CRST: How would you manage a young patient who is unhappy after surgery on their first eye because of dysphotopsias? Would you proceed with surgery on the right eye, exchange the IOL in the left eye, stop treatment, or use another alternative?
Uday Devgan, MD: The key here is to determine the specific dysphotopsias and the patient’s expectations. If the patient is unhappy in the immediate postoperative period and says they notice a shimmering or shaking of the IOL or even a peripheral dark crescent shadow, then I am confident the visual disturbance will resolve as healing progresses. If the patient is intolerant of the glare/halo or decreased contrast, then the best option is to delay surgery on the second eye for at least a month to give them time to adapt to their new vision. If at that time the patient still desires explantation of the IOL, then I would perform it without delay (for all of the authors’ IOL exchange pointers, see Top Tips for an IOL Exchange). If the patient is starting to adapt to the new IOL, then placing the same lens in the second eye is a reasonable choice.
Top Tips for an IOL Exchange
Uday Devgan, MD
No. 1. Use a modified twist-and-out technique,1 which allows the IOL to be explanted through an unenlarged incision with standard instruments (Figure 1; watch a related video). With a straight tying forceps and a cyclodialysis spatula, the IOL is rolled inside the anterior chamber and brought out through a standard phaco incision. Next, one haptic is brought outside the incision while the tying forceps are used to hold the edge of the optic. The spatula is then placed above the optic, and the forceps are rotated. The IOL should roll tightly and can then be pulled out of the eye.
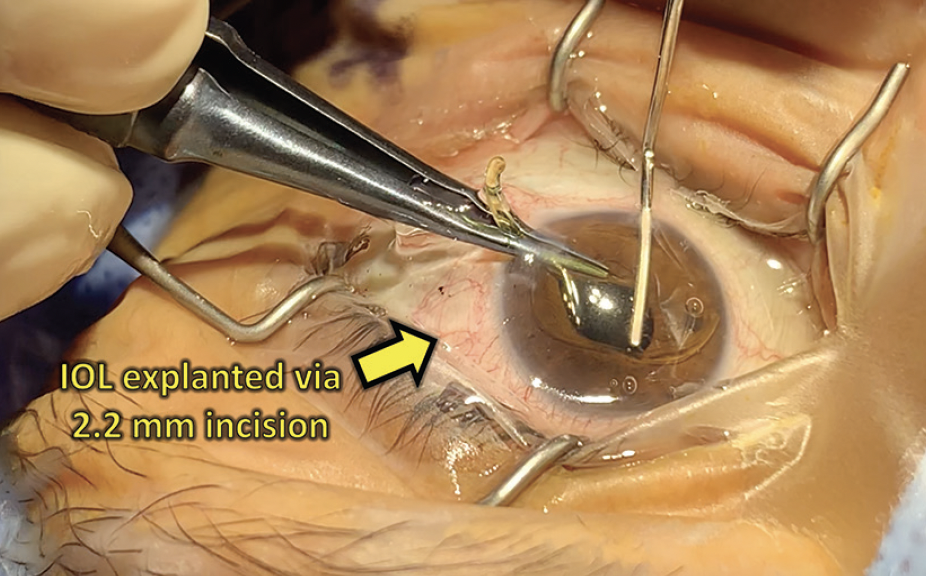
Figure 1. An IOL is explanted with standard instrumentation using the twist-and-out technique.
Courtesy of Uday Devgan, MD
Brenton Finklea, MD
No. 1. Paracentesis incisions are free. Access is a crucial component of smooth dissection and elevation of an IOL. I always make two paracenteses and often will make three for a bag-for-bag lens exchange. I usually sit in a temporal position for these cases. I create three points of access—one for the right hand, one for the left hand, and one nasally. All paracenteses are created at the beginning of the case to avoid the need to stop midsurgery because of insufficient access points.
