

Cataract surgery can be enormously beneficial for people with neurodiversity including dementia, Down syndrome, autism spectrum disorder, and cerebral palsy. Although many ophthalmologists assume that these individuals are poor surgical candidates due to greater risk for less benefit, there is little published data to support this conclusion. The perception that neurodiverse people are poor candidates for surgery leads to unnecessary suffering because vision loss from cataracts has a vital impact on health, happiness, and cognitive function.
At Boston Medical Center, where we practice, more than 250 cataract surgeries under general anesthesia have been performed on people with special needs over the past 15 years (see Case Example). This article shares several simple procedural and surgical modifications based on our experience. Adopting these strategies is not difficult, but it does require commitment and advance planning. Our hope is that the information provided here helps reduce unnecessary barriers to cataract surgery for people who cannot advocate for themselves but who can greatly benefit from improved vision (see Vision Loss and Dementia Risk).
CASE EXAMPLE
A 52-year-old nonverbal man with autism and an intellectual disability presented for an ophthalmic evaluation. According to his group home caregiver, the patient had become increasingly listless and uninterested in group activities during the past 2 years. A year ago, he had visited another ophthalmologist who suspected cataracts and suggested surgery. Because of concern about the patient’s inability to tolerate postoperative drops and keep his hands away from his eyes, however, he was deemed a poor candidate for surgery.
Recently, caregivers had noticed that the patient wanted only to sit alone in his room. They described his frustrated outbursts and increased sadness. The past time his sister visited, he had not recognized or responded to her. The caregivers wondered if the observed changes could be due to his vision.
The patient underwent cataract surgery on the left eye. He removed the eye shield in the post anesthesia care unit. After a brief episode of eye rubbing, he began to look around. He was sent home with topical antibiotics and an eye shield.
At the postoperative visit, caregivers reported that the patient was walking independently and put a plate in the dishwasher for the first time in 2 years. Fleeting penlight views revealed a clear cornea, deep anterior chamber, and a small, round pupil. At subsequent visits, caregivers reported that the patient had been observed exploring his house with confidence and laughing and smiling again. Cataract surgery for the right eye was scheduled.
VISION LOSS AND DEMENTIA RISK
A study of French patients with Alzheimer disease showed that cataract surgery, unlike glaucoma surgery, reduced the risk of dementia development.1 A prospective cohort study monitored and assessed 2,927 adults without dementia who were 65 years of age or older for 8 years. The investigators found that the risk of dementia development was 1.23 times higher among the individuals with vision impairment compared to those with no sensory impairment.2
A cross-sectional cohort study of 16,690 individuals participating in the University of Michigan Health and Retirement Study found that vision impairment was associated with 1.8% of dementia cases.3 Both cohort studies2,3 identified vision loss as a preventable risk factor for dementia, with the potential to slow or prevent cognitive decline.
1. Lee CS, Gibbons LE, Lee AY, et al. Association between cataract extraction and development of dementia. JAMA Intern Med. 2022;182(2):134-141.
2. Hwang PH, Longstreth WT Jr, Thielke SM, et al. Longitudinal changes in hearing and visual impairments and risk of dementia in older adults in the United States. JAMA Netw Open. 2022;5(5):e2210734.
3. Ehrlich JR, Goldstein J, Swenor BK, Whitson H, Langa KM, Veliz P. Addition of vision impairment to a life-course model of potentially modifiable dementia risk factors in the US. JAMA Neurol. 2022;79(6):623-626.
