CASE PRESENTATION
A 72-year-old woman is referred for cataract surgery after consulting three other ophthalmologists about the procedure. The patient reports a reduction in vision at both distance and near and desires an improvement. She would prefer spectacle independence after surgery, but she is willing to wear correction and understands that surgery may be challenging because of her severe musculoskeletal changes, which could make positioning her in the OR difficult (Figure 1).

Figure 1. In the preoperative area just before cataract surgery, the patient is unable to extend her upper back and neck, which is angled almost 90º from the back of the bed. Her head tilts toward her left shoulder. These images show maximal extension of the patient’s upper back and neck.
Courtesy of Brandon D. Ayres, MD
The patient’s BCVA is 20/50 OD and 20/60 OS. IOP measures 18 mm Hg OU with a Tono-Pen (Medtronic). A slit-lamp examination of each eye finds a 2+ to 3+ nuclear cataract and a normal anterior segment. The pupils dilate to 7 mm. A posterior segment examination of each eye is within normal limits.
The risks and benefits of cataract surgery are discussed with the patient, who decides to proceed. Cataract surgery on the left eye is scheduled. She is aware that, if she cannot be positioned properly under the microscope, surgery will be canceled owing to safety concerns.
How would you proceed?
— Case prepared by Brandon D. Ayres, MD

SURESH K. PANDEY, MD
The challenges of performing cataract surgery in the presence of a postural disorder must be thoroughly discussed with the patient and informed consent obtained. I have had a few such cases and managed to implant a multifocal or trifocal IOL in some of them (watch below).1
My first step in the current situation would be to conduct a mock drill with my OR team. The exercise would help us determine the best possible positioning of the patient on the bed, the operating microscope, and the surgeon stool. The foot end of the bed would be raised, and the patient’s head and neck would be supported with a pillow to make her comfortable. While sitting on the surgeon’s stool, I would tilt the microscope handpiece. The goal would be to maintain patient safety while attempting to keep her and myself comfortable.
After being cleaned with 5% povidone-iodine, the left eye would be prepped and covered with sterile plastic drapes. I am left-handed and would make a clear corneal incision in the inferotemporal area.
Topical (and intracameral) anesthesia would be my preference. An intracameral injection of a fixed combination of 1% lignocaine, 0.1% phenylephrine, and 0.02% tropicamide (Phenocaine Plus, Entod Pharmaceuticals) would be performed to provide anesthesia and maintain pupillary dilatation during the cataract procedure. A dispersive OVD (Viscoat, Alcon) would be instilled to protect the corneal endothelium.
A 5-mm capsulorhexis would be performed followed by hydrodissection, nuclear emulsification, and cortical cleanup with bimanual irrigation and aspiration. Next, a foldable monofocal IOL would be implanted. The OVD would be removed from the capsular bag and anterior chamber, and the clear corneal incision(s) would be sealed. After the sideport and main incisions are closed, an intracameral injection of 0.1 mL of moxifloxacin would be performed, and one drop of 5% povidone-iodine would be instilled.

JONATHAN B. RUBENSTEIN, MD
The dilemma presented is uncommon but not unheard of. Neck and back disease has produced profound kyphosis that prohibits the patient from lying flat in the position usually required for cataract surgery. Fortunately, the cataracts themselves do not present a particular challenge. Each eye has 2+ to 3+ nuclear sclerosis, a well-dilating pupil, and a normal anterior segment.
Two pieces of equipment might make cataract surgery easier:
No. 1: A special bed that allows for Trendelenburg positioning; and
No. 2: A heads-up display microscope.
The patient must be positioned such that her head is as horizontal as possible. This demands an exaggerated Trendelenburg position. Her head must be positioned below her feet, and her head flexion requires support from an articulated headpiece, blankets, and cushions. To maintain this position, her body must be secured. The patient’s legs, arms, torso, and head must be strapped firmly to the bed to keep her from sliding off. This type of surgical positioning is often used in pelvic and abdominal procedures, and special beds have been designed for surgery on a patient in this position (Figure 2). Unfortunately, Trendelenburg positioning decreases the space under the table available for the surgeon to operate the pedals. The use of a heads-up 3D microscope such as the Ngenuity 3D Visualization System (Alcon) or the Artevo 800 (Carl Zeiss Meditec) can give surgeons more positioning flexibility. They do not have to sit up as high to reach the oculars of a conventional microscope. Moreover, although their hands still must reach the operative field, positioning their legs under the table is easier (Figure 3).