No. 2. Evaluate the capsular bag for sufficient support and location of the IOL haptics, both of which require a dilated eye exam with multiple rounds of tropicamide and phenylephrine as needed. The exact location of the IOL to be removed and the orientation of its haptics should be documented. This allows iris hooks to be placed easily in the orientation of the haptics if dilation is insufficient in the OR. Alternatively, the initial incision should be oriented appropriately before placing a pupil expansion device.
No. 3. Always obtain consent for a vitrectomy. Most bag-for-bag exchanges are uncomplicated, but there is an increased risk of seeing vitreous compared to standard cataract surgery. Patients must be counseled appropriately.
No. 4. If a patient is referred by another physician, either obtain the surgical notes and IOL information or speak with the referring surgeon. If capsular stability was a concern, it may not make it into the surgical note. Having all information before surgery and understanding what to expect in the OR can help with counseling the patient and may guide your decision to proceed with surgery versus observe the patient.
Cathleen M. McCabe, MD
No. 1. Use a spatulated cannula such as the McCabe 25-gauge Femto Visco Paddle Cannula (Storz/Bausch + Lomb) with a dispersive OVD to separate the anterior and posterior capsular leaflets and break the fibrotic bands around the haptic.
No. 2. Identify the most likely regions for fibrosis of the haptic or lens. Initiate the inflation of the capsular bag along the axis of the haptic, and use the spatulated end of the cannula and an additional OVD injection to expand the fibrotic band while sliding the haptic out of the bag.
No. 3. Have microscissors and microforceps available. I prefer the MST Duet Handle (MicroSurgical Technology). Amputating the haptic at the haptic-optic junction can facilitate removal.
No. 4. Place a capsular tension ring after the capsular bag is inflated. If there is zonular weakness, a three-piece IOL with the optic captured in the capsular bag or even through an Nd:YAG capsulotomy is a secure way to stabilize the lens, especially with a capsular tension ring in the bag.
No. 5. An IOL exchange can be performed after an Nd:YAG capsulotomy, but the need for an anterior vitrectomy is more likely.
No. 6. Perform an intracameral injection of triamcinolone to stain the vitreous and leave a depot of steroid behind to decrease inflammation in the postoperative period.
Neda Nikpoor, MD
I spend a lot of time counseling patients before surgery because my goal is a 0% IOL exchange rate. This goal obviously is not possible, but I tell patients that part of why I spend time setting appropriate expectations before surgery is to avoid an IOL exchange. I explain to nervous patients that IOL exchanges are possible and are associated with a slightly higher risk level than cataract surgery. It often comforts them to know that their decision is not as permanent as it seems.
In general, I like to rule out all other causes of poor vision or dissatisfaction before blaming the IOL and failed neural adaptation. I have had a few cases in which an IOL exchange did not solve the patient’s problems, and it was later determined that long-forgotten mild amblyopia or cloudy vitreous was the culprit. That said, time is a factor. I prefer to exchange IOLs within 1 year of implantation and inform my patients that the risk of complications is higher after that time. Surgically speaking, I have four tips to share.
No. 1. Polish the capsule. During cataract surgery, I carefully polish the posterior and anterior capsules with a Whitman Shepherd capsule polisher whenever a diffractive IOL is implanted. Residual cortical material can make performing an IOL exchange difficult.
No. 2. Leave one-piece acrylic IOLs intact. I find that most of these IOLs can be removed easily through a 2.4- to 2.8-mm incision. I therefore no longer cut them in half. The cornea is protected with a second instrument while the IOL is twisted or folded inside the eye and pulled out whole. I have tried other techniques but find this strategy to be simple and safe. Corneas are clear the next day.
No. 3. Use the new IOL for protection when appropriate. Some IOLs such as the Light Adjustable Lens (RxSight) must be cut in half to remove. In this situation, if the anterior chamber depth is adequate, I place the new IOL in the bag or sulcus before cutting or removing the old IOL. This helps protect the posterior chamber.
No. 4. Perform viscodissection. A dispersive OVD (Viscoat, Alcon) is injected to dissect open the plane and delivered along the haptic to its end if possible. If the capsule is tightly fused to the IOL, an OVD injection from a 30-gauge needle is delivered to get under the edge. As many paracentesis incisions as necessary are made to obtain a good angle for OVD delivery. There is no reason to struggle.