TIP NO. 1: RELY ON THE HISTORY
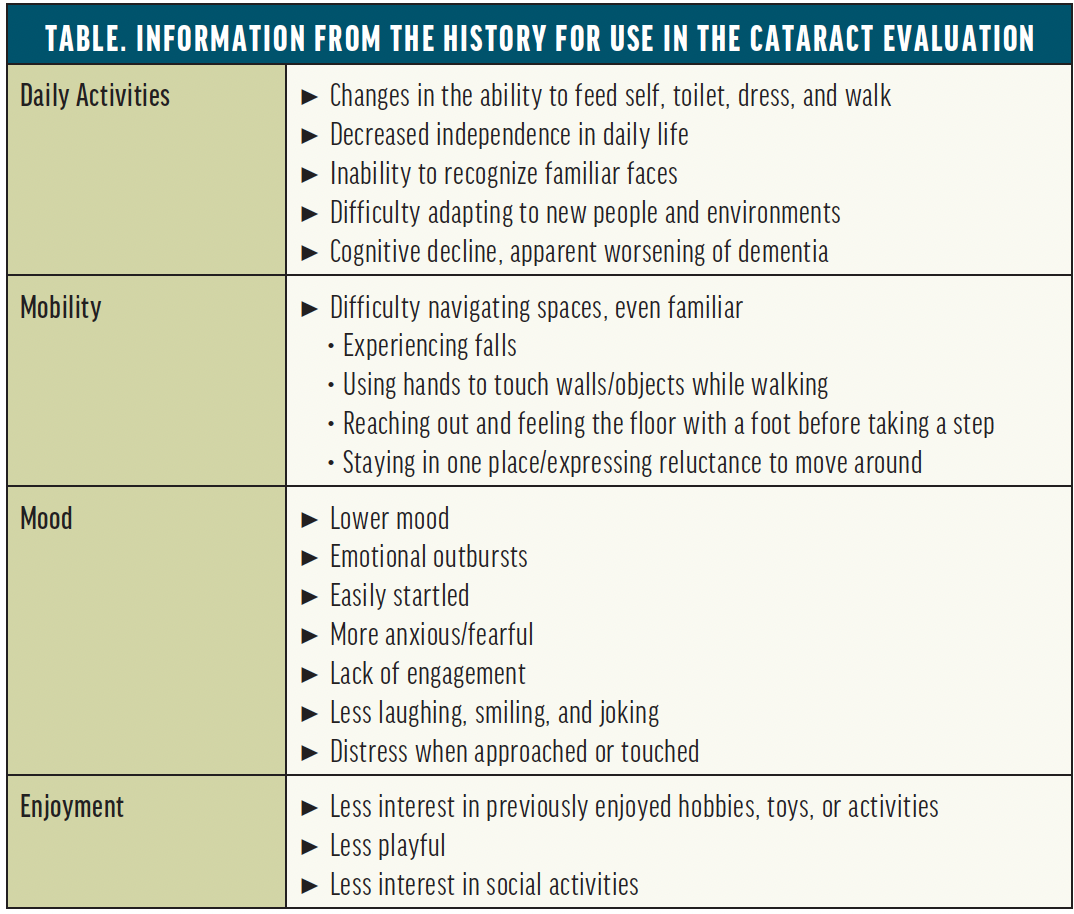
An eye examination can be challenging for neurodiverse patients owing to sensory processing challenges, lack of comprehension, or anxiety due to previous medical trauma. A careful history usually provides enough information to determine whether cataracts are the likely reason for vision loss. An ocular history, focused on recent changes, can establish a baseline for precataract visual potential (Table).
The primary goal is to determine whether an examination under anesthesia (EUA) is indicated. Elements of a standard eye examination may be performed as tolerated. We have found it best to defer any part that is stressful until the patient has been anesthetized.
TIP NO. 2: OBTAIN SURGICAL CONSENT FOR BOTH EYES
We rarely perform immediate sequential bilateral cataract surgery. We obtain surgical consent for an EUA and surgery on both eyes, however, to provide flexibility once an examination is completed in the OR. We find it helpful to include caregivers in the consent process—even if they are not legal guardians—because they often have questions regarding postoperative care.
TIP NO. 3: CONSIDER MYOPIC MINI-MONOVISION
The target refraction is determined with the help of the patient’s caregivers based on which activities are most important. Many people with special needs are unable to tolerate eyeglasses. A mini-monovision strategy with a slightly myopic aim (-0.50 and -1.25 D) can allow them to see across the room and right in front of them.