Figure 2. A bed designed for Trendelenburg positioning of the patient.
Figures 2 and 3 courtesy of Jonathan B. Rubenstein, MD
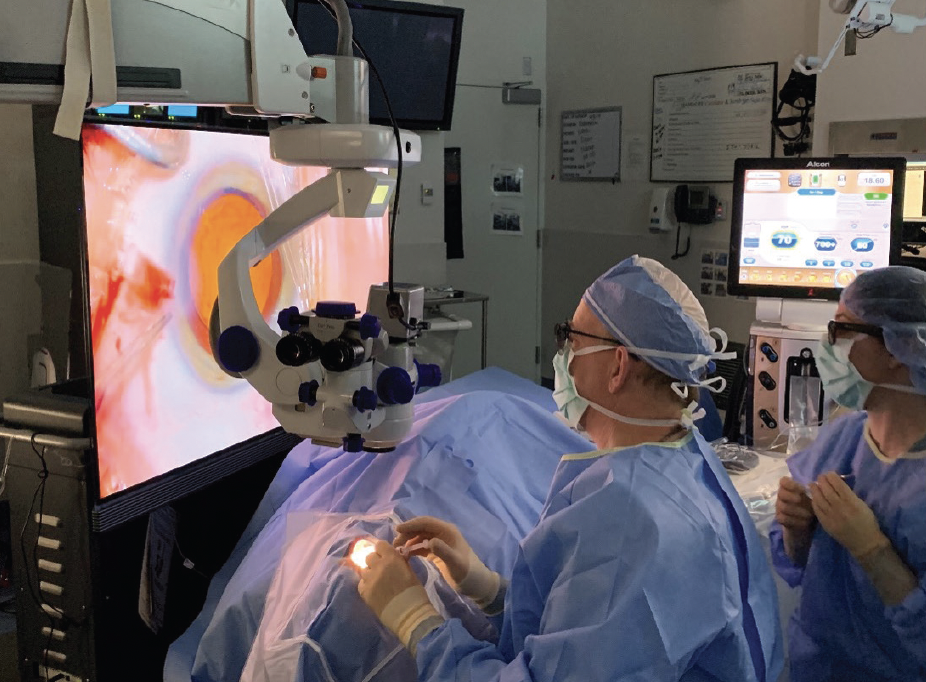
Figure 3. Using a 3D heads-up display instead of a traditional microscope can allow more flexibility in surgeon positioning.

WHAT I DID: BRANDON D. AYRES, MD
During the preoperative consultation, the patient, her family, and I had a long and candid discussion about the challenge of positioning her at the surgical microscope and the traditional risks and benefits of cataract surgery. Of particular concern was that, should one occur, a surgical complication would be more difficult to manage than usual. We decided that measurements such as biometry would be performed in the OR on the day of the cataract procedure but that, if positioning the patient proved too difficult, surgery would be cancelled.
In the OR, the back of the bed was brought to its maximum height, and the head of the bed was lowered to account for the patient’s inability to extend her neck. The head of the bed could be lowered only so much, however, or the patient would have slid off. The position was tested and found to be adequate for surgical exposure, but it made it impossible for me to sit for the surgery or to stand comfortably. The oculars were repositioned, and the traditional 175-mm objective lens was exchanged for a 200-mm lens. These changes allowed surgery to proceed (Figure 4).

Figure 4. Adequate surgical positioning was achieved before proceeding. Note the downhill positioning of the bed. With the addition of a 200-mm microscope lens and Dr. Ayres’ slightly awkward standing position, it was deemed safe to proceed with the operation.
Figures 4–7 courtesy of Brandon D. Ayres, MD
Keratometry, immersion A-scan ultrasound, and IOL calculations were performed in the OR (Figure 5). The patient desired optimal distance correction. Cataract surgery began (watch below). The only change made to my typical cataract protocol was my standing position during surgery. An assistant surgeon held the patient’s head in position, which was extremely helpful. One of the greatest surgical challenges encountered was my inability to control the microscope and phaco machine simultaneously. On some microscope platforms, the hand grips can be custom programmed, allowing focus to be controlled by the surgeon’s left hand while the right hand holds the phaco handpiece, which might have made performing surgery slightly more comfortable. Another issue was that the constant leftward tilt of the patient’s neck caused balanced salt solution to pool in the nasal orbit (Figures 6 and 7).

Figure 5. Auto keratometry and immersion A-scan ultrasound were performed in the OR, after which the IOL calculation was performed.

Figure 6. In essence, the patient stood on her head to compensate for her inability to extend her neck and back.

Figure 7. Mounting of the camera on the bed rail disguises the OR table’s severe head-down position and elevation. The patient’s extreme Trendelenburg position required Dr. Ayres to stand during surgery. The leftward tilt of the patient’s head caused balanced salt solution to pool in the nasal orbit. The assistant surgeon wicked away the fluid to prevent distortion of the surgical field.
Postoperatively, the patient was happy with her uncorrected distance visual acuity of 20/40 OS. Surgery on the right eye was scheduled and performed in a similar fashion. Her postoperative UCVA was 20/30 OD.
Complex cataract surgery involves more than intraocular challenges. The complexity of this case related not to the eye itself but to surgical planning and patient positioning (to read another article on surgical positioning for patients with physical disabilities, see “Physically Disabled Patients," pg 40). With a little creativity and flexibility with regard to my own positioning, cataract surgery was completed with no complications other than my slight, transient backache. What do we do if the patient develops posterior capsular opacification?
1. Pandey SK, Sharma V. Phacoemulsification in postural disorders. Cataract & Refractive Surgery Today. April 2016. Accessed June 9, 2023. https://crstoday.com/articles/2016-apr/phacoemulsification-in-postural-disorders