William F. Wiley, MD
IOL exchange can be a daunting procedure. It can be more complicated than the original cataract surgery and often carries a higher risk profile. It is imperative to have a procedure that will deliver a sufficient outcome for the patient. I have started to use a technique that makes the exchange procedure easier to perform and allows the IOL to be removed nearly as easily as it was to insert. The technique is a modified version of the technique first described by Fukuoka and colleagues.1 Forceps are used to pull the IOL into a cartridge, allowing a reversal of IOL insertion. My tips for the method include the following (see below to watch a video demonstration):
No. 1. Free the IOL from the bag with an OVD. This helps the lens to be removed easily.
No. 2. Shorten the tail end of a Monarch A (Alcon) cartridge by removing half of the posterior IOL loading chamber (Figure 2). This allows the forceps to be passed through the entire cartridge. Then, place the cartridge into the corneal incision, which must be widened to 3 mm.
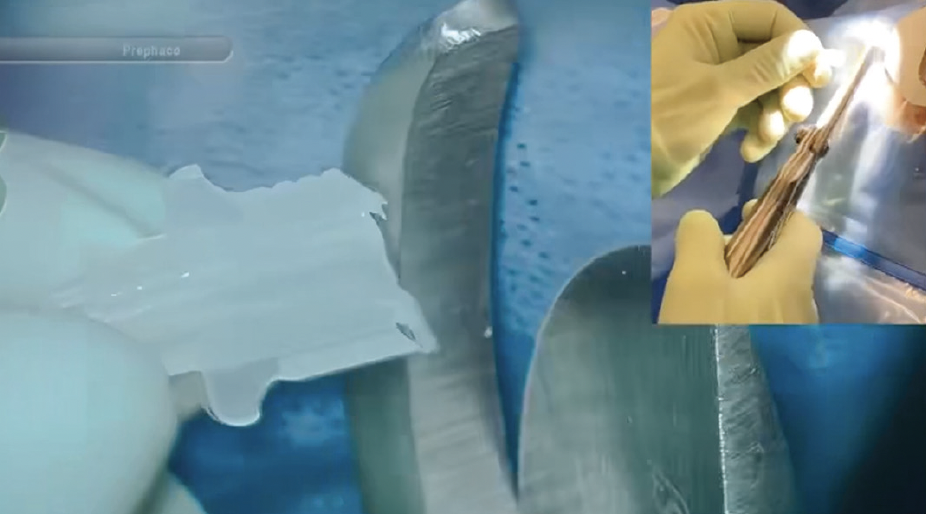
Figure 2. The tail end of the cartridge is cut.
No. 3. With a pair of ICL loading forceps (TMV181 Zaldivar-Kraff ICL Pacman Cartridge Loading Forceps, Titan Medical) inserted through the back of the cartridge into the eye, grasp the IOL just left of the IOL-haptic junction and pull the IOL into the cartridge. The IOL should fold into the cartridge in a slow, controlled, and safe manner (Figure 3).
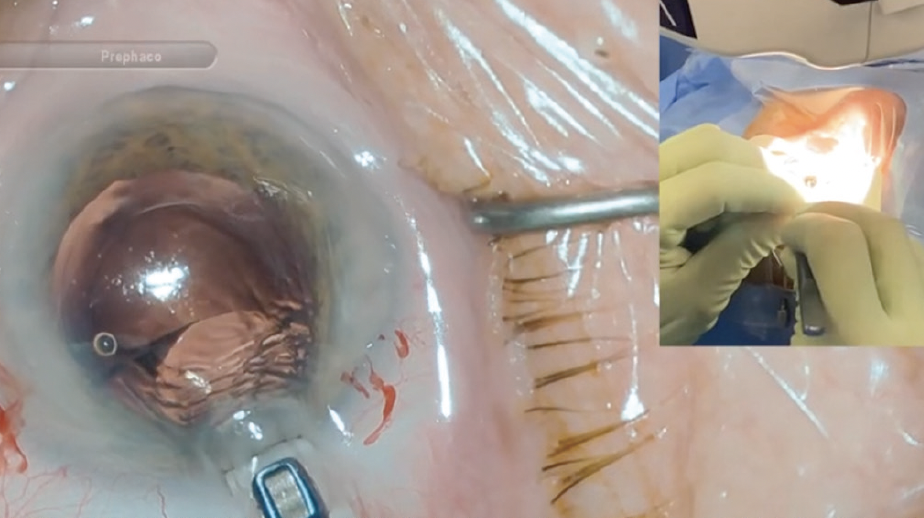
Figure 3. The IOL folds into the cartridge in a slow, controlled, and safe manner.