TIP NO. 4: MINIMIZE DISTRESS IN THE PREOPERATIVE HOLDING AREA
This can be accomplished with patience and gentle redirection. Caring for people with special needs may require modifications to protocol, which can be stressful for the care team unless they know what to expect and have a plan for how to proceed. The anesthesia and preoperative teams may need to complete preoperative testing and telephone consent before the day of surgery. Pediatric anesthesia may be consulted for complex cases.
Pretreatment with oral anxiolytics before the patient leaves home can greatly reduce anxiety. A quiet preoperative space can also be beneficial. A trusted staff or family member can help the patient remain calm and interpret communications if they are nonverbal.
Many neurodivergent individuals object to the removal of clothing and placement of an intravenous unit and monitors. The intramuscular administration of ketamine can be helpful in this situation. Occasionally, people may require sedation with inhalant anesthesia in the OR before intravenous therapy is initiated.
TIP NO. 5: PERFORM A COMPLETE EXAMINATION DURING THE EUA
In addition to general anesthesia, a topical anesthetic is administered for analgesia to minimize the systemic anesthetic load. A retro- or peribulbar block should be avoided owing to the risk of postoperative injury. A complete ophthalmologic examination, including autorefraction, keratometry, optical biometry, and B-scan ultrasonography if indicated, is performed. An IOL is selected from a standing inventory.
TIP NO. 6: PREPARE FOR COMPLEX SURGERY
The surgical technique is standard, but it is wise to prepare for complex surgery because advanced cataracts are common in this population owing to delayed care. Phacodonesis may be present because of the increased risk of trauma. Intracameral mydriatics can reduce the risk of iris prolapse. Intracameral antibiotics and a sub-Tenon injection of triamcinolone acetonide can minimize the need for topical drops postoperatively.
TIP NO. 7: PAY CLOSE ATTENTION TO WOUND CLOSURE
A sutureless approach minimizes ocular irritation and the likelihood that patients will rub their eye. Strong, reliable wound closure is essential, however, because many neurodivergent people find it difficult or impossible to tolerate an eye shield.
Most clear corneal incisions close securely after 10 seconds of gentle pressure with a Wek-Cel sponge (BVI Medical) on the corneal side of the wound. Applying a tetracaine-soaked Wek-Cel sponge to the wound for 10 seconds can enhance wound stability. We leave the eye soft (< 10 mm Hg to palpation). A rigorous Seidel test with provocation—using as much pressure as a patient might apply with vigorous rubbing—can establish wound integrity. Rarely, placement of a 10-0 nylon suture is required to prevent leakage.
TIP NO. 8: THE SHIELD WILL PROBABLY COME OFF
As people recover from general anesthesia and discover that they can see, they often remove the shield and rub the eye. They are permitted to do so after hand hygiene is performed. Individuals who self-stimulate through eye rubbing may do so, but we often find that this behavior lessens once their vision has been restored.
TIP NO. 9: TAKE A MINIMALIST APPROACH TO POSTOPERATIVE MANAGEMENT
Postoperative visits focus on visual function, pain management, and caregiver questions. If possible, a brief penlight examination is conducted to assess wound integrity, the shape of the pupil, and anterior chamber depth. An eye shield is not used if it cannot be tolerated by the patient. If they cannot tolerate eye drops, caregivers can apply antibiotic/steroid ointment or the equivalent twice a day while the patient sleeps. If a patient rubs their eye, caregivers perform hand hygiene four times per day as well as after meals and toileting.
The postoperative visit schedule is decided on a case-by-case basis. Refraction and dilation are often deferred until the EUA for second eye surgery because the yield for treatable findings is low. If an examination in the office is impossible, a final EUA after the second eye surgery is performed as needed.
CONCLUSION
Many of the neurodivergent people we have cared for developed severe vision loss years before they presented to our practice. Many sought care from multiple surgeons who felt unable to provide safe, high-quality cataract surgery. We hope this article empowers and inspires our colleagues to offer this safe treatment that can dramatically improve quality of life, support joy and independence, and reduce risks of injury and dementia.
1. Pershing S, Henderson VW, Goldstein MK, et al. Cataract surgery complexity and surgical complication rates among Medicare beneficiaries with and without dementia. Am J Ophthalmol. 2021;221:27-38.




