciano RC Jr, Sulewski ME. Pupillary block glaucoma associated with a secondary piggyback intraocular lens. J Cataract Refract Surg. 2007;33(10):1813-1814.
8. Kristianslund O, Dalby M, Drolsum L. Late in-the-bag intraocular lens dislocation. J Cataract Refract Surg. 2021;47(7):942-954.
9. Gayton JL, Apple DJ, Peng Q, et al. Interlenticular opacification: clinicopathological correlation of a complication of posterior chamber piggyback intraocular lenses. J Cataract Refract Surg. 2000;26(3):330-336.
10. Gomaa A, Lee RM, Liu CS. Polypseudophakia for cataract surgery: 10-year follow-up on safety and stability of two poly-methyl-methacrylate (PMMA) intraocular lenses within the capsular bag. Eye (Lond). 2011;25(8):1090-1093.
11. Cao KY, Sit M, Braga-Mele R. Primary piggyback implantation of 3 intraocular lenses in nanophthalmos. J Cataract Refract Surg. 2007;33(4):727-730.
12. Ollerton A, Werner L, Strenk S, et al. Pathologic comparison of asymmetric or sulcus fixation of 3-piece intraocular lenses with square versus round anterior optic edges. Ophthalmology. 2013;120(8):1580-1587.
13. Kirk KR, Werner L, Jaber R, Strenk S, Strenk L, Mamalis N. Pathologic assessment of complications with asymmetric or sulcus fixation of square-edged hydrophobic acrylic intraocular lenses. Ophthalmology. 2012;119(5):907-913.
14. Duncker GI, Sasse AC, Duncker T. A prospective pilot study using a low power piggy-back toric implantable Collamer lens to correct residual refractive error after multifocal IOL implantation. Clin Ophthalmol. 2019;13:1689-1702.