Figures 2 and 3 courtesy of William F. Wiley, MD
No. 4. Remove the cartridge (with the IOL) from the incision and place a new IOL in the capsular bag.
1. Fukuoka S, Kinoshita T, Morita S, Sakurai T. Intraocular lens extraction using the cartridge pull-through technique. J Cataract Refract Surg. 2021;47(12):e70-e74.
Brenton Finklea, MD: For multifocal IOLs, the decision to proceed with surgery on the second eye is often based on the quality and severity of the patient’s complaint. Those who note a mild glow or halos or slightly displeasing positive dysphotopsias are given the option to proceed with surgery on the second eye. Patients with multifocal IOLs implanted binocularly often suppress most unwanted images after a period of neural adaptation. Additionally, patients who show enthusiasm about their near vision after surgery on the first eye are encouraged to proceed with surgery on their second eye. Patients who are unhappy with the unwanted images, fixate on the negative aspects of their vision, or seem unwilling to give the IOL technology the necessary time for adaptation are encouraged to exchange the IOL for a monofocal lens before proceeding with the second eye. These individuals would be counseled on monovision options. A contact lens trial for their second eye would be performed. A Light Adjustable Lens (RxSight) with a mini-monovision strategy can achieve a good range of vision in this population.
Cathleen M. McCabe, MD: In this scenario, the first step is to assess if there are other sources of dysphotopsia such as ocular surface or dry eye disease. If present, aggressive treatment of the ocular surface with preservative-free lubricants should be initiated to help improve the patient’s image quality and decrease dysphotopsias. In my experience, posterior subcapsular cataracts are more common in younger patients and are sometimes associated with fibrosis of the posterior capsule that cannot be safely removed during cataract surgery. In this situation, an early Nd:YAG capsulotomy can improve visual acuity and resolve the dysphotopsias. Lastly, neural adaptation should help improve, minimize, or even resolve dysphotopsias.
The decision to proceed with surgery on the fellow eye with the same technology or wait for satisfactory improvement in symptoms can be difficult. Experience, intuition, careful listening, and effective communication skills are important. Some patients are convinced from the start that the technology simply is not right for them. In this situation, I would pivot to a different optical solution such as a monofocal IOL or an IOL with a nondiffractive technology (eg, extended depth of focus [EDOF] or monofocal plus) in the fellow eye. The hope would be for the patient to have fewer or no dysphotopsias in the second eye and reduced symptoms in the first eye.
I would consider an IOL exchange in two scenarios.
No. 1. When patients still have unacceptable dysphotopsias with both eyes open and is unwilling to wait for improvement.
No. 2. When resolving the symptoms in the first eye as quickly as possible is necessary for the patient to be comfortable moving forward with surgery on the second eye and they are unable or unwilling to delay intervention.
Before explanting the IOL, I would emphasize to the patient the potential for losing uncorrected near vision and demonstrate it by neutralizing some or all of the near focus with loose lenses or glasses.
Neda Nikpoor, MD: I would rule out other causes of dissatisfaction first. I would also explain neural adaptation to the patient. Presumably, they chose the implanted lens for the benefits of presbyopia correction and range of vision. I would remind the patient that these benefits will be lost if the IOL is exchanged and suggest they consider waiting. If the patient is amenable to waiting, I would consider doing so to allow neural adaptation to occur. If there is anisometropia or an urgency to remove the cataract in the second eye, the conversation might be different.
An important factor in the decision-making process is whether the IOL was implanted in the dominant or nondominant eye. (I would hope the nondominant eye was operated on first.) I would feel comfortable proceeding with surgery on the dominant eye as planned, and I would recommend a nondiffractive EDOF IOL. I would explain to the patient that they will notice a difference in the vision of the two eyes but that, if they do not cover and test each eye individually, their brain will likely adapt to the difference. This surgical strategy could give them the best of both worlds—sharp, high-quality vision in the dominant eye and a broad range of vision in the nondominant eye.
The aforementioned strategy can be risky with extremely nervous patients. Moreover, in my hands, there is a higher chance of an IOL exchange when lenses are mixed and matched. If the patient wants the IOL in the first eye to be exchanged before undergoing cataract surgery on the second eye, I would feel comfortable proceeding as they wish. Depending on the timing, however, that course of action may be premature.
William F. Wiley, MD: Multifocal IOLs are a great option for patients who want to maximize their spectacle independence. The latest trifocal IOLs can provide patients with a full range of spectacle-free vision with a side effect profile that is generally more forgiving than previous models. Occasionally, however, patients are unhappy with their multifocal vision after surgery on their first eye. In this situation, I consider the appropriate next steps carefully to ensure the best outcomes. If a patient presents with dysphotopsias, I look to see if other issues such as residual refractive error, dry eye disease, or posterior capsular opacification may be contributing to their symptoms. Often, if the residual refractive error can be neutralized with a contact lens trial, the patient’s symptoms will subside. If they do not, I suggest a wait-and-see period for the dysphotopsias to lessen through neural adaptation.
If no other contributing factors to the dysphotopsias are found and the patient continues to notice them after a sufficient time, I typically recommend considering a monofocal (or EDOF) lens for the second eye. This may help the patient tolerate the dysphotopsias in their first eye better, understand the give-and-take nature of a multifocal IOL, and appreciate the near vision and wider range of vision provided by the multifocal compared to the monofocal or EDOF IOL. In my experience, patients are likely to adapt to their vision and appreciate the different IOL styles in each eye.
CRST: How would you approach a patient who requests an upgrade from a monofocal to an advanced technology IOL via an exchange procedure?
Dr. Devgan: Every surgery has some element of risk. For any part of the body, the lowest number of surgeries is best. This certainly applies to the eye. If the patient is currently seeing well with the monofocal IOL, then the best option is to avoid going back inside the eye. LASIK can be performed, multifocal contact lenses can be used, and reading glasses are perfectly acceptable.
Most cataract patients do a before-and-after comparison of their vision. When they compare an opaque cataract to a trifocal or multifocal IOL, they typically prefer the manufacturered lens despite the splitting of the incoming light. When they compare a monofocal IOL (which has great image quality and contrast) to a multifocal or trifocal IOL (which gives more near vision at the expense of image quality and contrast), however, patients are not always pleased with the comparison. I would not perform an IOL exchange in this situation.
Dr. Finklea: An ample number of patients with early presbyopia and visually significant cataracts come to the hard realization that their near vision after monofocal IOL surgery is dependent on spectacle correction. These patients can be displeased regardless of the time and care taken by the surgeon to counsel them ahead of time. There are two main considerations for counseling patients about exchanging a monofocal IOL for a multifocal lens.
No. 1: Can it be done safely? An IOL exchange should be considered within the first few months after the initial cataract surgery. IOLs should have good 360º capsular overlap. The lens should be evaluated for centration. Additionally, opening the capsular bag completely is essential when exchanging a monofocal for a multifocal IOL to create perfect centration, particularly for a toric multifocal IOL. If several months have elapsed since the initial surgery and a toric lens is selected, the location of the haptics must be at least 45º away from the intended location of the haptics. Otherwise, adhesions near the ends of the haptics can limit complete opening of the capsular bag and result in poor centration if the haptics rest central to the adhesions.
No. 2: Should it be done? Patient counseling is paramount. All limitations of multifocal IOLs should be reviewed, and the same education and consent process that is used for cataract surgery must be applied. If the patient has an outstanding monofocal refractive outcome, I would encourage them to first do a monovision trial. A monocular exchange to a monofocal IOL has a much lower risk profile. In my experience, many patients prefer this option once they experience it.
In the end, if a patient is highly motivated, understands the risks of surgery, and still prefers a multifocal IOL, I would plan the exchange procedure with preoperative biometry or stable postoperative measurements to achieve the patient’s desired outcome.
Dr. McCabe: The answer to this question depends on several factors. How long ago was the surgery performed? Did any complications occur during or after surgery? Is there a history of trauma, refractive surgery, pseudoexfoliation, or cystoid macular edema? Did the patient experience delayed visual recovery or high IOP postoperatively? It is also important to understand what the patient is trying to achieve with the lens exchange and, if the procedure is warranted, what technology will work best and in one or both eyes.
A thorough evaluation is required. First, I would look at the capsular bag carefully. I would evaluate the centration of the current IOL; consider possible zonular pathology; check for evidence of aggressive fibrosis, phimosis, and retained cortex; evaluate the integrity of the posterior capsule; and check for signs of an Nd:YAG capsulotomy or vitreous in front of the IOL. Second, I would determine what type of IOL is currently implanted. This aids in planning the IOL exchange procedure. A one-piece acrylic IOL can be more challenging to explant than a three-piece IOL because it is usually easier to dial the latter out of the capsular bag. PMMA lenses may require a large incision. I would examine the patient to determine if their ocular health (ie, ocular surface, pupil size, macula, optic nerve, endothelium, and corneal topography) is compatible with the IOL technology that the patient desires. Lastly, I would have a frank discussion with the patient about the risks and benefits of IOL exchange surgery, including an explanation that the risks are different than those of their original surgery and the benefits more modest because the cataract has already been removed.
Dr. Nikpoor: I have experience upgrading patients’ IOLs from a monofocal to an advanced technology lens via an exchange procedure. I would feel comfortable performing the surgery in this case. If the purpose is only astigmatism correction, the best procedure would be laser vision correction (for more on laser vision correction as an alternative strategy, see “Alternative Options: When and Why?,” pg 54). If the patient wants a presbyopia-correcting IOL, an IOL exchange is the only option. In this situation, I would ensure to the extent possible that the capsular bag is intact.
The patient would be counseled extensively about the risk of a torn capsule, the possibility that the eye will have to be left aphakic, and the potential for a monofocal IOL to be implanted if the posterior capsule is violated. If the patient accepts these risks, I would offer an IOL exchange because I feel strongly that presbyopia-correcting IOLs significantly improve patients’ quality of life.
I am troubled when I encounter someone whose surgeon did not explain the available IOL options. When these patients come to me wanting an exchange, I feel a responsibility to proceed if it is safe to do so. These individuals are often grateful because other surgeons have declined to perform the procedure.
Dr. Wiley: From time to time, patients regret not investing in a multifocal IOL at the time of cataract surgery. It can be hard for patients to imagine absolute presbyopia with a monofocal IOL; until they experience it, they may not realize how it can impact their lifestyle. I offer IOL exchanges in this scenario. Managing patient expectations is crucial. They must be counseled that multifocal IOLs carry a different side effect profile than monofocal IOLs. I like to demonstrate multifocality through a bifocal contact lens trial so that the patient can see the trade-offs associated with multifocal vision. I caution them that the demonstration is not an exact representation of what they can expect. In my experience, patients who are motivated and educated on their lens choices are typically happy exchanging their monofocal IOL for a premium IOL.
1. Duncan NB, Micheletti MJ. Modified adaptation of the twist-and-out technique for intraocular lens exchange. J Cataract Refract Surg. 2022;48(12):1469-1471.